Abstract
Background
Patient nonadherence to cardiac medications following acute coronary syndrome (ACS) is associated with increased risk of recurrent events. However, the prevalence of cognitive dysfunction and poor health literacy among ACS patients and their association with medication nonadherence are poorly understood.
Methods
We assessed rates of cognitive dysfunction and poor health literacy among participants of a clinical trial that tested the effectiveness of an intervention to improve medication adherence in patients hospitalized with ACS. Of 254 patients, 249 completed the Rapid Estimate of Adult Literacy in Medicine, Revised (REALM-R) survey, an assessment of risk for poor literacy, and the St Louis University Mental Status (SLUMS) exam, a tool assessing for neurocognitive deficits, during ACS hospitalization. We assessed if SLUMS or REALM-R scores were associated with medication adherence.
Results
Based on SLUMS score, 14% of patients were categorized as having dementia, and 52% with mild neurocognitive disorder (MNCD). Based on REALM-R score of ≤6, 34% of patients were categorized as at risk for poor health literacy. There was no association between poor health literacy and medication nonadherence. Of those with MNCD, 35.5% were nonadherent, compared to 17.5% with normal cognitive function and 6.7% with dementia. In multivariable analysis, cognitive dysfunction was associated with medication nonadherence (P=0.007), mainly due to an association between MNCD and nonadherence (odds ratio =12.2, 95% confidence interval =1.9 to 243; P=0.007). Cognitive status was not associated with adherence in patients randomized to the intervention.
Conclusion
Cognitive dysfunction and risk for poor health literacy are common in patients hospitalized with ACS. We found an association between MNCD and medication nonadherence in the usual care group but not in the intervention group. These findings suggest efforts to screen for MNCD are needed during ACS hospitalization to identify patients at risk for nonadherence and who may benefit from an adherence intervention.
Keyword:
Introduction
Mild cognitive dysfunction is present in 15% of those over the age of 70,Citation1 affecting an estimated 5.4 million people in the United States.Citation2 Cognitive dysfunction may have implications following acute coronary syndrome (ACS) as its presence may impact patients’ ability to understand and adhere to secondary prevention medication regimens that potentially consist of several new medicines with differing dosing schedules.Citation3 Up to 12% of patients with ACS have cognitive dysfunction;Citation4 however, the relationship between cognitive dysfunction at time of presentation of ACS and subsequent medication nonadherence is poorly defined.
Poor health literacy is present in roughly 30% of ambulatory patients and is associated with cognitive dysfunction.Citation5 Independent of cognitive dysfunction, level of health literacy is an important predictor of medication adherence,Citation6,Citation7 and patients with low levels of literacy are at higher risk for clinically relevant medication errors.Citation8 Limited data exist regarding the prevalence and impact of poor health literacy in those presenting with ACS.Citation4 Further, the prevalence of coincident poor health literacy and cognitive dysfunction in the setting of ACS, and their relationship with medication nonadherence, is unknown.
To assess the prevalence of cognitive dysfunction and poor health literacy, and their associations with medication nonadherence, we analyzed data from the Multifaceted Intervention to Improve Cardiac Medication Adherence and Secondary Prevention Measures (MEDICATION) study. This was a randomized clinical trial that assessed the effect of a multifaceted intervention on medication adherence in veterans presenting with ACS.Citation9 In the study, a greater proportion of patients randomized to the intervention were adherent compared to the usual care patients (89% versus 74%; P=0.03). The objectives of the current analysis were to describe the prevalence of cognitive dysfunction and poor health literacy in patients presenting with ACS. In addition, we sought to evaluate if either cognitive dysfunction or health literacy were independently associated with medication nonadherence in the year following ACS hospital discharge among patients randomized to usual care. Then, we assessed the extent to which these associations would be modified among patients randomized to the intervention group given the positive effects of the intervention demonstrated in the main study.
