Abstract
Background
Medication can ease symptoms and limit disease progression in rheumatoid arthritis (RA). Despite this, nonadherence to medication is common in RA. We explored the determinants of high and low adherence to disease-modifying antirheumatic drugs (DMARDs) in patients with RA and provide suggestions on approaches to improving adherence to DMARDs.
Methods
Patients with RA were identified from those who had previously participated in a questionnaire measuring levels of medication adherence. Twenty patients participated (ten high and ten low adherers, as determined by responses to the Medication Adherence Report Scale). In-depth individual semistructured interviews were undertaken until data saturation was reached. Interviews were transcribed and analyzed using a constant comparative method.
Results
Four main themes related to adherence were identified: 1) symptom severity; 2) illness perception; 3) perceived benefits and risks of DMARDs; and 4) the quality and quantity of information about RA and DMARDs. In addition, patients’ suggestions about strategies to optimize adherence to DMARDs were captured and they fell within the following themes: 1) musculoskeletal ultrasound to explain the disease process and to provide objective feedback about the extent to which their disease activity is being effectively controlled; 2) better explanations of the consequences of poorly controlled RA; and 3) a good relationship with the health professional.
Conclusion
Patients’ beliefs about medicines, perceptions about RA, and level of satisfaction with information about DMARDs influenced their adherence to DMARDs. The use of musculoskeletal ultrasound to image the inflamed joint may help to improve patient adherence to DMARDs.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease characterized by synovitis and associated with joint destruction.Citation1 RA causes progressive decline in functional ability and limits participation in social and work-related activities.Citation2 RA is also associated with an increased risk of extra-articular complications including ischemic heart disease.Citation3 While curative therapies are not currently available, treatments with disease-modifying antirheumatic drugs (DMARDs) and biologic agents improve joint function,Citation1 work productivity,Citation4 and health-related quality of life, reducing the risk of joint destruction, disability, and morbidity and improving the life expectancy.Citation5 Despite these treatments, many patients fail to achieve optimal disease control, in part, due to nonadherence.Citation6
The World Health Organization defines adherence as “the extent to which the patient’s behavior coincides with the health professional’s advice”.Citation7 Nonadherence to medication remains a major problem across the spectrum of chronic diseases.Citation8,Citation9 Factors associated with poor medication adherence are complex.Citation7 In RA, only a small proportion of the variance in adherence is explained by demographic characteristics which are largely unchangeable,Citation10 therefore necessitating the identification of other modifiable factors that could be changed.Citation11,Citation12 It is widely reported that patients’ beliefs about medicines can have a major impact on their decision to take them.Citation13–Citation15
Medication-taking behavior might be enhanced by a better understanding of the types of belief that are associated with poor adherence.Citation16 This understanding can be obtained by employing the Necessity–Concerns Framework (NCF)Citation16 and the Self-Regulatory Model (SRM)-Common Sense Model (CSM).Citation17 The SRM-CSM/NCF framework allows researchers to see how adherence is associated with the ways in which patients judge their personal need for their prescribed medicines relative to their concerns about possible side effects.Citation11,Citation15 Studies across long-term conditions including RA have demonstrated the utility of the SRM-CSM/NCF with nonadherence related to doubts about personal need for treatment and concerns about side effects.Citation11,Citation15 Patients’ judgment about prescribed medications may be influenced by more general attitudes to medicines as a whole, for example, perceptions that medicines are harmful, addictive, and poisonous and are overused by doctors.Citation18 Negative attitudes and beliefs about DMARDs appear more prevalent within certain ethnic groups including the South Asian population where many patients have negative attitudes toward DMARDs.Citation19 However, those studies that report data on the impact of beliefs about medicines on adherence have not included South Asian patients with RA.Citation13–Citation15,Citation20 Health care professionals managing patients with RA need to understand the influence of health beliefs on medication adherence, as nonadherence is costly.Citation10 As part of a questionnaire study examining determinants of medication adherence in patients of White British and South Asian origin,Citation21 we explored the views about DMARDs and the determinants which influence medicine-taking by patients with RA. In addition, we documented patients’ suggestions about adherence-enhancing strategies.
Materials and methods
Ethical approval for this study was granted by the South Birmingham Research Ethics Committee, and all patients gave written informed consent.
