Abstract
Background
An increasing number of clinics offer complementary or integrative medicine services; however, clear guidance about how complementary medicine could be successfully and efficiently integrated into conventional health care settings is still lacking. Combining conventional and complementary medicine into integrative medicine can be regarded as a kind of merger. In a merger, two or more organizations − usually companies − are combined into one in order to strengthen the companies financially and strategically. The corporate culture of both merger partners has an important influence on the integration.
Purpose
The aim of this project was to transfer the concept of corporate culture in mergers to the merging of two medical systems.
Methods
A two-step approach (literature analyses and expert consensus procedure) was used to develop practical guidance for the development of a cultural basis for integrative medicine, based on the framework of corporate culture in “mergers,” which could be used to build an integrative medicine department or integrative medicine service.
Results
Results include recommendations for general strategic dimensions (definition of the medical model, motivation for integration, clarification of the available resources, development of the integration team, and development of a communication strategy), and recommendations to overcome cultural differences (the clinic environment, the professional language, the professional image, and the implementation of evidence-based medicine).
Conclusion
The framework of mergers in corporate culture provides an understanding of the difficulties involved in integrative medicine projects. The specific recommendations provide a good basis for more efficient implementation.
Introduction
In Germany and the US, complementary medicine is increasingly provided by conventional medical institutions.Citation1–Citation6 Furthermore, new terms – particularly the term “integrative medicine”Citation7,Citation8 – have been introduced to capture the increasing implementation of complementary medicine into conventional medicine (mainstream medicine).
Complementary medicine is an umbrella term, which represents a heterogeneous field with disparate beliefs and practices that can vary considerably.Citation9,Citation10 According to the National Institutes of Health in the US, “complementary” generally refers to using a non-mainstream approach together with conventional medicine.Citation11
To date, few theoretical models and frameworks for describing and evaluating complementary medicine services have been publishedCitation12,Citation13 and clear guidance about how complementary medicine could be successfully and efficiently integrated into conventional health care settings is lacking. This so-called “integrative medicine” has been defined by the Consortium of Academic Health Centers for integrative medicine in the US as
[…] the practice of medicine that reaffirms the importance of the relationship between practitioner and patient, focuses on the whole person, is informed by evidence, and makes use of all appropriate therapeutic approaches, health care professionals, and disciplines to achieve optimal health and healing.Citation14
A previous semi-structured interview study with leading experts of academic integrative medicine was performed. In addition to recommendations that include creating common goals, networking, and establishing well-functioning research teams,Citation15 the interviewees made it clear that for the successful development of integrative medicine, familiarity with the different cultures of conventional and complementary medicine plays an important role.
Combining conventional and complementary medicine into integrative medicine can be regarded as a kind of merger. In a merger, two or more organizations − usually companies − are combined into one in order to strengthen the companies financially and strategically. Merging organizations have the opportunity to adapt quickly to new or changing markets by fostering a more rapid transformation of the organization that will not occur with either organization alone.Citation16
The careful selection of the merger partners is extremely important for success. Not only must the acquirer consider the likelihood of success of combining financial and strategic aspects of both companies, it must also consider the likelihood of success of combining the corporate cultures.Citation17 It is well known that a failure to negotiate the cultural differences between the merger partners can contribute to merger failure.Citation17,Citation18
The corporate culture of an organization may be expressed as “the way we do things around here,” and this sentiment includes values, beliefs, attitudes, assumptions, norms, mission statements, aims, personal interests, behaviors, and management styles. In general, two merging organizations may not necessarily have the same corporate culture, but they should be able to act together.Citation17 In practice, several cultures (ie, microcultures) often coexist within one organization. According to Sherwin,Citation19 medical schools and teaching hospitals are under pressure to change from academic institutions to corporate organizations. In the hospital environment today, different departments often start to develop their own operational norms. These are influenced by multiple factors, including medical specialization, country, type of hospital, leadership, and employees. In general, many problems in cooperation, communication, teamwork, and acceptance of treatments can be attributed to cultural differences. In corporate mergers, organizations that once offered mutually exclusive and competitive products and services in the marketplace face challenges to become uniform and integrated.
