Abstract
Background
An essential contribution regarding the prevention of thromboembolic events in patients with (non-valvular) atrial fibrillation (AF) is good adherence to direct oral anticoagulants (DOACs). However, it is an open question what “good” adherence means for DOACs or below which threshold non-adherence is clinically relevant for AF patients. Ultimately, such a classification could prevent strokes and associated costs through adjusted treatment regimens or supportive measures.
Methods
We selected 10,092 AF patients from health insurance claims data between 2014 and 2018 who were issued a majority (at least half of the number) of maximum approved strength prescriptions of one of the following DOACs, namely rivaroxaban, apixaban, or dabigatran. Due to the limited sample size, the prescriptions of dabigatran had to be finally excluded for the cut-off analysis. DOAC adherence was calculated as the proportion of days covered (PDC) by dividing the days of theoretical use (days covered) of the drug by the duration in days of the observation interval. PDC cut-off values were derived from stroke risk as a function of continuous PDC values in time-to-event analyses and corresponding dose-response models. The influence of adherence-promoting interventions (targeted and untargeted) on the occurrence of strokes and related costs was then projected, considering intervention costs per patient.
Results
The population had a mean age of 74.5 years and 50% were female. The median PDC was 0.79 ± 0.28 with a median follow-up time of 1218 days, in which 2% of all DOAC patients had a stroke. The adherence cut-offs for good adherence were identified at 0.78 for rivaroxaban and 0.8 for apixaban. Targeted interventions appeared to be far more cost-effective than untargeted interventions.
Conclusion
Clear adherence cut-offs enable healthcare professionals to identify patients with clinically relevant non-adherence. Interventions based on these cut-offs appear to be a promising means to optimize DOAC treatment.
Introduction
Adherence is a necessary prerequisite for a drug to work, either prophylactically, therapeutically, or palliatively.Citation1–Citation3 This is also true for direct oral anticoagulants (DOACs), which aim to prevent serious medical consequences such as thromboembolic events in patients with (non-valvular) atrial fibrillation (AF).Citation1,Citation4,Citation5 Adherence is a continuum and achieving and consistently maintaining 100% adherence over a long period of time is difficult. Indeed, the cost of keeping adherence rates high increases with the level of intended adherence.Citation6 Therefore, the obvious question is how much adherence is necessary and how much is enough? Often, general cut-off values that define “good“ adherence have been arbitrarily and conventionally set at 80%.Citation5,Citation7–Citation10 However, this is unlikely to be true for all medicines and may not apply to DOACs. Sufficient adherence may be a critical factor in clinical practice, depending on the expected benefits of the medicine and the consequences of underuse. A drug-specific adherence cut-off for DOACs may help to classify patients at substantially higher risk and to offer supportive interventions.
Medication adherence can be readily estimated from routine claims data that contain information on drug purchases and dispensed package sizes and thus allow investigating the relationship between adherence, clinical outcomes, and associated costs.Citation1–Citation3 In addition to a continuous adherence metric, the use of adherence thresholds is common, dividing patients into “good” and “poor” adherence groups by a cut-off, which can help clinicians to identify patients in need of support.Citation2,Citation11,Citation12 Such adherence cut-off values can be established by relating them to clinical outcomes. Taking binary outcome definitions as an example, one can maximize their sensitivity and specificity, and for time-to-event analyses, one can maximize the test statistic for the group comparison between “high” and “low” adherence, separated by a cut-off value.Citation2,Citation11,Citation12 Because the effect of DOACs on clinical endpoints is concentration-dependent as well as dose-dependent (and non-adherence is in fact a dose reduction), a pharmacologically more intuitive approach would be to apply (sigmoid) dose-response analyses to choose a cut-off value and to thus achieve a certain percentage of maximum effect. Regardless of the method chosen, the adherence model allows to project the impact of adherence-increasing interventions on the number of (averted) clinical outcomes and thus equally addresses health economic aspects.Citation5 Given the disastrous clinical consequences of strokesCitation13,Citation14 and the immense costs associated with them,Citation15–Citation17 it seems imperative to define an adherence threshold that identifies patients at risk of treatment failure while considering the potential benefits in terms of averted events and costs.
In this study, we explored claims data from a large German statutory health insurance fund to determine adherence cut-offs for the DOACs rivaroxaban and apixaban in AF patients; the data were generated as a preparatory step for the evaluation of the ARMIN (“Arzneimittelinitiative Sachsen-Thüringen”) program, a quality initiative to improve medication quality and safety. Therefore, we analyzed the association between continuous adherence and stroke risk as a dose-response relationship to derive clinically meaningful adherence cut-offs for optimum stroke risk reduction after DOAC initiation. A secondary aim was to compare adherence patterns and cut-offs of DOACs with different dosing schedules, such as once-daily regimens for rivaroxaban and twice-daily for apixaban. Finally, we predicted the potential impact of supportive interventions on avoided events as a function of adherence cut-off values.