The study took place at Sandwell and West Birmingham Hospitals NHS Trust and University Hospitals Birmingham NHS Foundation Trust, UK. Patients were selected from those who had participated in a previous questionnaire study of 180 patients with RA.Citation21 Patients in that cross-sectional study had had a diagnosis of RA (according to the 1987 American College of Rheumatology criteria)Citation22 for at least 3 months, were aged 18 and over, and were taking at least one DMARD or had taken a DMARD in the past.
Patients were selected purposively to ensure a mixture of age, sex, language spoken, and employment status ().Citation21
Table 1 Demographic data of the patients interviewed
All 180 patients who had taken part in the questionnaire study were given a questionnaire (Medication Adherence Rate Score)Citation15 that measured self-reported medication adherence. “High” adherence was defined as a Medication Adherence Rate ScoreCitation15 in the upper tertile () and “low” adherence as a score in the lowest tertile. Patients in the middle tertile were excluded. There were 50 high-adhering patients (White British 33, South Asian 17) and 62 low-adhering patients (White British 23, South Asian 39); and from these 112 patients, 36 were invited by mail for an interview. Patients who responded to letters were recruited into the study (high adherers: ten White British, eight South Asians; low adherers: six White British, 12 South Asians); 16 declined.
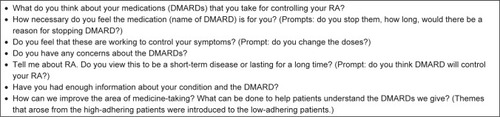
A group of Patient Research Partners were part of the steering committee that helped with the development of the topic prompt (). The topic guide was organized around questions broadly based on the NCF, SRM,Citation14 and patient satisfaction with information about DMARDs. Initial questions were general (eg, “What do you think about your DMARDs?”), and were followed by prompts based on the NCF (eg, “How necessary do you feel the DMARD(s) is for you?” and “Do you have any concerns about DMARDs?”). In addition, questions were asked about the patients’ adherence or nonadherence to DMARDs, including stopping and changing the doses of DMARDs and reasons for doing so. Patients’ recommendations as to how adherence could be improved were also elicited.
Figure 1 Topic guide based on SRM-CSM and NCF (questions asked during the interviews).
Individual interviews with patients were conducted at two hospitals in areas designated for research, away from their routine clinical setting. The interviews were undertaken by KK who was fluent in both English and Punjabi. Five patients chose to be interviewed in Punjabi. Recruitment and interviewing continued until data saturation had been reached in both groups.
Each interview lasted approximately 1 hour. All interviews were audio-taped and transcribed verbatim by KK. A selection of English transcriptions was independently checked for emerging themes by KK, PG, and SG. A sample of the English-translated transcripts from Punjabi-speaking patients was validated for accuracy by an independent health professional (AJ). Any discrepancies regarding themes were discussed and agreed. The overall analysis was organized by labeling data relevantCitation23 to each of the questions in the topic guide and then grouping similar themes.Citation24 Constant comparisonCitation25 was used to analyze the transcripts line by line, comparing the themes related to high- and low-adhering patients’ views about DMARDs.Citation25 Particular emphasis was placed on comparing determinants influencing medicine-taking that differed between ethnic groups. Data on strategies that were recommended by high-adhering patients to help improve the area of medication adherence for patients with RA were identified.
Results
Twenty interviews were conducted (with ten high-adhering patients and ten low-adhering patients). Fourteen participants were female and eight were in full-time employment. Fifteen were interviewed in English and five in Punjabi. Four themes related to adherence were identified in both high- and low-adhering patients: 1) symptom severity; 2) illness perception; 3) perceived benefits and risks of DMARDs; and 4) the quality and quantity of information about RA, DMARDs, and the need for DMARDs. In addition, patients’ suggestions about strategies to optimize adherence to DMARDs were captured () and they fell within the following themes: 1) visual representations to explain the disease process and to provide objective feedback about the extent to which their disease activity is being effectively controlled; 2) better explanations of the consequences of poorly controlled RA; 3) a good relationship with the health professional; and 4) access to patient support groups. Each theme is illustrated with quotations from the transcripts. The data from high-adhering patients are presented first.
Table 2 Comparison of themes and subthemes by adherence level
Results from patients with high adherence
Symptom severity
Seven patients perceived RA medication to be very important; this was related to patients’ current experience of symptoms and their recollection of severe symptoms at disease onset (Quote 1). They were also aware that uncontrolled RA could lead to future health problems (Quote 2). As a result of both symptom severity and awareness of future risks, the high-adhering patients viewed RA medicines to be important. Family history of RA appeared to increase the level of importance in four of the patients. (Quote 3).