Transferring the theoretical frameworks that have been developed for merging organizations to the two distinctive medical approaches of conventional medicine and complementary medicine might be helpful for a better understanding and further development of integrative medicine. The underlying aim for a corporate merger is to arrive at positive synergy, meaning that the final outcome of the merged system is greater than the sum of its constituent parts. Similarly, integrative medicine wants to reach synergistic therapeutic effects that lead to a better treatment outcome for patients by combining conventional and complementary medicine.Citation8
The impact of the merger on the corporate culture of both organizations is strongly influenced by the employed integration type. According to Kummer,Citation20 different degrees of integration are possible during a merger. Developing an integrative medicine referral service would be characterized as a “linking” type of integration, which allows conventional and complementary medicine to work together while maintaining their respective and independent identities; in this case, at least a mutual understanding of both cultures is needed. The creation of a new department for integrative medicine with a joint team of conventional and complementary medicine professionals would be called “the best of both worlds” integration type; here, the development of a new corporate culture is necessary.
The aim of this project was to develop practical guidance for the development of a cultural basis for integrative medicine. This guidance is based on the framework of corporate culture in “mergers” and could be used to build an integrative medicine department or integrative medicine service.
Methods
A two-step approach, including a literature analysis and expert consensus procedure, was used. The preparation of the symposium was based on a literature analysis and brief narrative telephone interviews with merger experts as well as with professionals working in integrative medicine. Relevant information on merger theory and corporate culture, as well as information on corporate culture aspects of both conventional and complementary medicine, were summarized in a written document and synthesized into a presentation for the workshop. Furthermore, integrative oncology, a growing field within integrative medicine, was identified as a good example. Workshop participants from Germany and the US were identified and invited to participate in a 2-day interdisciplinary consensus symposium. The symposium took place at the Robert Bosch Foundation in Stuttgart, Germany on October 22–23, 2012.Citation14 The 14 participants came from different backgrounds and included two leading experts on corporate culture in mergers, a hospital manager with experience in establishing an integrative medicine department in Germany, a nurse who established one of the leading integrative medicine programs in the US, four chief medical doctors from integrative medicine departments (one from Germany; three from the US), four researchers with experience in integrative medicine research from a variety of backgrounds (business, history of medicine, medical anthropology, and epidemiology), and two representatives of the supporting foundations (Robert Bosch Stiftung and The Institute for Integrative Health). The workshop included introductory lectures on mergers and corporate culture and case studies from integrative oncology, which were complemented by breakout sessions in which two interdisciplinary groups with seven participants each worked in parallel discussing the same topics over the course of 2 days. These topics included reasons for building an integrative medicine department or integrative medicine service, identifying the most relevant aspects of cultural differences between conventional and complementary medicine, and developing practical recommendations to guide the development of an integrative medicine department or integrative medicine service.
Results from the two working groups were presented in a plenary session and synthesized through a consensus discussion. In addition to written Delphi rounds, all workshop participants and those who were not able to join the workshop were asked to comment on the manuscript until final consensus was reached after the third round.
Three additional experts (one patient advocate, one chief medical doctor, and the principal investigator of a large collaborative research project on integrative oncology) – who were invited, but unable to participate in the workshop – joined the post-symposium Delphi process.
Results
From the symposium and Delphi process, some general comments and insights were derived. When building an integrative medicine department or offering an integrative medicine service, the primary aim was viewed as the achievement of positive synergy between conventional and complementary medicine and the improvement of hospital outcomes, including health care. Positive synergy was viewed as the integration of the two approaches to medicine (conventional and complementary) leading to better patient outcomes as well as to better clinic outcomes (eg, patient numbers, revenue) than either approach could achieve alone. Because several definitions exist for the terms complementary medicine and integrative medicine, it was decided that the term “integrative medicine” would be used to denote a combination of conventional medicine and complementary medicine that creates positive synergy. Providers play an important role and cultural differences between conventional health care providers and complementary medicine providers were discussed during the symposium as a threat resulting in a possible cultural clash. This would have a negative impact on synergy as well as on each provider group itself. This impact may include conflict, low morale, low productivity, poorer quality care, and turnover among key individuals and groups.Citation21
It became clear that in each hospital or department a mosaic of different perspectives generally exists (eg, medical doctors, nurses, administration, pharmacists) and that both conventional medicine and complementary medicine have many microcultures depending on their respective specialties or modalities. However, although both are heterogeneous on the microculture level, it was assumed that each has an overall macroculture. On a macro level, conventional medicine appeared to have a more uniform and sharply delineated culture with clear norms and values, whereas the macroculture of complementary medicine seemed to be more heterogeneous and strongly influenced by the different treatment modality philosophies (eg, Chinese medicine). Although conventional medicine also includes a broad variety of disciplines with heterogeneous microcultures, these were commonly seen to be highly respected in society and share a similar scientific basis, whereas complementary medicine was viewed as less respected and less scientific. Furthermore, different financial models for conventional and complementary medicine in health care were discussed, which vary between countries and states. Third party coverage is more common for conventional medicine overall, whereas complementary medicine is more often based on fee-for-service models or philanthropic support.