Materials and Methods
Data Source and Study Population
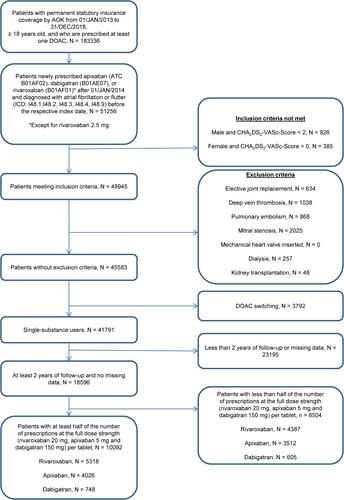
The study’s data source was constituted of claims data of insured persons belonging to a large German health insurance fund (AOK PLUS) in the calendar years 2013–2018. Insured persons were included in the follow-up period between 2014 and 2018 if they received at least one DOAC prescription (rivaroxaban, apixaban, or dabigatran) between 01/JAN/2014 and 31/DEC/2018, were permanently insured in the period from 01/JAN/2013 to 31/DEC/2018, and at least 18 years old in 2013. Thus, the year 2013 served as a run-in period to characterize the population at baseline and ensured that each patient was characterized for at least 12 months prior to individual follow-up. describes the inclusion and exclusion criteria used to form the study population (for a detailed description of underlying billing codes, see Supplementary Table 1). Accordingly, the study applied a retrospective cohort design considering DOAC initiation as individual entry time. We chose a new-user design (also called incident-user design) as study design, meaning that only patients who had not received a DOAC prescription in the year prior to individual study entry (ie, the time of the “first” prescription) were included in the study. Inclusion was restricted to patients with a majority of full-dose prescriptions in order to avoid inclusion of patients who were falsely underdosed, a common phenomenon in clinical practice associated with an increased risk of stroke.Citation18–Citation21 Hence, the study exclusively considered patients who received at least half of the number (or the same number) of prescriptions with the full dose strength (rivaroxaban 20 mg, apixaban 5 mg, and dabigatran 150 mg) per tablet. This also avoided the consideration of renal function, which cannot be validly extracted from (outpatient and inpatient) claims data and can be a reason for dose reduction. Patients were followed up to the first clinical event (stroke), or to a censoring event. This could be either death, switching to a vitamin K antagonist, or end of follow-up. Because all data were completely anonymous to the analysts, this research project did not require ethical approval. All analyses strictly followed the STROBE statement (Strengthening the Reporting of Observational studies in Epidemiology, see Supplementary Table 3).Citation22
Figure 1 Selection of a patient cohort suffering from atrial fibrillation that are anticoagulated with direct oral anticoagulants as documented in a large health insurance database.
Outcome
To identify patients with stroke as an outcome, validated and previously applied code sets of the main and secondary diagnoses of inpatient admissions were used (for a detailed list of codes, see Supplementary Table 2).Citation23,Citation24
Exposure
The exposure variable was defined by DOAC adherence, which was obtained by a form of proportion of days covered (PDC). The PDC is a numeric proportion between 0 and 1 that is calculated by dividing the days of theoretical use (number of days covered by medication) by the number of (outpatient) days in the follow-up window.Citation25 Formula 1 below describes how the PDC is calculated:
The algorithm used (CMA6 function from the AdhereR packageCitation25) first determines the number of days without medication (the so-called gap days are derived from the prescription durations of the packs) in the follow-up period. In the next step, these are subtracted from the total number of days in the follow-up period to determine the number of days with theoretical use. DOAC prescription records were used to determine the date of prescription and the quantity and strength of tablets prescribed. From this, a prescription duration was determined for each pack based on the patient’s dose. According to patient selection, the usual doses of 10 mg per day for apixaban, 20 mg per day for rivaroxaban, and 300 mg per day for dabigatran were assumed. The prescription duration (PD) was calculated for each pack according to formula 2:
Quantity denotes quantity of tablets per package, Number corresponds to the number of packages prescribed, Strength denotes the amount of active ingredient of one solid oral dosage form of the package and Dose denotes the standard dose (full-dose) per day of the corresponding DOAC. If patients were hospitalized within the prescription duration of a package, the length of the hospital stay was added to the prescription duration of the package because during hospitalization, provision of all drugs by the hospital is mandatory. PDC was calculated using the R package AdhereR as an averaged value over a patient’s entire observation period (see Supplementary Material 1 for functional parameters).Citation25
Potential Confounders
Potential confounding variables were defined by clinical expertise considering 18 variables as extracted from prior publications.Citation4 These variables originated from different areas such as demographics (sex and age), comorbidities (hypertension, heart failure, diabetes mellitus, prior stroke, prior myocardial infarction, renal disease, chronic liver disease, peripheral vascular disease, depression, alcohol abuse, and drug abuse), scores for individual prognosis (CHA2DS2-VASc Score for thromboembolic events),Citation26 comedication (use of antiplatelets or vitamin K antagonist), and healthcare utilization (number of hospitalizations and number of medications co-prescribed). We assessed which of the individual conditions mentioned in the Charlson and Elixhauser scores were predictors of non-adherence and used these to adjust the model.Citation27,Citation28 Overall, their covariates were derived from the prescription data, the medically-confirmed outpatient diagnoses by the general practitioner, the hospital admission diagnoses, and the main diagnoses of hospital stays in the year before the patient’s index date.Citation4 A complete list of potential confounders and their definitions is provided in Supplementary Table 4.
Sample Size
With our study design, the total number of patients for all three DOAC cohorts was 10,092 (). Of these, 4026 patients (39.9%) were treated with apixaban and 5318 patients (52.7%) with rivaroxaban. Only rivaroxaban initiators and apixaban initiators were used for adherence-response modeling, while the cohort of 748 (7.4%) dabigatran initiators was too limited for either statistical inferences or modeling and was thus only used for an exploratory comparison with an external reference.Citation4 Because enrollment was restricted to patients with complete data sets, no values were missing.
