Abstract
Purpose
Numerous studies showed the effectiveness of pharmaceutical care in improving medication adherence in primary care patients. However, in daily pharmacy practice, the provision of pharmaceutical care appears to be limited. We aimed at quantifying the content of counseling by community pharmacy staff during patient contacts, especially adherence counseling, and at investigating pharmacist views about their practice of adherence counseling.
Patients and methods
A Master’s student in Pharmacy observed patient contacts at selected community pharmacies in the region of Basel, Switzerland. Content of counseling was manually ticked on a checklist with predefined themes (administration, dose, effect, and adherence). Pharmacists working in the pharmacy were interviewed on triggers, topics, and barriers in adherence counseling.
Results
In 20 community pharmacies and during a total of 148.1 hours, 1,866 patient contacts were observed. During the 1,476 patient contacts including the dispensing of one or more medications, counseling was provided to 799 (54.1%) patients; with 735 (49.8%) patients counseled about administration, 362 (24.5%) about dose, 267 (18.1%) about effect, and 99 (6.7%) about adherence. Significantly more patients received counseling when they obtained prescribed versus over-the-counter medication (P=0.002), a new prescription versus a repeat prescription (P<0.001), or when they were served by a pharmacist versus by another staff member (P<0.001). Of the 33 interviewed pharmacists, all except one reported actively approaching patients for adherence counseling. Triggers included medication-related and patient-related factors. The pharmacists named predominantly product-centered topics of adherence counseling. The most cited barriers were rejection of counseling by the patient and lack of time.
Conclusion
Half of the patients receiving one or more medications were counseled, and only 6.7% of all contacts included adherence counseling. Future studies should clarify how barriers to adherence counseling at the community pharmacy can be overcome.
Introduction
Pharmaceutical care has been defined as “…the pharmacist’s contribution to the care of individuals in order to optimize medicines use and improve health outcomes,”Citation1 and the pharmacist has been designated as part of the health care team for added value in the health care system.Citation2–Citation4 Pharmaceutical care activities practiced by community pharmacies have been shown effective in improving medication adherence.Citation5–Citation12 Face-to-face counseling during dispensing of medication is part of pharmaceutical care.Citation4 Counseling can include providing education to patients (eg, about therapy, their condition), intervening in a patient’s drug therapy (eg, optimizing intake times), and ultimately, helping improve medication adherence.Citation13 Previous studies reported significantly improved adherence and persistence through targeted counseling by community pharmacists.Citation14–Citation16
Counseling practice in community pharmacies has been reported to be limited. In a pan-Europe comparison in 2009, the mean total score of pharmaceutical care provision, expressed as a percentage of the total score achievable, ranged from 31.6% to 52.2%.Citation17 Patient counseling was reported to be only a minor task in every day practice in the community pharmacy,Citation18–Citation21 and communication was predominantly nonmedical or product-centered, instead of patient-centered.Citation22–Citation24
At the dispensing of prescription medication, Swiss pharmacists are reimbursed for providing counseling on dose, frequency, administration, duration of use, storage, and potential adverse effects.Citation25 Introduced in 2005, this was the first acknowledgment of cognitive services delivered by community pharmacists to improve the patients’ use of medication. Additionally, the provision of a dose-dispensing aid by the pharmacy is reimbursed.Citation26
To our knowledge, the current counseling practices in Swiss community pharmacies have not yet been addressed, especially the content of adherence counseling. The aim of this study was to quantify the content of counseling by community pharmacy staff during patient contacts, with a specific focus on adherence counseling, and to investigate the views of community pharmacists about their practice of adherence counseling.