Methods
Patient population
The design of the randomized trial has been described in detail previously.Citation10 In brief, this multicenter, prospective clinical trial enrolled veterans at one of four Veterans Affairs (VA) medical centers with ACS as the primary reason for hospital admission. All patients admitted with ACS (defined as ST-elevation myocardial infarction, non-ST elevation myocardial infarction, or unstable angina) who used the VA as their usual source of healthcare were screened for eligibility to participate. Patients were ineligible if they were admitted for a noncardiac primary diagnosis, were planned to be discharged to a nursing home or skilled nursing facility, had an irreversible noncardiac medical condition likely to affect 6-month survival, lacked telephone or cellular phone service, or did not regularly fill medications at a VA pharmacy. Patients were randomized to a multifaceted intervention designed to improve medication adherence and outcomes or usual care. The intervention consisted of pharmacist-led medication reconciliation and tailoring, patient education, collaborative care between the study pharmacist and a patient’s primary care doctor and/or cardiologist, and two types of voice messaging including educational and medication refill reminder calls.
Exposure variables
Of 254 enrolled patients, 249 (98%) completed the St Louis University Mental Status (SLUMS) exam, a tool assessing for neurocognitive deficits, and the Rapid Estimate of Adult Literacy in Medicine, Revised (REALM-R) survey, an assessment of patients at risk for poor literacy skills, at baseline during their ACS hospitalization.
The SLUMS exam is a 30-point screening questionnaire that tests orientation, memory, attention, and executive function. The sensitivity and specificity of the SLUMS exam has been validated in a VA cohort.Citation11 As compared to the clinical dementia rating, the SLUMS exam has a sensitivity of 74% and specificity of 65% to detect mild neurocognitive disorder (MNCD) and a sensitivity of 93% and specificity of 96% to detect dementia in the VA population.Citation12 Patient scores are interpreted in the context of the level of patient education. For patients with at least a high school education, a score of 27–30 is normal, 21–26 represents MNCD, and 1–20 represents dementia. For those with less than a high school education, a score of 25–30 is normal, 20–24 represents MCND, and 1–19 represents dementia. In our study, patients with a SLUMS exam score ≤20 were categorized as having dementia, those with a score between 21 and 26 were categorized as having MNCD, and those with a score ≥27 were categorized as normal.
The REALM-R survey is a commonly used tool for assessing patients at risk for poor health literacy and correlates well with standardized reading tests.Citation13 Scores range from 0 to 8, and a score of ≤6 corresponds a sixth grade reading level.Citation13 In our analysis, patients with a score ≤6 on the REALM-R survey were categorized as at high risk of health illiteracy, while those with a score ≥7 were categorized as normal.
Outcomes
The primary outcome was the proportion of patients who were adherent to cardioprotective medication regimens in the year following ACS. Medications included in the adherence analysis were beta-blockers, statins, clopidogrel, angiotensin converting enzyme inhibitors, and angiotensin receptor blockers. Aspirin was not included in the analysis due to the large proportion of veterans who obtain aspirin over-the-counter.
Of the 249 patients with baseline survey data, 238 had complete follow-up data available for the adherence analysis. Medication adherence was calculated based on the proportion of days covered (PDC) during a follow-up period of 365 days that a patient had a medication available. The calculation was adjusted for inpatient hospitalization, medication cancellation, medication changes within class, medication fills prior to enrollment date, and death. Adherence for each class of medication was scored from 0 to 1.00 (perfect medication coverage) and was then averaged for all prescribed classes of medications to calculate a summary PDC. Patients with a summary PDC >0.80 were categorized as adherent.
Statistical analysis
Demographic variables were compared across SLUMS and REALM-R categories separately using chi-square tests for categorical variables and t-tests or f-tests for continuous variables. Distributions were summarized as means and standard deviations for continuous variables and as proportions and numbers for categorical variables. Using medication adherence as an outcome, we used three logistic regression models to assess 1) the bivariate association between REALM-R and adherence, 2) the bivariate association between SLUMS and adherence, and 3) a multivariate model with SLUMS and REALM-R as primary predictors, adjusted for potential confounders. We selected confounders from age, sex, race, smoking history, hypertension, hyperlipidemia, diabetes mellitus, cerebrovascular disease, chronic lung disease, coronary artery disease history, peripheral arterial disease, depression, and chronic kidney disease using backwards stepwise variable selection with a P-value cutoff of 0.2. We did not include the primary predictors in the models while selecting the covariates. We fit all three models in the usual care group and separately in the intervention group. An alpha level of 0.05 was used as a cutoff for all P-values.