Statistical Analyses
The cohort was described by statistics summarizing their distributional location parameters for continuous and proportions for categorical variables. Inferential tests on descriptive characteristics of the study population were chosen in accordance with the variable scale and variable distribution.
Association of DOAC Adherence with Stroke
To describe the association between DOAC adherence and stroke risk, we adopted the procedure proposed by Shore et al.Citation4 Cox proportional hazards regressionCitation4 was applied to all three DOAC cohorts in order to analyze event times for each patient starting at the index date and ending with the event of stroke or censoring time due to premature death, switching to a vitamin K antagonist, or end of follow-up (31/DEC/2018). In addition to the list of potential confounders, the continuous adherence measure of each patient was chosen as independent variable of interest. To facilitate a comparison with the external reference by Shore and colleagues, hazard ratios (HR) with 95% confidence intervals (CI) were determined for each 10% decrease in adherence to the respective DOAC regimen.Citation4 The fully adjusted Cox models were also used for a general group comparison between rivaroxaban and apixaban. In a further analysis, the stroke event frequency of the study population was compared with a population that switched between the different DOAC agents.
Adherence Cut-off Estimation
To analyze the dose-response relationship and derive an adherence cut-off, we applied the time-to-event approach with continuous PDC estimates in Cox proportional hazards models for stroke risk.Citation29 As a preliminary step, non-linearity in the effects of apixaban and rivaroxaban was ruled out by inferential tests based on model comparisons with multifractional polynomials.Citation30 Because empirically no evidence for non-linearity was present, we applied linear Cox models of adherence to predict probabilities of stroke and used them as the (continuous) dependent variable in dose-response analyses with adherence as the independent variable. In particular, 4-fold logistic (growth) models were used to derive a cut-off value from the common effective dose exerting 80% of the maximum effect (ie, ED80 value corresponding to the estimated PDC inducing 80% of the maximum effect).Citation31 In these models, the effect sizes (hazard ratios) were scaled to 100% by dividing each value by the maximum value (ie, estimate at the point of zero adherence). Sensitivity analyses included a cut-off determination based on the Youden index to maximize sensitivity and specificityCitation32 and a derivation of the cut-off from the receiver operating characteristic (ROC) curve as the point with the smallest distance from the upper left corner (0/1).Citation11
Impact of Supportive Interventions on Averted Events
We considered two settings to examine the impact of adherence-increasing interventions on stroke incidence. In the first setting, we considered offering a complex adherence-increasing intervention to the entire study population regardless of the adherence score of the individual patient (untargeted intervention), whereas the second setting foresaw a targeted adherence-increasing intervention for the group below the previously determined cut-off value. Untargeted and targeted interventions differ in whether all patients participate in the intervention or only a predefined (eg, presumably poorly adherent) proportion of patients. Possible interventions for both groups include a mobile app or phone calls that remind patients to take their anticoagulant. Other possibilities are patient education about the value of good adherence and ways to reach adherence rates ≥ 80% or refill activities to promote uninterrupted drug supply.Citation33–Citation36 To consider the interventional impact independently from our modeling data, we chose a DOAC adherence distribution from an external reference.Citation4 The assumed effect estimate for the untargeted intervention in the first setting was adopted from unpublished data as an odds ratio of 1.08 for an increased probability for adherence improvement by a complex intervention. We applied formula 3:
where ORAI denotes the odds ratio for adherence improvement. First, baseline adherence (PDC) from the reference distribution was randomly assigned to our patients in order to predict the baseline number of strokes from the aforementioned adjusted Cox models. Second, improved adherence (PDC*) was derived from the formula to predict the number of strokes after an intervention. This procedure was repeated a thousand times and median numbers of strokes across iterations were extracted to calculate the number of avoided events.
The assumed effect estimates for the targeted intervention in the second setting related to probabilities for improving a patient’s adherence to a value above the cut-off yielding 80% efficacy. We considered the meta-analytically pooled odds ratio of 1.57 for achieving “good” adherence.Citation37 First, each patient was randomly assigned an adherence according to the reference distribution. Then, we randomly sampled 57% of the patients below the cut-off, assigned the cut-off value to their adherence estimate, and predicted the number of events depending on the new adherence values. This procedure was repeated a thousand times to obtain a median number of avoided events across all iterations. Finally, we averaged the number of averted events across all samples. For both types of intervention, we then calculated the costs that could be saved with each intervention through reduced events. Costs of 43,129 Euros were assumed for each case of stroke.Citation17
In general, statistical tests were two-sided, and 95% CI were calculated according to an alpha level of 0.05. All analyses were conducted using the R software environment in version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Study Population
shows the baseline characteristics of the three cohorts selected by our inclusion and exclusion criteria. The mean age of the 10,092 eligible patients was 74.5 ± 9.7 years and 50% were female. During follow-up, 210 (2% of all patients) strokes were recorded with a median follow-up time of 1218 days (). The median CHA2DS2-VASc Score of the study population was 4. Comorbidities were frequent, with nearly all patients being diagnosed for hypertension (95%) and nearly half of the patients being diagnosed for heart failure (53%), and diabetes (46%). Antiplatelets were used by 18% of patients and 30% of patients had a prescription for a vitamin K antagonist in the year before the first DOAC prescription. Apixaban patients were older than patients receiving rivaroxaban. They had shorter median times to stroke, on average more comorbidities, and were more frequently prescribed antiplatelets or anticoagulants before participating in the study. They equally had higher CHA2DS2-VASc scores. A detailed presentation of the cohort subdivided into age groups can be found in Supplementary Tables 6 and 7.