It became clear that providers of complementary medicine vary depending on the country in which complementary medicine is delivered, as well as national and local regulation. In Germany, for example, complementary medicine is more often provided by conventional medical doctors,Citation22 whereas in the US, it is mainly provided by non-medical doctors. Some of the recommendations below, for example, using a common language and terminology, are more relevant when conventional medical doctors and non-medical doctor complementary medicine practitioners work together.
During the discussion it became obvious that when integrating conventional and complementary medical providers, it is very likely that more than two cultures will be brought together, potentially exacerbating the challenges discussed above.
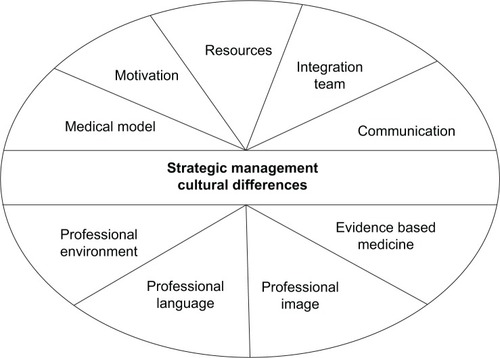
The following recommendations were developed for practical guidance to support the development of a cultural basis for integrative medicine, which could be used to build an integrative medicine department. They are divided into recommendations for general integration management and recommendations for dealing with cultural differences ().
Figure 1 Recommendation areas for general integration management and for dealing with cultural differences.
Recommendations for general integration management
The recommendations center on five general strategic dimensions of integration management. These include the definition of the medical model, motivation for integration, clarification of the available resources, development of the integration team, and development of a communication strategy.
Definition of the medical model
It is important to choose a medical model that suits the needs of patients, the clinic, and its other relevant stakeholders. The medical model includes the type of integration (eg, integrative medicine department which needs the development of a new shared culture or an integrative medicine referral service where a mutual understanding of both cultures is needed); the complementary medicine modalities to be offered, with attention to their safety and credibility (eg, starting with the more known and accepted modalities); and the degree of specialization (eg, How much specialization is reasonable and necessary to be competent and effective without losing the patient-centered and holistic approach?). The benefit to the patient should play a key role when defining the medical model.
Motivation for integration
The motivation of the administration and the providers from both sides (complementary and conventional medicine) should be succinct, explicit, and transparent for the integration and subsequent collaboration when treating patients. Both intrinsic (eg, seeing the benefit of integration for the patient) and extrinsic (eg, financial incentives) motivators should be communicated and accepted by all parties involved.
Clarification of available resources
The available resources should be defined and reasonable, including space, staff, training, and consumables, as well as time and incentives for those involved in the planning and implementation.
Building the integration team
The team should consist of visible “champions,” with interpersonal, social, and emotional skills, who can act as door openers or liaisons between administrators and practitioners from both medical approaches. However, to support sustainability, it is important not to depend on a single person. The “champions” should understand the aims, share the overall vision, and be able to work together as a team. This teamwork requires building mutual respect and belief in the validity of both approaches to medicine. The team ideally includes: 1) a conventional medical doctor in a leadership position who is highly respected in the clinic, has political savvy, and is able to compromise; 2) an administrator who is in a leading position; 3) a complementary medicine practitioner who is respected in his/her field, with good leadership and clinical skills, and who has high visibility, and brings value to the organization beyond complementary medicine; and 4) a nurse who is visible and highly respected to encourage bridging between complementary and conventional medicine as well as bridging to patients.