Results
Based on the SLUMS questionnaire, 14% (n=36) of patients were categorized as having dementia and 52% (n=130) were categorized as having MNCD. Overall, 67% of patients were categorized as having some level of cognitive dysfunction. Both increasing age (P=0.01) and non-white race (P=0.03) were associated with the presence of dementia ().
Table 1 SLUMS score and covariates
Based on REALM-R survey score, 34% (n=85) were categorized as at risk for poor health literacy. Non-white race was the only demographic variable associated with health literacy and was negatively associated with REALM-R (). Coincident cognitive dysfunction and risk for poor health literacy were present in roughly one-quarter of patients. REALM-R and SLUMS scores were correlated, though the strength of this correlation was low (Kendall correlation =0.18; significance P=0.005).
Table 2 REALM-R score and covariates
In the usual care arm, 25.6% (30/117) of patients were nonadherent to their cardiovascular medications. Cognitive dysfunction as measured by SLUMS was associated with medication nonadherence in unadjusted analysis (P=0.017), where patients with MNCD were more likely to have non-adherence; 35.5% (22/62) of patients with MNCD were nonadherent, compared to 17.5% (7/40) of patients with normal cognitive function and 6.7% (1/15) of patients with dementia (). In contrast, health illiteracy as measured by REALM-R was not associated with medication nonadherence (P=0.92). In multivariable models adjusting for race, age, and history of diabetes, cognitive dysfunction was associated with medication nonadherence (P=0.007), primarily due to an association between MNCD and nonadherence (odds ratio [OR] =12.2; 95% confidence interval [CI] =1.9–243), while normal cognition was not associated with medication nonadherence (OR =4.8; 95% CI =0.6–101.5) (). Finally, REALM-R was not associated with adherence in the adjusted model (P=0.31).
Figure 1 Medication adherence across SLUMS score.
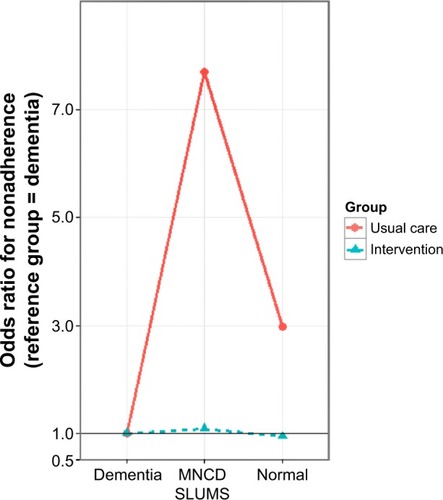
Table 3 Relationship between SLUMS and REALM-R scores and medication nonadherence
In the intervention group, 10.7% (13/121) of patients were nonadherent to their cardiovascular medications. SLUMS score was not associated with adherence in the intervention group in unadjusted (P=0.98) or adjusted (P=0.91) analysis. Some 11.3% (7/62) of patients with MNCD were nonadherent, compared to 10% (4/40) of patient with normal cognitive function and 10.5% (2/19) of patients with dementia. In addition, REALM-R score was also not associated with adherence in the intervention group in unadjusted (P=0.13) or adjusted (P=0.17) analysis.
Discussion
The objectives of this study were to describe the prevalence of cognitive dysfunction and health illiteracy among patients hospitalized for ACS and to evaluate the association with medication nonadherence in the year following ACS hospitalization. We found that cognitive dysfunction was common (67%) and associated with medication nonadherence in the usual care group but not in the intervention group, suggesting that the intervention may have modified this association. In contrast, poor health literacy was common (34%) but not associated with medication adherence. These findings suggest patients with MNCD are at risk for poor medication adherence following ACS, and interventions focusing on adherence may help improve the medication-taking behavior of these patients.
The prevalence of cognitive dysfunction and risk for poor health literacy in our cohort, 67% and 34%, respectively, are higher than prior reports. These studies found a significantly lower rate of cognitive dysfunction in patients presenting with ACS (2.1% of over 85,000 patients in one series)Citation14 but relied on claims data, likely underestimating the prevalence. The Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-CVD) study assessed the prevalence of cognitive dysfunction and the level of health literacy in patients enrolled in a randomized control trial assessing the effect of a pharmacist-based intervention on the rate of serious medication errors in the first 30 days following hospital discharge for ACS or decompensated heart failure.Citation4 The rate of cognitive dysfunction in that cohort was 11.5%, considerably higher than found in analyses based on claims data, though significantly lower than in our cohort. The rate of poor health literacy in the PILL-CVD study was 18.7%, also lower than that of our cohort. These differences may reflect the different sensitivity of the screening tools used or differences in the patient populations in the PILL-CVD study and in our study.