Table 1 Baseline Characteristics of the Study Cohorts
Association of DOAC Adherence and Stroke
In our study cohorts mean adherence (PDC) during follow-up was 0.79 ± 0.28 in total, while highest PDC was observed for apixaban users (0.81 ± 0.27) followed by rivaroxaban (0.80 ± 0.29) and dabigatran users (0.70 ± 0.33). Adherence distributions were quite similar between different DOACs and dosing regimens (). A 10% reduction in adherence was associated with a 2% increase in stroke risk in the dabigatran cohort (adjusted HR 1.02, 95% CI [0.9–1.15]), a 5% increase of the rivaroxaban cohort (adjusted HR 1.05, 95% CI [0.98–1.12]), and a 3% increase in the apixaban cohort (adjusted HR 1.03 95% CI [0.95–1.11]). In a sensitivity analysis, the stroke incidence of patients who were a priori excluded because they switched between DOACs (n = 3792) was substantially greater (12.5%) than in our main study population, where patients did not switch between DOACs (1.9%). Moreover, in patients who switched twice (n = 106), stroke rate was 18.9%, ie, 50% larger than in patients switching only once (12.3%). In the follow-up period, 94 patients (1% of all enrolled patients) switched to a vitamin K antagonist.
Figure 2 Adherence cut-off estimation of apixaban and rivaroxaban with Cox models (A and C) and 4-parameter logistic dose-response models (B and D).
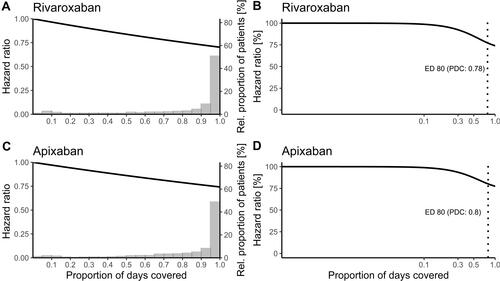
Adherence Cut-off Estimation
Using our study design the determined adherence cut-offs for 80% efficacy (ED80) were 0.78 for rivaroxaban and 0.8 for apixaban ( and ; other estimated doses and the corresponding PDC values can be found in Supplementary Table 5). Alternative methods in sensitivity analyses yielded an optimal cut-off for rivaroxaban of 0.84 and 0.94 (determined by the Youden index/ROC 0/1 method) and an optimal cut-off for apixaban of 0.83 and 0.83, respectively (determined by the Youden index/ROC 0/1 method). Based on our design of the study the maximum achievable plateau effect within the separate cohorts was estimated to be greater for rivaroxaban than for apixaban ( and ). The apparently stronger relationship between adherence and stroke risk is consistent with the group effect for the comparison rivaroxaban versus apixaban in our cohorts (adjusted hazard ratio 0.93, 95% CI [0.75–1.14]). While a 10% reduction in adherence in the pooled cohort resulted in a 4% increase of stroke risk, this adherence effect was higher in the rivaroxaban cohort by additional 2% (adjusted HR 1.02, 95% CI [0.99–1.05]). Both DOACs differed only slightly in their PDC distribution, with patients in the rivaroxaban cohort having higher mean and identical median adherence scores as patients in the apixaban cohort ( and , ). Based on these cut-off values, approximately 30% of rivaroxaban patients and 32% of the apixaban patients were classified as poorly adherent. Numerous patient characteristics were associated with poor adherence according to these adherence cut-off values in adjusted logistic models (Supplementary Figure 1).
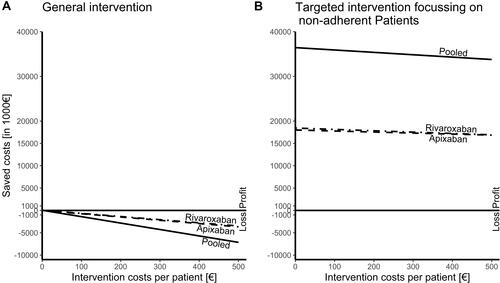
Impact of Supportive Interventions on Averted Events
shows that a targeted intervention to improve patient adherence was significantly superior to a non-targeted intervention offered to all patients. Accordingly, a non-targeted intervention ceased to be cost-effective, whereas a targeted intervention allows for intervention costs of more than 500 Euros per patient. Of note, the saved costs were directly proportional to the events prevented. Thus, the general intervention potentially prevented a mean of 0.04 strokes per 1000 patient-years (combined from the simulation of rivaroxaban and apixaban), whereas the targeted intervention potentially prevented a mean of 27.8 strokes per 1000 patient-years (combined from the simulation of rivaroxaban and apixaban).
Figure 3 Effect of supportive interventions on stroke events in atrial fibrillation and net cost per patient receiving such an intervention.
Discussion
In our work, we determined the minimum adherence threshold above which the DOACs rivaroxaban and apixaban achieve at least 80% efficacy. The adherence cut-offs we obtained are slightly below the conventional limit of 0.8. Using adjusted adherence risk models, we were able to extrapolate the intervention effect on adherence improvement. This extrapolation not only verified our analysis but may also be an interesting approach for future interventions.