Communication strategy
The concept of the integrative medicine department or referral service should be over-communicated. This communication should emphasize the project’s aims, as well as describing exactly what integrative medicine services are anticipated. Strategies should be developed to increase the knowledge and understanding of integrative medicine (eg, joint events in which physicians and practitioners might socialize and bond such as conferences and trainings). Furthermore, the impact of the new service/department on the different stakeholders should be clearly communicated.Citation23,Citation24
Recommendations for overcoming cultural differences
Four cultural differences have been identified that could lead to a clash of cultures when developing and implementing an integrative medicine department or referral service: the clinic environment, the professional language, the professional image, and the implementation of evidence-based medicine. For each, the cultural difference, potential implications, and recommendations to mitigate cultural differences are outlined in .
Table 1 Identified cultural differences that could lead to a clash of cultures when developing and implementing an integrative medicine department or referral service
Discussion
The framework of corporate culture in mergers provides perspectives that allow for an understanding of the difficulties involved in integrative medicine projects. Five key actions have been identified as important in the strategy for development of an integrative medicine department or referral service: definition of the medical model, clarification of the motivation for integration, clarification of available resources, development of the integration team, and development of a communication strategy. Four cultural differences that are relevant for integrative medicine were able to be identified: the clinic environment, the professional language, the professional image, and the implementation of evidence-based medicine. Furthermore, recommendations to mitigate these cultural differences were provided.
The recommendations were based on a literature analysis and systematic multidisciplinary expert experience. One limitation is that in the symposium participants represented only two countries, Germany and the US. These countries were selected because both had strong development in the field of integrative medicine within medical schools and teaching hospitals in recent years, but have very different health care systems. The recommendations might have differed had experts from other countries such as China or India participated, where the culture of traditional medicine has long been the predominant medical approach and is still widely available. One further limitation is that patients’ barriers to integrative medicine were not discussed. However, it was recommended that it is important to choose a medical model that suits the needs of patients, and to make this possible, patients should be fully integrated into the development process of the integrative medicine department or integrative medicine service.
Furthermore, integrative medicine is a broad and heterogeneous field and the recommendations provided here should be viewed as general guidance. When putting these recommendations into practice, it will be necessary to take many details of the actual context into account. The structure of the health care system and reimbursement guidelines will have an especially strong influence on the choice of the medical model. In the US and Germany, the reimbursement of integrative medicine could be various based on the policy. Due to this, not all integrative medicine services will be economically self-sustainable. It is important to allow enough time and resources for the strategic planning phase of the proposed integrative medicine department. Sometimes the best decision may be to not pursue implementation of the integrative medicine department project, because it will be neither accepted nor sustainable. The integration project might even lose money and reduce the productivity of the organization as a whole. It is noteworthy to mention that the integration of complementary and alternative medicine into a mainstream hospital is only possible if the hospital is financially viable.
A new integrative medicine department that is based on the integration type “best of both worlds” needs the development of a “new,” shared culture,Citation20 a process that can be resource intensive. For a successful and efficient integrative medicine referral service that is based on the integration type of “linking,” corporate culture also plays an important role, but the focus might be better directed toward developing mutual respect and an understanding of cultural differences than at the development of a completely “new” culture. Such mutual respect and understanding would be based not only on a shared professional language, but also on an appropriate orientation to and familiarity with the professional environment. Moreover, sensitivity to incentive systems is critical, especially in environments where complementary medicine and conventional medicine may not be viewed or valued the same. Without these, patient safety and productivity might be negatively affected. Overall, the integration might be less resource intensive and easier in Germany than in the US, because in Germany complementary medicine is often provided by conventionally trained medical doctors who know the conventional environment and speak the professional language. However, independent of their professional backgrounds, the “champions” from the complementary medicine field need strong leadership skills and the ability to work in a team in addition to their clinical skills. Currently, in both Germany and the US, there is a shortage of complementary medicine practitioners with extensive skills and experience in leading multidisciplinary teams. Leadership in integrative medicine is an area that needs development, and should include clear definitions of the necessary competencies, motivation incentives, and training in leadership competencies.
Acknowledgments
The authors thank Iris Bartsch and Hildegard Micko for their assistance in organizing the symposium.
The symposium was funded by the Robert Bosch Stiftung. Marion Pérard received a scholarship from The Institute for Integrative Health. Claudia Witt’s work, in her role as Chair of Complementary Medicine Research, was funded by the Carstens Foundation.