Quote 1: I will take this medication for the rest of my life. I wouldn’t stop taking them just to test it out. I just don’t want to go where I was. [59, retired, English speaking, White patient]
Quote 2: I have no doubt in my mind that if I stop taking these medications then I know that I would be in a wheelchair. [34, nurse, English speaking, Asian patient]
Quote 3: I have had experience of my mother. She had exactly the same problem as me. She really suffered. I saw her disease develop over time. That really put the fright in me. [34, nurse, English speaking, Asian patient]
Illness perception
Regarding patients’ views about RA, all ten high-adhering patients identified a range of factors that they felt had caused their RA, but none believed that the disease was a transient illness or was curable. They all accepted the need for long-term therapy (Quote 4) and held the belief that taking DMARDs regularly would help to control the disease (Quotes 5 and 6).
Quote 4: I doubt it very much that it can be cured yes it can be controlled. [62, retired, English speaking, White patient]
Quote 5: When I went to my first appointment with the nurse and the way she was talking it seemed I would be on methotrexate for very long time don’t know … may be even for the rest of life because there isn’t a cure for this is there? [52, retired, English speaking, White patient]
Quote 6: I have watched my cousin with this arthritis after twenty years he still has it you know … so I know it’s not going to go away. [51, off work due to RA, English speaking, Asian patient]
Perceived benefits and risks of DMARDs
Nine patients described their DMARD(s) as working to control their RA. Patients made decisions by weighing up the benefits and concerns and/or perceptions about the efficacy of treatment. For example, those who were taking anti-tumor necrosis factor (TNF) therapy (six patients) believed that their lives had been transformed through taking this class of drug and that it was more effective in controlling their symptoms than their previous nonbiologic DMARDs. This view emerged from both White British and South Asian patients (Quotes 7 and 8). The patients who viewed their medicines as necessary (all ten patients) expressed fewer concerns about medicines and did not question the necessity of DMARDs (Quote 9). This appraisal was based on the theme related to symptom severity and views about control rather than cure. Five patients gave examples of their past experiences of stopping medication and how the decision to discontinue DMARDs for a while had led to disease flares (Quotes 10 and 11). The remaining five gave examples of the persistent presence of RA symptoms. These evaluations helped to form beliefs about the necessity of DMARDs and these patients reported that they were now completely adherent to DMARDs.
Quote 7: Rituximab has transformed my life now. The rheumatoid arthritis has kept under control since I have started on that. [62, retired, English speaking, White patient]
Quote 8: Initially I couldn’t even bend my knees I couldn’t do my household chores, since I have been on methotrexate …. Yes I can do these now. I am a paediatric nurse and I am on my feet all the time. So for me to take the medicines is very important. [36, manager, English speaking, Asian patient]
Quote 9: I think that sometimes you think I am taking all these medicines … like methotrexate they could damage your kidneys your liver … but I would rather have that danger rather than how I was before. So the dangers of the drugs that I hear mean nothing to me because I want to be how I am now. [52, house wife, English speaking, White patient]
Quote 10: I stopped it for a while [methotrexate] but my flare had come back so I knew I had to take it. [36, manager, English speaking, Asian patient]
Quote 11: I know this would get worse you see. It’s there all the time and stopping the medication will make it worse. [42, machine operator, English speaking, White patient]
A range of concerns about DMARDs appeared to be related to the different types of DMARDs used. For example, concerns about short- and long-term side effects of their current DMARDs and their previous experiences of side effects were mentioned by all ten patients. Three patients expressed the view that taking DMARDs was like taking poison and viewed these drugs to be “unnatural”. One South Asian patient viewed methi (an Indian herb) and ginger to be more natural than DMARDs (Quote 12). However, despite these concerns, the drivers for the need for DMARDs led the patients to take their DMARDs as prescribed (Quote 13). Three of the patients expressed that DMARDs were less serious than some other therapies such as certain cancer treatments (Quotes 14–16) and this promoted adherence to DMARDs.