In our population, we noticed similar adherence PDC distributions for the studied DOACs, with the median of the dabigatran cohort achieving the lowest estimate. This appears to be in line with the previous literature, where dabigatran predominantly showed lower median adherence values compared to rivaroxaban and apixaban.Citation38–Citation40 In contrast to other populations, patients in our cohorts were old aged.Citation4,Citation38–Citation40 Additionally, differences between cohorts in the literature and our population existed with regard to comorbidities. For example, hypertension, diabetes, and renal failure occurred slightly more frequently in our population.Citation4,Citation38–Citation40 Moreover, we observed higher CHA2DS2-VASc scores on average.Citation39 With regard to the potential inter-relationship between patient characteristics and adherence, these small differences may partly explain the difference in the adherence estimates in our population compared with previous work.Citation4
To ensure that the effect size of our results compared with those measured in clinical trials was plausible, we compared them with the results of randomized controlled clinical trials. The adherence-risk relationships ( and ) observed in our study appear plausible when compared with concentration-stroke relationships from pivotal DOAC trials that also found an exponential decrease and a comparable reduction in stroke risk with increasing DOAC exposure.Citation41,Citation42 Although our curves decreased exponentially, they did not flatten as much at high adherence values as in previous studies, which may be due to the calculation of our adherence measure. The PDC by definition truncates any value above the full maximum daily dose and sets it to the maximum. Higher dose ranges are thus fixed at 100%. As a consequence, it is possible that we did not reach the plateau in our dose-response curves. This is a natural consequence of PDC, which must be seen as a substitute for the actually ingested dose or resulting exposure, with this exposure-response relationship being the gold standard. Using our study design, the estimated net pharmacological effect of apixaban and rivaroxaban was within the expected range,Citation43,Citation44 and group differences were small, possibly reflecting baseline differences in CHA2DS2-VASc scores between treatment cohorts ().
Overall, our results are consistent with findings of previous studies that used comparable approaches to quantify the adherence effect on stroke risk.Citation45–Citation50 For example, Shore et alCitation4 observed a 13% increase in the hazard of stroke for every 10% reduction in dabigatran adherence (adjusted HR 1.13, 95% CI [0.97–1.33]). This is statistically comparable to the 2% risk increase (in the hazard of stroke) for every 10% reduction in dabigatran adherence we observed with our study design (adjusted HR 1.02, 95% CI [0.9–1.15]). Borne et alCitation51 found an increased stroke risk of 7% with each 10% decrease in rivaroxaban adherence (adjusted HR 1.07, 95% CI [0.89–1.28]), which is statistically comparable to the 5% increase found in our analysis (adjusted HR 1.05, 95% CI [0.98–1.12]) using our study design. One possible explanation regarding the similar relationship between non-adherence and stroke risk in our cohort and in previously published cohorts is probably the comparability of covariates. All cohorts were generated from real-world data, used relatively similar inclusion and exclusion criteria, and were similar in many summary statistics,Citation4,Citation51 limiting the impact of small variations in a few covariates (eg, age). Finally, it is plausible that underdosing was also associated with an increased risk of stroke because, like poor adherence, it leads to lower DOAC exposure.Citation20,Citation21,Citation52
Using these adherence-stroke relationships in economic projections revealed that a targeted intervention is more efficient than a general intervention offered to all patients regardless of their adherence value (). Overall, there are several conceivable factors modulating the success of an adherence intervention that equally reduce clinical events and costs. The maximum achievable effect depends on baseline adherence distribution and on the compound’s efficacy. Concerning the latter, the absolute effectiveness of the substance determines the maximum achievable effect, while the slope of the relationship determines the individual benefit from an adherence increase. Finally, the nature of the intervention itself is decisive as it may improve adherence significantly in some patients while being ineffective in others. In our example of a steep adherence-response relationship with an early beginning at low adherence values, an intervention would have a particularly large influence on costs when targeted at a group below the adherence cut-off (assuming a large unexploited benefit and thus an opportunity to generate large responses with small improvements).
When interpreting the results of this study, the following limitations need to be considered. The first limitation relates to the data source and calculation of adherence: limitations of data generated for billing purposes are well knownCitation53 and concern, for example, the correctness of the codes. This has been addressed as far as possible by using established and validated code sets to select the population and to define outcomes and covariates (internal validity) and by aligning the study design with previous work (external reference as a surrogate for external validity). On the other hand, the adherence measure of PDC derived from billing data is itself an approximation. As previously shown by Steiner et al, the refill compliance is considered a good marker of adherence in health insurance systemsCitation54 but the actual adherence behavior within prescription episodes, such as the temporal pattern of omitted doses, remains unclear. It may well make a difference whether one single dose is omitted from a twice-daily regimen, whether both single doses are omitted sporadically, or whether a drug holiday is taken. In this context, it is also important to note that our data source does not distinguish between planned episodes of treatment discontinuation (eg, after a bleeding event) and non-adherence. However, the proportion of patients admitted for bleeding episodes was low (2.3%) and their in-hospital stay was short (median: 6 days), suggesting that intentional pausing of DOACs did not significantly affect these results. Another important limitation is the sample size and the number of events; this was especially obvious as no adherence-stroke relationship could be reasonably modelled for dabigatran. A limiting factor regarding the events of interest is that only patients hospitalized with a stroke can be considered as having an outcome. Patients who died of a stroke without being hospitalized are lost in our database because the causes of death are not coded. However, this loss of information in the follow-up period can be considered as uninformative with regard to the adherence effect because we consider that drug intake patterns do not determine whether a patient is admitted to hospital or dies in the outpatient sector. Thus, we only expect a reduced number of events, but this reduced event frequency may have nevertheless influenced the statistical power of the study.