Material and methods
Of 106 community pharmacies in the region of Basel, Switzerland, community pharmacies that had participated in previous studiesCitation27,Citation28 were approached consecutively, according to a random number list, until the sample size of 20 was reached. This number was calculated to enable approximately 2,000 patient contacts, assuming that counseling would take 5 minutes and one investigator could observe approximately 100 patients during 8 hours. We did not perform analysis of health communication between pharmacy staff and patients, but rather, we observed and quantified the content of counseling. A Master’s student in Pharmacy observed the patient contacts of the pharmacy staff in sequential order during 1 day at each pharmacy. The observation began at the entrance of one patient into the pharmacy and lasted until the departure of this patient; thereupon, the student observed the next patient who entered the pharmacy. Information about the staff member serving the patient, the number of dispensed medications, and content of counseling were manually ticked on a checklist. The checklist enabled ad hoc coding of the patient contacts by allocation into two categories (“medication on prescription” and “medication over the counter”), as well as the coding of four themes (“administration”, “dose”, “effect”, and “adherence”) and 12 topics of adherence counseling. The latter were deduced from published recommendations ().Citation29 Observation time and characteristics of the pharmacy and the team were simultaneously assessed. At the end of the observation time, an interview was performed with all present pharmacists, consisting of two closed-ended questions (active approach to patients about adherence [yes/no]; frequency of active approach per month) and three open-ended questions (triggers, topics, and barriers in adherence counseling).
Table 1 Definitions and numbers of observed counseling events by counseling themes and topics of explicit adherence counseling
We defined explicit adherence counseling as provision of patient-centered information that directly addresses the spectrum of adherence problems, including unintentional (ie, the patient is physically or cognitively unable to adhere) and intentional nonadherence (ie, the patient is not willing to adhere); this included the use of targeted questioning (“have you missed any pills in the past week”), offer of refill reminders and dose-dispensing aids, reinforcement, etc.Citation29 We defined implicit adherence counseling as provision of product-centered information, eg, information on administration or dose. This information does not directly address adherence but might prevent unintentional nonadherence.
Coded patient contacts were quantified and analyzed statistically within the sample of patients obtaining one or more medications. Answers from the interviews were categorized and analyzed quantitatively. We used SPSS V. 20 (IBM Corp., Armonk, NY, USA) for Windows for descriptive and comparative (χ2-test) calculations. A P-value of ≤0.05 was considered statistically significant. Missing data were excluded from analysis.
Results
During February and March 2010, 21 community pharmacies were approached, 20 took part in the study, and one pharmacy declined participation without specification of a reason. The pharmacies were located in the city center (eight), in residential districts (eight), and in shopping centers (four). Of a median of 9.25 opening hours (range 8.75–11.5), 7.5 hours (range 6.5–7.75) were observed per day and pharmacy. The observation day was equally distributed over the weekdays (Tuesday [five]; Monday, Wednesday, and Thursday [four]; and Friday [three]). The median number of working staff members was two pharmacists, three pharmacy technicians, and one apprentice, respectively.
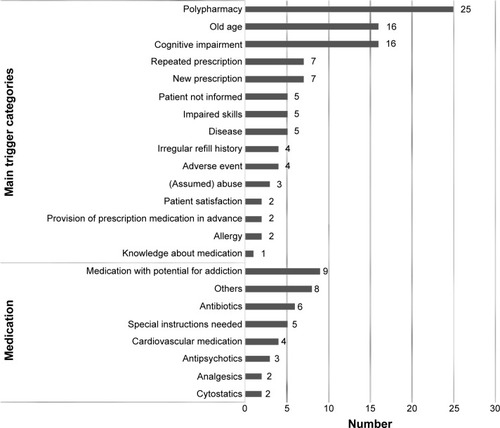
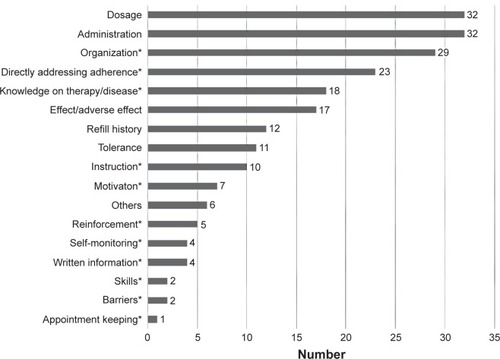
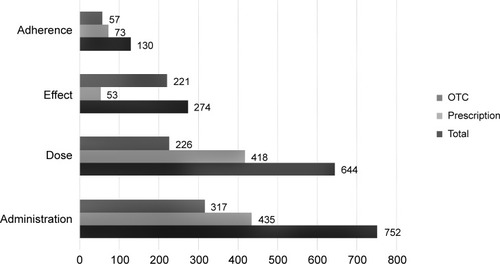