Quote 12: I do try and take methi (Indian herb) and ginger. I have fresh ginger every day to help get rid of the toxins (swelling in joints). [51, off work due to RA, Punjabi speaking, Asian patient]
Quote 13: I really hate this medication [methotrexate]. But I appreciate that I need to take it I guess it’s a reasonable compromise. [62, retired, English speaking, White patient]
Quote 14: I thought look … there are people on cancer medicine where their hair falls out and I am not that bad to take these. [42, machine operator, English speaking, White patient]
Quote 15: You know, at least I haven’t got cancer its only arthritis. [52, house wife, English speaking, White patient]
Quote 16: I mean at least it wasn’t leukaemia or something, you know. I mean touch wood I mean it’s not bad as that. I mean it is bad but you know … cancer is a bad thing to have. [55, unemployed, English speaking, White patient]
Quality and quantity of information
When patients were asked about what information they found useful as a basis for their decisions to take DMARDs, they gave a range of spontaneous responses. Eight patients believed that seeing an ultrasound scan of one of their inflamed joints had helped them to understand the nature and extent of their disease. These patients stated that they were less likely to stop taking their DMARDs after having seen imaging evidence of synovitis (Quotes 17–20). The images also helped patients to understand the seriousness of the condition (Quote 21). Two patients made reference to ultrasound scans and plain radiographs as having helped them not only to understand the nature of the disease but also to accept the condition.
Quote 17: Dr XX scanned my joints and he showed me my joints and that helped me understand what was going on in my joints. He explained what was happening … there were different lights flashing and red was showing swelling in the joints. [42, machine operator, English speaking, White patient]
Quote 18: The scan pictures really helped me to understand the disease and to be honest this really motivates me to take the methotrexate. You see I know why I have got to do it. [36, manager, English speaking, Asian patient]
Quote 19: The scan showed me the lights flashing on my joint swelling. It made me scared and helped me to know how serious the condition can be. [51, off work due to RA, Punjabi speaking, Asian patient]
Quote 20: … but when she showed me the X-rays I understood the reasons for my pain and also saw the damage that the disease had caused. [55, unemployed, English speaking, White patient]
Quote 21: When I saw the X-rays and the damage I thought you know … I need to listen to what is being said and accept this is for life. So I am taking my medication and slowly here I am today not that bad. [34, nurse, English speaking, Asian patient]
Quote 22: It really makes a difference when you can get on with your doctors. Mine explained the disease really well. [42, machine operator, English speaking, White patient]
Quote 23: Yeh I mean it makes it easier when the team support is there it makes you feel that you are not alone and there is support there you know. It does make the journey that much easier otherwise you get lost and we take so many medicines. [36, manager, English speaking, Asian patient]
For some patients (six patients), changes in the measured disease activity parameters (blood tests, disease activity score) produced a positive effect in terms of accepting the need for continuous DMARDs. For others (four patients), a positive view about taking DMARDs was facilitated by a good relationship with health professionals and an in-depth explanation of the nature of the disease (Quote 22), in particular RA severity and long-term consequences and explanations about the treatment options available (Quote 23). Information leaflets and use of the Internet were also identified as useful sources of information (four patients), though others (six patients) stated that the leaflets on RA that they had been given did not effectively communicate the seriousness of the disease and were not helpful in visualizing how untreated synovitis could damage joints. Good explanations regarding the seriousness of the disease, ultrasound scans of joints, support by health professionals, and a good explanation of the fluctuating nature of the disease all acted as factors that motivated patients to begin and continue to take DMARDs.
Results from patients with low adherence
Symptom severity
Some low-adhering patients had similar experiences to high-adhering patients regarding their symptom severity (Quote 24). However, there were five patients (all South Asian) in whom symptom experiences were mild (patient’s view) at the beginning and as the treatment gave them relief, their reaction was to stop the medication as they thought that the disease had been cured (Quote 25).
Quote 24: I was in so much pain and I thought gosh I would die rather than staying in bed like that … it was bad. [44, microbiologist, English speaking, Asian patient]
Quote 25: When I started on methotrexate I was well for about five years. Because I was well for so many years and I didn’t really have any pain I made myself believe that the disease has cured. [69, retired, Punjabi speaking, Asian patient]
Illness perception
In contrast to high-adhering patients, some of the low-adhering patients held the view that the disease was curable and saw medication as a short-term therapy. This was particularly the case among the South Asian patients (Quotes 26 and 27). Furthermore, their decisions to take medication were based on their perception of RA (Quotes 28 and 29). One South Asian patient had stopped methotrexate to try herbal treatment instead.