Conclusion
Using health insurance data as a data source and PDC estimates as a marker for individual patient adherence, the present analysis provided critical threshold values for poor adherence with the two most frequently prescribed DOACs in Germany, rivaroxaban and apixaban. The cut-off-values of rivaroxaban (PDC: 0.78) and apixaban (PDC: 0.8) are only slightly different from the conventional cut-off value (PDC: 0.8), which is reassuring because no substantial misclassification will result from further use of this value (especially when calculated from data sources other than ours). These adherence cut-offs can be applied in prospective studies to investigate whether such a categorization can help clinicians to develop promising adherence measures. They can equally be used in predictive models that detect patients at a higher risk for poor adherence. Given that effective interventions exist, our projections of interventional impact suggest that targeted interventions for patients with poor adherence identified by our cut-off values could substantially contribute to treatment success.
Acknowledgments
Andreas D. Meid is thankful for being supported by the Physician-Scientist Programme of the Medical Faculty of Heidelberg University. We would like to thank Claudia Marquart for her expert assistance with the linguistic revision of the manuscript.
The ARMIN study group: Christiane Eickhoff, Uta Mueller, Martin Schulz (ABDA – Federal Union of German Associations of Pharmacists, Berlin); Andreas Fuchs, Dorit Braun, Ulf Maywald (AOK PLUS, Dresden); Catharina Doehler, Mike Maetzler (Association of Statutory Health Insurance Physicians – Saxony, Dresden); Anja Auerbach, Urs Dieter Kuhn, Anke Moeckel (Association of Statutory Health Insurance Physicians – Thuringia, Weimar); Christine Honscha, Susanne Donner (State Association of Pharmacists – Saxony, Leipzig); Stefan Fink, Kathrin Wagner (State Association of Pharmacists – Thuringia, Erfurt); Andreas D. Meid, Robert Moecker, Carmen Ruff, Hanna M. Seidling, Felicitas Stoll, Marina Weissenborn, Lucas Wirbka (Heidelberg University Hospital, Heidelberg).
Disclosure
Lucas Wirbka is funded by the German Innovation Funds according to § 92a (2) Volume V of the Social Insurance Code (§ 92a Abs. 2, SGB V - Fünftes Buch Sozialgesetzbuch), grant number: 01VSF18019. Andreas D. Meid is funded by the Physician-Scientist Programme of the Medical Faculty of Heidelberg University. The funding bodies did not play any role in the design of the study and data collection, analysis, and interpretation of data, and in writing the manuscript. Prof. Dr. Walter E Haefeli report grants, personal fees from Daiichi-Sankyo, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- Raparelli V, Proietti M, Cangemi R, Lip GY, Lane DA, Basili S. Adherence to oral anticoagulant therapy in patients with atrial fibrillation. Focus on non-vitamin K antagonist oral anticoagulants. Thromb Haemost. 2017;117(2):209–218. doi:10.1160/TH16-10-0757
- Baumgartner PC, Haynes RB, Hersberger KE, Arnet I. A systematic review of medication adherence thresholds dependent of clinical outcomes. Front Pharmacol. 2018;9:1290. doi:10.3389/fphar.2018.01290
- Walsh CA, Cahir C, Tecklenborg S, Byrne C, Culbertson MA, Bennett KE. The association between medication non-adherence and adverse health outcomes in ageing populations: a systematic review and meta-analysis. Br J Clin Pharmacol. 2019;85(11):2464–2478. doi:10.1111/bcp.14075
- Shore S, Carey EP, Turakhia MP, et al. Adherence to dabigatran therapy and longitudinal patient outcomes: insights from the veterans health administration. Am Heart J. 2014;167(6):810–817. doi:10.1016/j.ahj.2014.03.023
- Ruff C, Koukalova L, Haefeli WE, Meid AD. The role of adherence thresholds for development and performance aspects of a prediction model for direct oral anticoagulation adherence. Front Pharmacol. 2019;10:113. doi:10.3389/fphar.2019.00113
- Cutler RL, Fernandez-Llimos F, Frommer M, Benrimoj C, Garcia-Cardenas V. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open. 2018;8(1):e016982. doi:10.1136/bmjopen-2017-016982
- Caro JJ, Ishak KJ, Huybrechts KF, Raggio G, Naujoks C. The impact of compliance with osteoporosis therapy on fracture rates in actual practice. Osteoporos Int. 2004;15(12):1003–1008. doi:10.1007/s00198-004-1652-z
- Doro P, Benko R, Kosik E, Matuz M, Toth K, Soos G. Utilization of oral antihyperglycemic drugs over a 7-year period (1998-2004) in a Hungarian population and adherence to drug therapy. Eur J Clin Pharmacol. 2005;61(12):893–897. doi:10.1007/s00228-005-0031-9
- Hansen RA, Farley JF, Droege M, Maciejewski ML. A retrospective cohort study of economic outcomes and adherence to monotherapy with metformin, pioglitazone, or a sulfonylurea among patients with type 2 diabetes mellitus in the United States from 2003 to 2005. Clin Ther. 2010;32(7):1308–1319. doi:10.1016/j.clinthera.2010.07.011