During the total observation time of 148.1 hours, 1,866 patient contacts were observed, of which 21 resulted in a referral to the physician, 18 in further inquiry by phone or fax with the physician, and eight in a refusal of dispensing. A total of 1,476 patient contacts included the dispensing of one or more medications, constituting the basis sample for statistical analysis (). Of 2,789 products dispensed, 1,742 (62.5%) were on prescription and 1,047 (37.5%) were “over the counter” (OTC). Counseling was provided to 799 (54.1%) patients, with 735 (49.8%) patients counseled about administration, 362 (24.5%) about dose, 267 (18.1%) about effect, and 99 (6.7%) about adherence (). The total number of observed counseling events was 1,800, with most patients receiving counseling on two (55.4%) or three (21.2%) themes. Explicit adherence counseling (n=130) mostly included comprehensive instruction (49 [37.7%]) and counseling on knowledge of disease and medication (36 [27.7%]) (). Significantly more patients solely obtaining prescription medication were provided with overall counseling compared with those solely obtaining OTC medication (57.3% vs 50.2%) (χ2=7.1, P=0.002; n=1,402). In the same groups, the single theme “effect” was observed significantly more often in patients contacts with the dispensing of OTC than in patients contacts with the dispensing of prescription medication (31.3% vs 6.3%) (χ2=1483, P<0.001; n=1,402). There was no significant difference in frequency of adherence counseling for prescription vs OTC medication (7.1 % vs 5.9%) (χ2=0.9, P=0.17; n=1,402).
Figure 1 Patient numbers and allocations by category and themes.
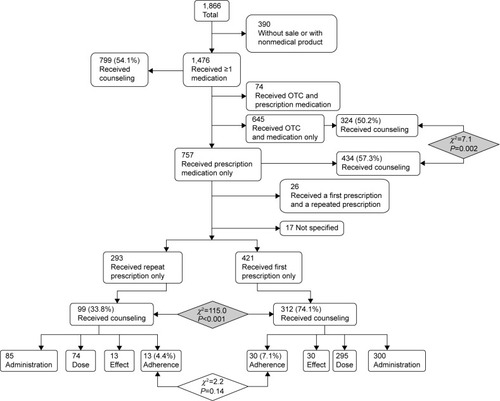
Figure 2 Numbers of observed counseling events about administration, dose, effect, and adherence in total and according to dispensing category (prescription/OTC)
Abbreviation: OTC, over the counter.
Focusing on the 757 patients solely receiving prescription medication, 421 (55.6%) had a new prescription, 293 (38.7%) requested a repeat prescription, 26 (3.4%) had both, and 17 (2.2%) were not specified (). The pharmacy staff provided overall counseling to significantly more patients with new prescriptions compared with patients with repeat prescriptions (74.1% vs 33.8%) (χ2=115.0, P<0.001; n=714). There was no significant difference in frequency of adherence counseling in these two groups (new vs repeat prescriptions: 7.1% vs 4.4%, respectively) (χ2=22, P=0.14).
Of all patients receiving one or more medications (n=1,476), 368 (24.9%) were served by a pharmacist, 1,075 (72.8%) by another staff member (eg, pharmacy technician or apprentice), and 33 (2.2%) by a combination of both. Significantly more patients received counseling when they were served by a pharmacist compared with other staff members (62.1% vs 51.2%) (χ2=14.1, P<0.001). Adherence counseling was provided to twice as many patients when served by a pharmacist compared with other staff members (10.7% vs 5.2%) (χ2=14.2, P<0.001).
Of 390 patients who did not receive a medication at the observed contact (eg, buying dose-dispensing aids, ordering out-of-stock medication), 42 (10.8%) received counseling.
Interview
Among the 20 community pharmacies, 33 pharmacists participated in the interview (a median of two and range of one to three pharmacists per pharmacy) and were mainly women (69.7%), with a median age of 41 (range 25–68) years and a median duration of 14 (range 1–43) years after university graduation. They worked with a median of 90% employment at the community pharmacy (range 40%–100%). All pharmacists except one reported actively asking patients about their adherence, and 20 (60.6%) did so on a daily basis. and illustrate named triggers and topics of adherence counseling. Barriers included rejection by the patient (15 [45.5%]), lack of time (12 [36.4%]), lack of patient data (seven [21.2%]), lack of checklists and demo material (six [18.2%]), lack of confidential room (five [15.2%]), lack of remuneration (three [9.1%]), and “Other” (19 [57.6%]).