Quote 26: For a year I really battled with myself. Even to now this day I believe that the disease can be cured … it will get better. [33, self-employed, English speaking, Asian patient]
Quote 27: I have been taking them for a year and now you would think that this could be cured … but it hasn’t. [69, retired, Punjabi speaking, Asian patient]
Quote 28: To be honest I thought I am 33 so maybe I am getting old or something. I mean this is only old person disease right … I mean, for arthritis, people live with it they don’t take long-term medicines. [33, self-employed, English speaking, Asian patient]
Quote 29: You see I never heard of arthritis well, I didn’t think it would be in a young person like me. So I thought at the time I would be on paracetamol and it would go away. [61, housewife, Punjabi speaking, Asian patient]
Perceived benefits and risks of DMARDs
Although the low-adhering patients viewed DMARDs as necessary and agreed that these medications were helpful in maintaining their function, they also had concerns. In South Asian patients, fears about dependency led them either to miss doses or to stop treatment temporarily (Quotes 30 and 31). The increased concern about side effects and dependency was partly linked to limited knowledge of the disease; again, this was mainly noted in South Asian patients. Some South Asian patients believed that the long-term usage of DMARDs could lead to additional physiological abnormalities (Quote 32). Three patients stated that medicines were poisonous (Quote 33). Two White British low-adhering patients viewed biologic agents such as anti-TNF to be important, but stated that they often missed doses of their nonbiologic DMARDs (Quotes 34 and 35).
Quote 30: I don’t like taking them (methotrexate) like the biggest thing for me is the hair loss you know. [44, microbiologist, English speaking, Asian patient]
Quote 31: I know that if I take these everyday then I am dependant on them for the rest of my life. [37, legal secretary, English speaking, Asian patient]
Quote 32: I read that these tablets can give you gastric problems. Then you have to take more tablets it’s a never stopping process. [41, off work due to RA, Punjabi speaking, Asian patient]
Quote 33: You see these are not natural. I know I have to take them but they are poisons. When I don’t need them I stop them for a while. [61, house wife, Punjabi speaking, Asian patient]
Quote 34: I am on Humira and this keeps my disease under control. I don’t think I should keep taking my methotrexate when I am controlled more on this drug [Humira]. [41, social worker, English speaking, White patient]
Quote 35: I will be honest with you … since I have been on these injections [anti-TNF therapy] I really think back why was I even taking these other ones [sulphasalazine]. [63, retired, English speaking, White patient]
Quality and quantity of information
The reasons for low adherence to DMARDs were linked to a lack of understanding about RA in six patients (Quotes 36 and 37); this was particularly noted among the South Asian patients. The majority of South Asian patients attributed their poor adherence to DMARDs, in part, to the fact that they felt that RA was not generally well known or taken seriously within the South Asian community (Quote 2). Five South Asian patients held the view that arthritis was a disease of the elderly and they did not understand the need for long-term therapy. Furthermore, the South Asian patients had very little understanding of the fluctuating pattern of the disease (Quote 38). Patients expected more information from their health professionals and felt that they were not always as aware of disease parameters as they would like to be (Quote 39). When asked whether they had experienced having an ultrasound scan of the joints, none of the patients in the low-adhering group had been exposed to this test (Quote 40).
Quote 36: Who cares if I have rheumatoid arthritis? Everyone has joint pains and this what people generally think. [69, retired, Punjabi speaking, Asian patient]
Quote 37: I still believe that this disease is not holding the same awareness as the heart diseases … so people don’t take arthritis seriously … err the medication is not taken seriously. [37, legal secretary, English speaking, Asian patient]
Quote 38: I didn’t know that this disease can come and go like this. If I had known I would not reduce my medications. [33, self-employed, English speaking, Asian patient]
Quote 39: No I wasn’t aware of this my doctor didn’t tell me [referring to disease activity measure – disease activity score]. So this works like a blood pressure when it is high you know it’s serious? [41, off work due to RA, Punjabi speaking, Asian patient]
Quote 40: No I didn’t ever have anything like this. [referring to ultrasound scan of joints] [37, legal secretary, English speaking, Asian patient]
Patients’ suggestions about strategies to optimize adherence to DMARDs
Themes that acted as drivers for high adherence to DMARDs (such as the quality and quantity of information provided) were suggested to low-adhering patients as potential ways of improving their adherence to DMARDs. All low-adhering patients (ten patients) agreed on the potential benefits of the drivers that were suggested by high-adhering patients. When patients with low adherence were asked about the types of visualization tool they felt would best improve adherence, they said they would prefer to see real-time ultrasound images rather than static images of joints that were not their own. However, some patients (three patients) indicated that pictorial representations would be better included in leaflet form. Seven low-adhering patients believed that the visualization of swelling in joints would enhance patients’ understanding of the nature and severity of the disease and the need to take medicines in the long term (Quotes 41 and 42). All ten patients further added that showing them the results of other disease parameters such as a measure of inflammatory makers in the blood or composite disease activity scores would also encourage them to take their DMARDs as prescribed (Quote 43). All ten patients highlighted that good communication with health professionals, health professional support, and better explanation of the risks of RA to their health would all promote better medication adherence (Quotes 44–46). Three patients felt that the level of engagement with disease information was an individual choice (Quote 47).