- Hurtado-Navarro I, Garcia-Sempere A, Rodriguez-Bernal C, Santa-Ana-Tellez Y, Peiro S, Sanfelix-Gimeno G. Estimating adherence based on prescription or dispensation information: impact on thresholds and outcomes. A real-world study with atrial fibrillation patients treated with oral anticoagulants in Spain. Front Pharmacol. 2018;9:1353. doi:10.3389/fphar.2018.01353
- Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC. Good and poor adherence: optimal cut-point for adherence measures using administrative claims data. Curr Med Res Opin. 2009;25(9):2303–2310. doi:10.1185/03007990903126833
- Wu JR, Moser DK, De Jong MJ, et al. Defining an evidence-based cutpoint for medication adherence in heart failure. Am Heart J. 2009;157(2):285–291. doi:10.1016/j.ahj.2008.10.001
- Mukherjee D, Patil CG. Epidemiology and the global burden of stroke. World Neurosurg. 2011;76(6 Suppl):S85–90. doi:10.1016/j.wneu.2011.07.023
- Collaborators GBDS. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2019;18(5):439–458. doi:10.1016/S1474-4422(19)30034-1
- Godwin KM, Wasserman J, Ostwald SK. Cost associated with stroke: outpatient rehabilitative services and medication. Top Stroke Rehabil. 2011;18(Suppl 1):676–684. doi:10.1310/tsr18s01-676
- Rajsic S, Gothe H, Borba HH, et al. Economic burden of stroke: a systematic review on post-stroke care. Eur J Health Econ. 2019;20(1):107–134. doi:10.1007/s10198-018-0984-0
- Kolominsky-Rabas PL, Heuschmann PU, Marschall D, et al. Lifetime cost of ischemic stroke in Germany: results and national projections from a population-based stroke registry: the Erlangen stroke project. Stroke. 2006;37(5):1179–1183. doi:10.1161/01.STR.0000217450.21310.90
- Yao X, Shah ND, Sangaralingham LR, Gersh BJ, Noseworthy PA. Non-vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. J Am Coll Cardiol. 2017;69(23):2779–2790. doi:10.1016/j.jacc.2017.03.600
- Steinberg BA, Shrader P, Thomas L, et al. Off-label dosing of non-vitamin K antagonist oral anticoagulants and adverse outcomes: the ORBIT-AF II registry. J Am Coll Cardiol. 2016;68(24):2597–2604. doi:10.1016/j.jacc.2016.09.966
- Santos J, Antonio N, Rocha M, Fortuna A. Impact of direct oral anticoagulant off-label doses on clinical outcomes of atrial fibrillation patients: a systematic review. Br J Clin Pharmacol. 2020;86(3):533–547. doi:10.1111/bcp.14127
- Steinberg BA, Shrader P, Pieper K, et al. Frequency and outcomes of reduced dose non-vitamin K antagonist anticoagulants: results from ORBIT-AF II (the outcomes registry for better informed treatment of atrial fibrillation II). J Am Heart Assoc. 2018;7. doi:10.1161/JAHA.117.007633
- von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi:10.1016/S0140-6736(07)61602-X
- Lamberts M, Staerk L, Olesen JB, et al. Major bleeding complications and persistence with oral anticoagulation in non-valvular atrial fibrillation: contemporary findings in real-life Danish patients. J Am Heart Assoc. 2017;6:2. doi:10.1161/JAHA.116.004517
- Paschke LM, Klimke K, Altiner A, von Stillfried D, Schulz M. Comparing stroke prevention therapy of direct oral anticoagulants and vitamin K antagonists in patients with atrial fibrillation: a nationwide retrospective observational study. BMC Med. 2020;18(1):254. doi:10.1186/s12916-020-01695-7
- Dima AL, Dediu D. Computation of adherence to medication and visualization of medication histories in R with AdhereR: towards transparent and reproducible use of electronic healthcare data. PLoS One. 2017;12(4):e0174426. doi:10.1371/journal.pone.0174426
- Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–272. doi:10.1378/chest.09-1584
- Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi:10.1097/01.mlr.0000182534.19832.83
- van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626–633. doi:10.1097/MLR.0b013e31819432e5
- Cox DR. Regression models and life tables (with discussion). J Royal Stat Soc B. 1972;34:187–220.
- Royston P, Altman DG. Regression using fractional polynomials of continuous covariates: parsimonious parametric modelling (with discussion). Appl Stat. 1994;43(3):429–467. doi:10.2307/2986270
- Ritz C, Baty F, Streibig JC, Gerhard D. Dose-response analysis using R. PLoS One. 2015;10(12):e0146021. doi:10.1371/journal.pone.0146021
- Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35. doi:10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3
- Morawski K, Ghazinouri R, Krumme A, et al. Association of a smartphone application with medication adherence and blood pressure control: the MedISAFE-BP randomized clinical trial. JAMA Intern Med. 2018;178(6):802–809. doi:10.1001/jamainternmed.2018.0447
- Reidel K, Tamblyn R, Patel V, Huang A. Pilot study of an interactive voice response system to improve medication refill compliance. BMC Med Inform Decis Mak. 2008;8(1):46. doi:10.1186/1472-6947-8-46
- Huang D, Sangthong R, McNeil E, et al. Effects of a phone call intervention to promote adherence to antiretroviral therapy and quality of life of HIV/AIDS patients in Baoshan, China: a randomized controlled trial. AIDS Res Treat. 2013;2013:580974.