Discussion
Counseling was provided to half of the patients receiving one or more medications and occurred more frequently when the medication was on prescription, on a new prescription, or if patients were served by a pharmacist. The content of the counseling mostly included information on medication administration and dose. Only 6.7% of the patients obtaining medication received explicit adherence counseling, significantly more of them if the pharmacist was involved in the dispensing. However, most pharmacists seemed motivated to provide adherence counseling. They named a lot of triggers but also barriers to start adherence counseling and mostly named topics for adherence counseling, which only implicitly addressed the issue.
Due to easy access, regular patient visits, the possibility to monitor medication refill frequency, and the competences of the pharmacist, the community pharmacy seems to be a predestined place for counseling about adherence. In our study, we showed that if pharmacy staff counseled, they counseled about more than one theme, indicating motivation and assumption of responsibility for safe and effective medication management. If only looking at prescription medication, unsurprisingly, dispensing of first prescriptions largely predominated in the number of patients provided with counseling. A considerable percentage (74.1%) of these patients were counseled. Apart from the need to ensure the patient’s knowledge at first use, the patient filling a first prescription also seems to expect more counseling, which might result in facilitating counseling.Citation30 Still, explicit adherence counseling accounts for a very small part in both situations, in the dispensing of a new prescription and in the dispensing of a repeat prescription. Because the pharmacist is able to detect nonadherence in patients with long-term therapy, eg, by analyzing medication refill frequency, we expected adherence counseling to occur more in patients with repeat prescriptions.
Evidence that community pharmacy interventions have been successful in improving health outcomes and adherence have accumulated,Citation5–Citation10,Citation12,Citation31–Citation34 and two Cochrane reviews concluded that the pharmacists’ cognitive services were beneficial for safe and effective medication use.Citation3,Citation11 However, our study confirms results of earlier studies showing that community pharmacies provided limited pharmaceutical care services,Citation17,Citation19,Citation35–Citation37 indicating a problem of implementation in daily practice. Studies on counseling in community pharmacies were conducted using patient and pharmacist surveys, observation, and simulated patient visits.Citation38,Citation39 They mostly reported on pharmacists’ behavior only, with a total counseling rate of 8%–100%.Citation39 Similar to our study, predominant categories of counseling were administration and dose, and hence were more product- than patient-centered.Citation22–Citation24,Citation39 A large proportion of communications (26%–40%) between pharmacists and patients was reported to be nonmedical.Citation36,Citation37 The only observational study specifically investigating adherence counseling was performed with pharmacy students, who had a lack of specific training in adherence management and of resources, and therefore reported not to address adherence in counseling sessions.Citation40 A German study showed that pharmacists documented “evidence of nonadherence” in only 1.6% of all assessed drug-related problems during patient contacts in community pharmacies, indicating that the pharmacists had difficulties in identifying nonadherence.Citation41
We showed that pharmacists provided more counseling than pharmacy staff, which confirms the results of another study.Citation35 Differences may arise from the more detailed knowledge about therapy and disease, more intense training, and from the assumption of the responsibility for safe and effective medication use by the patients. This knowledge and attitude, however, should be transferred to the whole pharmacy team.
In our study, the comparison of observed counseling practice (observed adherence counseling of 6.7%) with pharmacists’ interview responses (60.6% indicated actively approaching patients with adherence issues every day) reveals a discrepancy between our definition and the pharmacists’ opinions about the topics of adherence counseling. We defined the topics more explicitly, whereas the most frequently named topics by the pharmacists were implicit. Several problems could arise from the implicit approach. First, the patients might not understand the purpose of the counseling and reject it. Second, while some unintentional nonadherence problems might be clarified with counseling on administration and dose, intentional nonadherence might be completely overlooked. Literature has described habits of pharmacists mainly asking standardized questions, eg, “Do you have any questions?”; at the same time, authors have suggested a more considerate and individualized approach according to patients’ needs, and the necessity of engaging patients in counseling.Citation24,Citation42,Citation43 Such an approach would include a more direct addressing of adherence. Further, almost all topics on our predefined list of explicit adherence counseling were named by the pharmacists, indicating that they were familiar with most of the topics, though less frequently addressed them during the observed patient contacts.