Quote 41: I think the scan would change your attitude to how you think about medicines …. [44, Microbiologist, English speaking, Asian patient]
Quote 42: You see I need something to validate to show me that I have a condition serious as this (rheumatoid arthritis). I think a scan can do this …. [37, legal secretary, English speaking, Asian patient]
Quote 43: My friend has a sugar monitoring machine he knows what a good and high level is. So if you told patients about disease activity levels it would encourage knowing how the medicines are working. [69, retired, English speaking, White patient]
Quote 44: Knowing how this disease will affect us in the future needs to be explained … so the seriousness of the disease does need to be told …. [56, off work due to RA, Punjabi speaking, Asian patient]
Quote 45: You see the disease isn’t viewed seriously, so if the risks aren’t explained then people will not take the medication seriously. [63, retired, Punjabi speaking, Asian patient]
Quote 46: Knowing the team is there to support you … the journey is shared and if the patients are made to feel like this then it’s easier, you know. [69, retired, English speaking, White patient]
Quote 47: Hmm I am not sure on what would help …. I think it doesn’t matter what you use to explain the disease; it’s all up to the individual, isn’t it? I mean if I want to know more then I will, but it’s all on how I want to take this …. [63, retired, English speaking, White patient]
Discussion
This study has highlighted the role of symptom experience, illness perceptions, the perceived benefits and risks of DMARDs, and the quality and quantity of information about RA and DMARDs in determining adherence to DMARDs. The findings provide an insight into some of the drivers and barriers for RA patients’ behavior toward their medication. Decisions not to take DMARDs were driven by the perception that RA was a nonserious, short-term condition, having insufficient information regarding the disease and the importance of regular DMARD therapy, and lack of discussion around disease parameters (eg, blood-based inflammatory marker results and disease activity scores). The high-adhering patients based their decision to take DMARDs on the perception that RA was a serious and long-term disease and felt that they had received sufficient information regarding the disease and disease activity parameters.
In line with other studies, the findings in our study showed the extent to which patient beliefs influenced treatment adherence – this has been widely reported in other chronic conditions, including asthma, cardiac disease, renal failure, cancer, and human immunodeficiency virus.Citation14,Citation15,Citation26 The NCF and SRM work suggests that a patient’s adherence decisions are a result of the balance between their perceived need for the medication (necessity) and their concerns regarding its use. We were able to explore how patients with RA balanced these to make decisions about DMARDs. Patients in our study who adhered well recognized the necessity of DMARD therapy, but some low-adhering South Asian patients clearly had doubts about their personal need for treatment. Studies on DMARD adherence, as well as studies on other conditions have also shown similar importance of medication beliefs.Citation27–Citation29 In our study, nonadherence in RA, therefore, was affected by individuals’ views about perceived illness.
Due to symptoms being episodic, the low-adhering patients tended to view their RA as being short term and nonserious. This was particularly evident in the South Asian patients. Similarly, a study conducted in India also found that South Asian patients did not regard RA as a serious condition and had negative beliefs about RA treatments.Citation30 Similar concepts have been reported among South Asian patients with other chronic conditions.Citation31–Citation34 In our study, South Asian patients with RA suggested that awareness of RA within their community and of the medication used for its management had an influence on their adherence to DMARDs. Lack of knowledge of RA and delays in initiating treatment have been reported in our previous work.Citation35,Citation36 Furthermore, a study conducted in IndiaCitation30 reported that South Asian patients with RA were more familiar with traditional remedies than Western medicines, and were found to be using these remedies alongside Western medicines. Similarly, our study has also found that some patients viewed traditional remedies favorably and felt that these could help to improve their RA symptoms.