- Hacihasanoğlu R, Gözüm S. The effect of patient education and home monitoring on medication compliance, hypertension management, healthy lifestyle behaviours and BMI in a primary health care setting. J Clin Nurs. 2011;20(5–6):692–705. doi:10.1111/j.1365-2702.2010.03534.x
- Fitzpatrick C, Gillies C, Seidu S, et al. Effect of pragmatic versus explanatory interventions on medication adherence in people with cardiometabolic conditions: a systematic review and meta-analysis. BMJ Open. 2020;10(7):e036575. doi:10.1136/bmjopen-2019-036575
- McHorney CA, Ashton V, Laliberte F, et al. Adherence to rivaroxaban compared with other oral anticoagulant agents among patients with nonvalvular atrial fibrillation. J Manag Care Spec Pharm. 2017;23(9):980–988. doi:10.18553/jmcp.2017.23.9.980
- Brown JD, Shewale AR, Talbert JC. Adherence to rivaroxaban, dabigatran, and apixaban for stroke prevention for newly diagnosed and treatment-naive atrial fibrillation patients: an update using 2013-2014 data. J Manag Care Spec Pharm. 2017;23(9):958–967. doi:10.18553/jmcp.2017.23.9.958
- Brown JD, Shewale AR, Talbert JC. Adherence to rivaroxaban, dabigatran, and apixaban for stroke prevention in incident, treatment-naive nonvalvular atrial fibrillation. J Manag Care Spec Pharm. 2016;22(11):1319–1329. doi:10.18553/jmcp.2016.22.11.1319
- Reilly PA, Lehr T, Haertter S, et al. The effect of dabigatran plasma concentrations and patient characteristics on the frequency of ischemic stroke and major bleeding in atrial fibrillation patients: the RE-LY trial (randomized evaluation of long-term anticoagulation therapy). J Am Coll Cardiol. 2014;63(4):321–328. doi:10.1016/j.jacc.2013.07.104
- Ruff CT, Giugliano RP, Braunwald E, et al. Association between edoxaban dose, concentration, anti-Factor Xa activity, and outcomes: an analysis of data from the randomised, double-blind ENGAGE AF-TIMI 48 trial. Lancet. 2015;385(9984):2288–2295. doi:10.1016/S0140-6736(14)61943-7
- Zhang J, Wang X, Liu X, et al. Comparative effectiveness and safety of direct acting oral anticoagulants in nonvalvular atrial fibrillation for stroke prevention: a systematic review and meta-analysis. Eur J Epidemiol. 2021;36(8):793–812. doi:10.1007/s10654-021-00751-7
- Almutairi AR, Zhou L, Gellad WF, et al. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants for atrial fibrillation and venous thromboembolism: a systematic review and meta-analyses. Clin Ther. 2017;39(7):1456–1478.e36. doi:10.1016/j.clinthera.2017.05.358
- Graham DJ, Baro E, Zhang R, et al. Comparative stroke, bleeding, and mortality risks in older medicare patients treated with oral anticoagulants for nonvalvular atrial fibrillation. Am J Med. 2019;132(5):596–604 e11. doi:10.1016/j.amjmed.2018.12.023
- Lip GYH, Keshishian A, Li X, et al. Effectiveness and safety of oral anticoagulants among nonvalvular atrial fibrillation patients. Stroke. 2018;49(12):2933–2944. doi:10.1161/STROKEAHA.118.020232
- Marietta M, Banchelli F, Pavesi P, et al. Direct oral anticoagulants vs non-vitamin K antagonist in atrial fibrillation: a prospective, propensity score adjusted cohort study. Eur J Intern Med. 2019;62:9–16. doi:10.1016/j.ejim.2018.12.010
- Nielsen PB, Skjoth F, Sogaard M, Kjaeldgaard JN, Lip GY, Larsen TB. Effectiveness and safety of reduced dose non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2017;356:j510. doi:10.1136/bmj.j510
- Staerk L, Gerds TA, Lip GYH, et al. Standard and reduced doses of dabigatran, rivaroxaban and apixaban for stroke prevention in atrial fibrillation: a nationwide cohort study. J Intern Med. 2018;283(1):45–55. doi:10.1111/joim.12683
- Coleman CI, Peacock WF, Bunz TJ, Alberts MJ. Effectiveness and safety of apixaban, dabigatran, and rivaroxaban versus warfarin in patients with nonvalvular atrial fibrillation and previous stroke or transient ischemic attack. Stroke. 2017;48(8):2142–2149. doi:10.1161/STROKEAHA.117.017474
- Borne RT, O’Donnell C, Turakhia MP, et al. Adherence and outcomes to direct oral anticoagulants among patients with atrial fibrillation: findings from the veterans health administration. BMC Cardiovasc Disord. 2017;17(1):236. doi:10.1186/s12872-017-0671-6
- Garcia Rodriguez LA, Cea Soriano L, Munk Hald S, et al. Discontinuation of oral anticoagulation in atrial fibrillation and risk of ischaemic stroke. Heart. 2020. doi:10.1136/heartjnl-2020-317887
- Ihle P, Krueger K, Schubert I, et al. Comparison of different strategies to measure medication adherence via claims data in patients with chronic heart failure. Clin Pharmacol Ther. 2019;106(1):211–218. doi:10.1002/cpt.1378
- Steiner JF, Prochazka AV. The assessment of refill compliance using pharmacy records: methods, validity, and applications. J Clin Epidemiol. 1997;50(1):105–116. doi:10.1016/s0895-4356(96)00268-5z