The most frequently reported barrier was rejection of the offered counseling by the patients. This has also been shown in other studies, with 41%–63% of patients declining offered counseling.Citation30,Citation36 Expectations of patients have been shown to not coincide with the recent development of the pharmacist’s role.Citation43,Citation44 Qualitative studies reported patient tendency to rely solely on the physicians, recommendations and to deny the pharmacists’ competences.Citation45,Citation46 This attitude persisted even in patient-centered consultationsCitation47 and was confirmed by a recent study that collected data over 15 years.Citation48
It seems logical that patients with prescribed medications obtain more counseling, on one hand because the medication plan usually is more complex, including long- and short-term medication for serious diseases, and hence counseling might be more relevant. On the other hand, the counseling about prescribed medication is remunerated by a medication tax of CHF 4.20 (= US$ 4.60) per prescribed item. Nevertheless, lack of adequate remuneration was only named by 9.1% of the pharmacists as barrier for adherence counseling. Remarkably, counseling was also given without product sale.
Apart from the structural factors discussed above, several procedure-related factors were identified, which hinder pharmacists in counseling, and patients in asking questions. Time constraints pose such a barrier.Citation40,Citation48–Citation50 However, surveys on pharmacists’ activities revealed that pharmacists were mainly occupied with traditional product-centered activities, such as business management, logistics, and product assembly, than with patient-centered activities, like counseling.Citation18–Citation21 In our study, we observed that pharmacists had fewer patient contacts in relation to their presence compared with the rest of the staff. Consequently, the problem could be designated as time mismanagement, and reconsiderations of staffing and of assignment of responsibilities might be a solution.
Another barrier to patient-centered, individualized counseling is the lack of privacy, named by the pharmacists in our study and also reported elsewhere.Citation35,Citation45,Citation50 Most people certainly are uncomfortable discussing their sensitive health problems next to a line of others at the counter. The traditional conceptualization of the pharmacy accommodations reminds patients more of a shopCitation46 than of a health care center and hence is not supportive in promoting counseling.
The limitations of our study firstly include the restriction to one region in Switzerland. Secondly, the methodology of observation has been reported to yield variable results but a more holistic picture of counseling practice.Citation39 We chose a minimally obtrusive method to observe the counseling, in order to prevent the introduction of biases. However, the open approach of the pharmacies and the presence of an observer could have triggered pharmacy staff to engage more in counseling practice than usual (Hawthorne effect).Citation51 Thirdly, the ad hoc coding without review by a second person could have limited the results’ reliability. Fourthly, due to the observational setting, we could not evaluate the rate of overall offered counseling. With the most named barrier for adherence counseling being the rejection of counseling by the patients, we can assume higher counseling rates at higher acceptance of counseling.
Conclusion
The unique position of the community pharmacy in the health care chain and the competencies of pharmacists make the community pharmacy a predestined place for medication and adherence counseling. Pharmacists are motivated to provide counseling but experience several structural and procedural barriers in delivering it. In our study, half of patients collecting one or more medications received counseling, which was predominantly product-centered, and only 6.7% of the patients received adherence counseling. This study revealed insufficient knowledge and gaps in the provision of explicit adherence counseling by pharmacists. Future studies should explore the pharmacist–patient interaction in depth and clarify how barriers to adherence counseling in the community pharmacy can be overcome.
Author contributions
All authors participated in conceptualizing the study. FB analyzed data and drafted the manuscript. IA and KEH revised the manuscript critically for intellectual content.
Acknowledgments
We would like to thank Irene Rüfenacht (MSc Pharm) for her participation in conceptualization of the project and data collection, and Gülistan Karatas (MSc Pharm) for data entry.
Disclosure
The authors report no conflicts of interest in this work.