Our study has identified potentially modifiable patient beliefs. Clinicians need to address patients’ perceptions of medication need and concerns early in the treatment course. The key messages from our data were that the need for treatment and decisions to continue taking DMARDs were reinforced by receiving adequate information and exposure to visual representations of the disease process, particularly images of their own joints obtained by ultrasound or plain radiography. Evidence regarding improving patients’ experiences or understanding of the disease by ultrasound scanning is not well documented in RA.Citation37 To date, one pilot study of 18 patients with RA has suggested that using ultrasound to illustrate the processes operating in their joints can reduce patients’ concerns about treatment.Citation37 Furthermore, the study showed that using ultrasound scans as an educational tool helped to increase beliefs about the necessity of treatment. However, with its small sample size and short follow-up, the study was not designed to measure the effect of this intervention on medication adherence levels. Larger studies are required to investigate the role of ultrasound scanning in improving medication adherence in RA. The findings of our study suggested that apart from visualization of joints, the ability to view graphical plots of clinical parameters such as the disease activity score and levels of inflammatory markers may be helpful in improving patients’ understanding of the need for long-term therapy.
The utility of pictorial/visualization tools to engage patients in understanding their disease and its treatment and in reducing anxiety has been reported in other conditions. For example, in relation to ovarian cancer, it has been shown that the use of ultrasound scanning of the ovaries reduced patients’ anxiety and improved their confidence and well-being.Citation38 Furthermore, the use of a moving three-dimensional heart in the context of explanation of future risks of heart disease had more impact on patients than did text-based information alone.Citation39,Citation40 The authors noted that the three-dimensional images of the heart increase patients’ common sense understanding of heart disease risk, causal beliefs, and control beliefs. Moreover, patients made more behavioral lifestyle changes, such as eating a healthy diet and taking up physical exercise, in response to such images.Citation17 In a separate studyCitation40 that demonstrated change in behavior, the authors reported that an intervention, whose development was informed by components of the CSM, enhanced patients’ understanding of heart disease risk and had a motivational effect on patient engagement. Building similar interventions in rheumatology might benefit patients from ethnic backgrounds such as those of South Asian origin who may need to be educated more about the differences between “curing” and “treating” RA with medicines and may also be of particular value in improving overall clinical outcomes in all patients.
This study had a number of limitations. Firstly, patients’ views about other medicines that they were taking were not explored. Data regarding patients’ views about medications such as antihypertensives might have provided insights regarding their relative views about different classes of drugs used to treat different conditions. The data from this study suggested that patients with RA expressed different views about conventional and biological DMARDs based on their experiences of the relative efficacy of these classes of medications. These views might have an effect on adherence; however, this aspect was not fully explored. The views of patients who refused to take part could have been different to those presented in this study. Despite these limitations, the strength of this study was that it captured views about medication adherence from adherent and nonadherent patients.
Conclusion
This study provides a deeper understanding of adherence to DMARDs in patients with RA. Improving adherence is likely to be facilitated by incorporating visual representations of the disease process, open discussion of disease parameters, and better explanations of the consequences of poorly controlled RA into the consultation. A good relationship with health professionals may also promote patients’ adherence to DMARDs.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
We would like to thank Amandeep Johal for reading and verifying the non-English transcripts. This study was funded by the National Institute for Health Research grant number (RGKP15291).
Disclosure
The authors report no conflicts of interest in this work.