Medication nonadherence following ACS is common and is associated with an increased risk of recurrent myocardial infarction and death.Citation15–Citation18 A number of factors have been associated with medication nonadherence following ACS, including older age, lower level of education, and preexisting cardiovascular disease.Citation18 While the mechanisms contributing to nonadherence are complex, cognitive dysfunction and low levels of health literacy have been associated with adverse outcomes in those with ACS and heart failure, respectively. An investigation of the prognostic influence of comorbid conditions in a cohort of patients with non-ST elevation ACS found the presence of dementia predicted death (hazard ratio 3.1).Citation19 In a study of ambulatory heart failure patients with New York Heart Association class II–IV symptoms, 37% had low literacy. Low literacy was associated with a significantly increased rate of all-cause hospitalization (incidence rate ratio [IRR] 1.31) and heart failure-related hospitalization (IRR 1.46).Citation20 Our findings further support that cognitive dysfunction and poor health literacy are common in those with ACS, and may contribute to medication nonadherence and adverse clinical outcomes in this population.
Our data suggest MNCD may play an important role in medication nonadherence following ACS, and the rate of nonadherence may be improved with multidisciplinary interventions designed to improve adherence. In our cohort, dementia was not associated with adherence. While the mechanisms for the difference in adherence between those with MNCD and dementia are not known, one potential explanation is greater support systems in place for those with recognized significant cognitive dysfunction. Patients with MNCD may lack the social support or assistance from the healthcare system more frequently available to those with dementia. Therefore patients with MNCD are at increased risk for medication nonadherence. More data are needed to better understand whether the combination of cognitive dysfunction and poor adherence leads to worse clinical outcomes after ACS.
Cognitive dysfunction and risk for poor health literacy were poorly predicted by traditional demographic variables (only age and race were significantly associated), and were not associated with preexisting medical comorbidities in our cohort. Non-white race has been associated with medication nonadherence post-ACS by others,Citation21 and further efforts to identify factors contributing to this association are needed. Systematic implementation of protocols for screening for MNCD may allow for identification of patients for whom a targeted intervention to improve medication adherence post-ACS is of benefit. Further studies should assess the impact of screening for MNCD to facilitate implementation of interventions to improve medication adherence and clinical outcomes in patients after ACS hospital discharge. In contrast, we did not find an association between health literacy and adherence. Additional studies should assess whether health numeracy impacts medication adherence.
Several limitations to our study should be acknowledged. First, we analyzed data from a randomized control trial that enrolled patients exclusively from VA medical centers. The majority of these patients were men and white. The generalizability of these findings outside of the VA population is unknown. Second, the VA is an integrated healthcare delivery system. Is it unclear how these findings may be translated to a nonintegrated healthcare delivery system. However, the findings are relevant to veterans who receive care in the VA system as well as the large number of patients who receive care in other large integrated healthcare delivery systems. Third, we do not have data regarding all variables that have been previously associated with medication adherence, including housing status. It is possible this or other unrecognized factors may have contributed to the difference in adherence between those with MNCD and dementia observed in our study. Fourth, we do not have data regarding the level of education achieved for patients in our cohort. We categorized patients’ cognitive status based on SLUMS score assuming at least a high school education. It is possible this overestimated the prevalence of significant cognitive dysfunction in our cohort. Lastly, we assessed medication adherence with pharmacy refill data. It is possible that patients refilled medications without ingesting the pills. However, pharmacy refill data as a measure of adherence has been validated in several other medication adherence studies.Citation22
In conclusion, we found cognitive dysfunction and risk for poor health literacy to be common in a cohort of veterans hospitalized for ACS. Mild cognitive impairment was associated with lower rates of medication adherence in patients randomized to usual care. There was no association between level of cognitive dysfunction and medication adherence in those patients randomized to the intervention, suggesting a role for such a multidisciplinary adherence intervention in patients with cognitive dysfunction and ACS.