Disclosure
The authors report no conflicts of interest in this work.
References
- HorriganBLewisSAbramsDPechuraCIntegrative Medicine in America: How Integrative Medicine is Being Practiced in Clinical Centers Across the United StatesMinneapolis, MNThe Bravewell Collaborative2012 Available from: http://www.bravewell.org/content/Downlaods/IMinAm.pdfAccessed August 27, 2014
- MaizesVRakelDNiemiecCIntegrative medicine and patient-centered careExplore (NY)20095527728919733814
- RuggieMMainstreaming complementary therapies: new directions in health careHealth Aff (Millwood)200524498099016136636
- DobosGJVoissPSchwiddeIIntegrative oncology for breast cancer patients: introduction of an expert-based modelBMC Cancer20121253923170989
- KnutsonLJohnsonPJSidebottomAFyfe-JohnsonADevelopment of a hospital-based integrative healthcare programJ Nurs Adm201343210110723343726
- LaucheRCramerHMoebusSResults of a 2-week inpatient stay at the department for internal and integrative medicine: an observational studyEvid Based Complement Alternat Med2012201287587423133499
- HolmbergCBrinkhausBWittCExperts’ opinions on terminology for complementary and integrative medicine – a qualitative study with leading expertsBMC Complement Altern Med20121221823151006
- DobosGIntegrative medicine – medicine of the future or “old wine in new skins”?Eur J Integr Med200913109115
- GevitzNAlternative medicine and the orthodox canonMt Sinai J Med19956221271317753079
- JütteRAlternative medicine and medico-historical semanticsJütteREklöfMNelsonMCHistorical Aspects of Unconventional Medicine: Approaches, Concepts, Case StudiesSheffieldEuropean Association for the History of Medicine and Health20011126
- Complementary, alternative, or integrative health: what’s in a name? [webpage on the Internet]Bethesda, MDNational Center for Complementary and Alternative Medicine (NCCAM)2008 [updated July 2014]. Available from: http://nccam.nih.gov/health/whatiscamAccessed June 6, 2014
- BoonHVerhoefMO’HaraDFindlayBFrom parallel practice to integrative health care: a conceptual frameworkBMC Health Serv Res2004411515230977
- LeckridgeBThe future of complementary and alternative medicine – models of integrationJ Altern Complement Med200410241341615165426
- About us: definition of integrative medicine [webpage on the Internet]Minneapolis, MNConsortium of Academic Health Centers for Integrative Medicine2004 [edited November 2009]. Available from: http://www.imconsortium.org/about/Accessed June 6, 2014
- WittCMHolmbergCChanging academic medicine: strategies used by academic leaders of integrative medicine – a qualitative studyEvid Based Complement Alternat Med2012201265254623093984
- AhernKRWestonJFM&As: the good, the bad, and the uglyJournal of Applied Finance2007171520
- CartwrightSCooperCLManaging Mergers, Acquisitions and Strategic Alliances Integrating People and CulturesOxfordButter-worth-Heinemann1996
- ChatterjeeSLubatkinMSchweigerDWeberYCultural differences and shareholder value: explaining the variability in the performance of related mergerStrategic Management Journal1992135319334
- SherwinJChanging culture, changing process: academic medicine’s own work in progress [webpage on the Internet]Washington, DCAssociation of American Medical Colleges2011 [cited October 18, 2011]. Available from: https://www.aamc.org/newsroom/reporter/october2011/262456/changingculture.htmlAccessed May 12, 2013
- KummerCOvercoming the challenges and issues of post-merger integration: putting PMI in the driver’s seat in the M&A processGaneshCMergers and Acquisitions – Issues and Perspectives from the Asia–Pacific RegionTokyoAsian Productivity Organization2012133147
- LubatkinMSchweigerDMWeberYTop management turnover in related M&A’s: an additional test of the theory of relative standingJ Manage19992515573
- JoosSMusselmannBMikschARosemannTSzecsenyiJThe role of complementary and alternative medicine (CAM) in Germany – a focus group study of GPsBMC Health Serv Res2008812718549476
- SchweigerDMDeNisiASCommunication with employees following a merger: a longitudinal field experimentAcad Manage J1991341110135
- SchweigerDMM&A Integration: A Framework for Executives and ManagersNew York, NYMcGraw Hill2002