References
- AllemannSSvan MilJWBotermannLBergerKGrieseNHersbergerKEPharmaceutical care: the PCNE definition 2013Int J Clin Pharm201436354455524748506
- Chisholm-BurnsMAKim LeeJSpiveyCAUS pharmacists’ effect as team members on patient care: systematic review and meta-analysesMed Care2010481092393320720510
- RyanRSantessoNLoweDInterventions to improve safe and effective medicines use by consumers: an overview of systematic reviewsCochrane Database Syst Rev20144CD00776824777444
- Joint FIP/WHO Guidelines on GPP: Standards for Quality of Pharmacy ServicesWorld Health Organisation Fédération Internationale Pharmaceutique2011 Available from: http://www.fp.org/www/uploads/database_file.php?id=331&table_id=,2014Accessed January 8, 2015
- Obreli-NetoPRGuidoniCMde Oliveira BaldoniAEffect of a 36-month pharmaceutical care program on pharmacotherapy adherence in elderly diabetic and hypertensive patientsInt J Clin Pharm201133464264921544559
- van BovenJFStuurman-BiezeAGHiddinkEGPostmaMJVegterSMedication monitoring and optimization: a targeted pharmacist program for effective and cost-effective improvement of chronic therapy adherenceJ Manag Care Pharm2014208786792
- PringleJLBoyerAConklinMHMcCulloughJWAldridgeAThe Pennsylvania Project: pharmacist intervention improved medication adherence and reduced health care costsHealth Aff (Millwood)20143381444145225092847
- Rubio-ValeraMSerrano-BlancoAMagdalena-BelíoJEffectiveness of pharmacist care in the improvement of adherence to antidepressants: a systematic review and meta-analysisAnn Pharmacother2011451394821205952
- JarabASAlqudahSGKhdourMShamssainMMukattashTLImpact of pharmaceutical care on health outcomes in patients with COPDInt J Clin Pharm2012341536222101426
- LeeJKGraceKATaylorAJEffect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trialJAMA2006296212563257117101639
- NkansahNMostovetskyOYuCEffect of outpatient pharmacists’ non-dispensing roles on patient outcomes and prescribing patternsCochrane Database Syst Rev20107CD00033620614422
- van DalemJKrassIAslaniPInterventions promoting adherence to cardiovascular medicinesInt J Clin Pharm201234229531122271222
- ChandraAMalcolmNFettersMPracticing health promotion through pharmacy counseling activitiesHealth Promot Pract200341647114610974
- TaitelMJiangJRudkinKEwingSDuncanIThe impact of pharmacist face-to-face counseling to improve medication adherence among patients initiating statin therapyPatient Prefer Adherence2012632332922563240
- CliffordSBarberNElliottRHartleyEHorneRPatient-centred advice is effective in improving adherence to medicinesPharm World Sci200628316517017004019
- ZolnierekKBDimatteoMRPhysician communication and patient adherence to treatment: a meta-analysisMed Care200947882683419584762
- HughesCMHawwaAFScullinCProvision of pharmaceutical care by community pharmacists: a comparison across EuropePharm World Sci201032447248720458539
- BellHMMcElnayJCHughesCMA self-reported work sampling study in community pharmacy practicePharm World Sci199921521021610550845
- McCannLHughesCMAdairCGA self-reported work-sampling study in community pharmacy practice: a 2009 updatePharm World Sci201032453654320559729
- SchommerJCPedersenCADoucetteWRGaitherCAMottDACommunity pharmacists’ work activities in the United States during 2000J Am Pharm Assoc (Wash)200242339940612030625
- DaviesJEBarberNTaylorDWhat do community pharmacists do?: results from a work sampling study in LondonInt J Pharm Pract201422530931824423212
- HassellKNoycePRogersAHarrisJWilkinsonJAdvice provided in British community pharmacies: what people want and what they getJ Health Serv Res Policy19983421922510187202
- ChongWWAslaniPChenTFPharmacist-patient communication on use of antidepressants: a simulated patient study in community pharmacyRes Social Adm Pharm201410241943723787139
- SleathBPharmacist-patient relationships: authoritarian, participatory, or default?Patient Educ Couns19962832532638852101
- Tarifvertrag (LOA IV) zwischen dem Schweizerischen Apothekerverband (pharmaSuisse) und santésuisse – Die Schweizer Krankenversicherer (santésuisse) [Labor agreement between the Swiss Pharmacist Association and the Association of Swiss Health Insurances]LiebefeldSolothurn2009 [cited January 26, 2015]. Available from: http://www.pharmasuisse.org/data/Oeffentlich/de/Themen/Tarifvertrag_LOA-IV_def_d_09-03-6.pdfAccessed January 26, 2015 German