Disclosure
The authors report no conflicts of interest in this work.
References
- RobertsROGedaYEKnopmanDSThe Mayo Clinic Study of Aging: design and sampling, participation, baseline measures and sample characteristicsNeuroepidemiology2008301586918259084
- PlassmanBLLangaKMFisherGGPrevalence of cognitive impairment without dementia in the United StatesAnn Intern Med2008148642743418347351
- Sanfélix-GimenoGPeiróSFerrerosIAdherence to evidence-based therapies after acute coronary syndrome: a retrospective population-based cohort study linking hospital, outpatient, and pharmacy health information systems in Valencia, SpainJ Manag Care Pharm201319324725723537459
- KripalaniSRoumieCLDalalPILL-CVD (Pharmacist Intervention for Low Literacy in Cardiovascular Disease) Study GroupEffect of a pharmacist intervention on clinically important medication errors after hospital discharge: a randomized trialAnn Intern Med2012157111022751755
- WolfMSCurtisLMWilsonEALiteracy, cognitive function, and health: results of the LitCog studyJ Gen Intern Med201227101300130722566171
- MurrayMDWuJTuWHealth literacy predicts medication adherenceClin Pharmacol Ther200475P76
- NoureldinMPlakeKSMorrowDGTuWWuJMurrayMDEffect of health literacy on drug adherence in patients with heart failurePharmacotherapy201232981982622744746
- DavisTCWolfMSBassPFLiteracy and misunderstanding prescription drug labelsAnn Intern Med20061451288789417135578
- HoPMLambert-KerznerACareyEPMultifaceted intervention to improve medication adherence and secondary prevention measures after acute coronary syndrome hospital discharge: a randomized clinical trialJAMA Intern Med2014174218619324247275
- Lambert-KerznerADel GiaccoEJFahdiIEMultifaceted Intervention to Improve Cardiac Medication Adherence and Secondary Prevention Measures (Medication) Study InvestigatorsPatient-centered adherence intervention after acute coronary syndrome hospitalizationCirc Cardiovasc Qual Outcomes20125457157622811499
- TariqSHTumosaNChibnallJTPerryMHMorleyJEComparison of the Saint Louis University mental status examination and the mini-mental state examination for detecting dementia and mild neurocognitive disorder – a pilot studyAm J Geriatr Psychiatry2006141190091017068312
- Cummings-VaughnLAChavakulaNNMalmstromTKTumosaNMorleyJECruz-OliverDMVeterans Affairs Saint Louis University Mental Status examination compared with the Montreal Cognitive Assessment and the Short Test of Mental StatusJ Am Geriatr Soc20146271341134624916485
- BassPFWilsonJFGriffithCHA shortened instrument for literacy screeningJ Gen Intern Med200318121036103814687263
- LinCFWuFLLinSWAge, dementia and care patterns after admission for acute coronary syndrome: an analysis from a nationwide cohort under the National Health Insurance coverageDrugs Aging2012291081982823018581
- FerrariEBenhamouMCerboniPMarcelBCoronary syndromes following aspirin withdrawal: a special risk for late stent thrombosisJ Am Coll Cardiol200545345645915680728
- HoPMSpertusJAMasoudiFAImpact of medication therapy discontinuation on mortality after myocardial infarctionArch Intern Med2006166171842184717000940
- RasmussenJNChongAAlterDARelationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarctionJAMA2007297217718617213401
- SpertusJAKettelkampRVanceCPrevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: results from the PREMIER registryCirculation2006113242803280916769908
- SanchisJNúñezJBodíVInfluence of comorbid conditions on one-year outcomes in non-ST-segment elevation acute coronary syndromeMayo Clin Proc201186429129621346247
- WuJRHolmesGMDeWaltDALow literacy is associated with increased risk of hospitalization and death among individuals with heart failureJ Gen Intern Med20132891174118023478997
- CrowleyMJZulligLLShahBRMedication non-adherence after myocardial infarction: an exploration of modifying factorsJ Gen Intern Med2015301839025361685
- HoPMBrysonCLRumsfeldJSMedication adherence: its importance in cardiovascular outcomesCirculation2009119233028303519528344