- GuignardEBugnonOPharmaceutical care in community pharmacies: practice and research in SwitzerlandAnn Pharmacother200640351251716467249
- EichenbergerPMLampertMLKahmannIVvan MilJWHersbergerKEClassification of drug-related problems with new prescriptions using a modified PCNE classification systemPharm World Sci201032336237220229029
- MengiardiSTsakirisDAMolnarVImpact of pharmaceutical care on self-administration of outpatient low-molecular-weight heparin therapyPharmacol Pharm201454372385
- HaynesRBMcDonaldHPGargAXHelping patients follow prescribed treatment: clinical applicationsJAMA2002288222880288312472330
- PuspitasariHPAslaniPKrassIPharmacists’ and consumers’ viewpoints on counselling on prescription medicines in Australian community pharmaciesInt J Pharm Pract201018420220820636671
- CliffordRMDavisWABattyKTDavisTMFremantle Diabetes StudyEffect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: the Fremantle Diabetes StudyDiabetes Care200528477177615793171
- PaulósCPNygrenCECeledónCCárcamoCAImpact of a pharmaceutical care program in a community pharmacy on patients with dyslipidemiaAnn Pharmacother200539593994315827075
- HohmannCKlotzJMRadziwillRJacobsAHKisselTPharmaceutical care for patients with ischemic stroke: improving the patients quality of lifePharm World Sci200931555055819633917
- RougheadEESempleSJVitryAIPharmaceutical care services: a systematic review of published studies, 1990 to 2003, examining effectiveness in improving patient outcomesInt J Pharm Pract20051315370
- KimberlinCLJamisonANLindenSWintersteinAGPatient counseling practices in U.S. pharmacies: effects of having pharmacists hand the medication to the patient and state regulations on pharmacist counselingJ Am Pharm Assoc (2003)201151452753421752776
- KaaeSMygindASaleemSA characterization of the current communication patterns in Danish community pharmacies – an observational studyRes Social Adm Pharm20139695896423131663
- OlssonEIngmanPAhmedBKälvemark SporrongSPharmacist-patient communication in Swedish community pharmaciesRes Social Adm Pharm201410114915523591412
- SchommerJCSullivanDLWiederholtJBComparison of methods used for estimating pharmacist counseling behaviorsJ Pharm Technol199410626126810138739
- PuspitasariHPAslaniPKrassIA review of counseling practices on prescription medicines in community pharmaciesRes Social Adm Pharm20095319721019733821
- ManganMNPowersMFLengelAJStudent pharmacists’ perceptions of barriers to medication adherence counselingJ Pharm Pract201326437638123178413
- NicolasAEickhoffCGrieseNSchulzMDrug-related problems in prescribed medicines in Germany at the time of dispensingInt J Clin Pharm201335347648223605073
- KaaeSTraulsenJMNørgaardLSChallenges to counseling customers at the pharmacy counter – why do they exist?Res Social Adm Pharm20128325325721955809
- ShahBKChewningBConcordance between observer reports and patient survey reports of pharmacists’ communication behaviorsRes Social Adm Pharm20117327228021371946
- RenbergTWichman TörnqvistKKälvemark SporrongSKettis LindbladATullyMPPharmacy users’ expectations of pharmacy encounters: a Q-methodological studyHealth Expect201114436137321199199
- CocohobaJComfortMKianfarHJohnsonMOA qualitative study examining HIV antiretroviral adherence counseling and support in community pharmaciesJ Manag Care Pharm201319645446023806059
- KaaeSTraulsenJMNørgaardLSCustomer interest in and experience with various types of pharmacy counselling – a qualitative studyHealth Expect201417685286223020683
- SalterCHollandRHarveyIHenwoodK“I haven’t even phoned my doctor yet.” The advice giving role of the pharmacist during consultations for medication review with patients aged 80 or more: qualitative discourse analysisBMJ20073347603110117449504
- SchommerJCGaitherCAA segmentation analysis for pharmacists’ and patients’ views of pharmacists’ rolesRes Social Adm Pharm201410350852824268770
- SchommerJCWiederholtJBA field investigation of participant and environment effects on pharmacist-patient communication in community pharmaciesMed Care19953365675847760574
- SchommerJCWiederholtJBPharmacists’ perceptions of patients’ needs for counselingAm J Hosp Pharm19945144784858017412
- Delgado-RodríguezMLlorcaJBiasJ Epidemiol Community Health200458863564115252064