References
- EmeryPEvidence supporting the benefit of early intervention in rheumatoid arthritisJ Rheumatol Suppl20022923812435162
- National Audit Office ReportServices for people with rheumatoid arthritis Available from: http://www.nao.org.uk/publications/0809/rheumatoid_arthritis.aspxAccessed April 7, 2015
- KitasGDGabrielSECardiovascular disease in rheumatoid arthritis: state of the art and future perspectivesAnn Rheum Dis201170181421109513
- YoungADixeyJKulinskayaEWhich patients stop working because of rheumatoid arthritis? Results of five years’ follow up in 732 patients from the Early RA Study (ERAS)Ann Rheum Dis200261433534011874837
- SymmonsDPPriorPScottDLBrownRHawkinsCFFactors influencing mortality in rheumatoid arthritisJ Chronic Dis19863921371453944225
- PasmaAVan’t SpijkerAHazesJMBusschbachJLuimeJFactors associated with adherence to pharmaceutical treatment for rheumatoid arthritis patients: a systematic reviewSemin Arthritis Rheum2013431182823352247
- World Health OrganizationAdherence to Long-Term Therapies-Evidence for ActionGenevaWorld Health Organization2003
- OsterbergLBlaschkeTAdherence to medicationN Engl J Med2005353448749716079372
- MartinLRWilliamsSLHaskardKBThe challenges of patient adherenceTher Clin Risk Manag20051318919918360559
- van den BemtBJZwikkerHEvan den EndeCHMedication adherence in patients with rheumatoid arthritis: a critical appraisal of the existing literatureExpert Rev Clin Immunol20128433735122607180
- NeameRHammondABeliefs about medications: a questionnaire survey of people with rheumatoid arthritisRheumatology (Oxford)200544676276715741193
- GoodacreLJGoodacreJAFactors influencing the beliefs of patients with rheumatoid arthritis regarding disease-modifying medicationRheumatology (Oxford)200443558358614970399
- HorneRPatients’ beliefs about treatment: the hidden determinant of treatment outcome?J Psychosom Res199947649149510661596
- HorneRWeinmanJSelf regulation and self management in asthma: exploring the role of illness perceptions and treatment beliefs in explaining non-adherence to preventor medicationPsychol Health2002171732
- HorneRWeinmanJPatients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illnessJ Psychosom Res199947655556710661603
- CliffordSBarberNHorneRUnderstanding different beliefs held by adherers, unintentional nonadherers, and intentional nonadherers: application of the Necessity-Concerns FrameworkJ Psychosom Res2008641414618157998
- LeventhalHNerenzDRSteeleDJIllness representations and coping with health threatsTaylorSESingerJEHandbook of Psychology and HealthHillsdale, NJErlbaum1984454219252
- KumarKGordonCBarryRShawKHorneRRazaK‘It’s like taking poison to kill poison but I have to get better’: a qualitative study of beliefs about medicines in rheumatoid arthritis and systemic lupus erythema-tosus patients of South Asian originLupus201120883784421511761
- KumarKGordonCToescuVBeliefs about medicines in patients with RA and SLE: a comparison between patients of South Asian and White British originRheumatology200847569069718375972
- CooperVGellaitryGHankinsMFisherMHorneRThe influence of symptom experiences and attributions on adherence to highly active anti-retroviral therapy (HAART): a six-month prospective, follow-up studyAIDS Care200921452052819401867
- KumarKRazaKNightingalePA mixed methods protocol to investigate medication adherence in patients with rheumatoid arthritis of White British and South Asian originBMJ Open2013316
- ArnettFCEdworthySMBlochDAThe American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritisArthritis Rheum19883133153243358796
- GreenhalghTTaylorRPapers that go beyond numbers (qualitative research)BMJ199731571107407439314762
- Dixon-WoodsMAgarwalSJonesDYoungBSuttonASynthesising qualitative and quantitative evidence: a review of possible methodsJ Health Serv Res Policy2005101455315667704
- Hewitt-TaylorJUse of constant comparative analysis in qualitative researchNurs Stand20011542394212212430
- HorneRCooperVGellaitryGDateHLFisherMPatients’ perceptions of highly active antiretroviral therapy in relation to treatment uptake and adherence: the utility of the necessity-concerns frameworkJ Acquir Immune Defic Syndr200745333434117514019
- de ThurahANorgaardMHarderIStengaard-PedersenKCompliance with methotrexate treatment in patients with rheumatoid arthritis: influence of patients’ beliefs about the medicine. A prospective cohort studyRheumatol Int201030111441144819823840
- TreharneGJLyonsACKitasGDMedication adherence in rheumatoid arthritis: effects of psychosocial factorsPsychol Health Med200492337349
- HorneRChapmanSCParhamRFreemantleNForbesACooperVUnderstanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the necessity-concerns frameworkPLoS One2013812e8063324312488
- ChitnisNMethaPNSamantRBhojaniKSJoshiVRLag time between disease onset and first visit to a tertiary rheumatology centre by patients with rheumatoid arthritisINJR20138161164
- LawtonJAhmadNPeelEHallowellNContextualising accounts of illness: notions of responsibility and blame in white and South Asian respondents’ accounts of diabetes causationSociol Health Illn200729689190617986021
- LawtonJParryOPeelEDouglasMDiabetes service provision: a qualitative study of newly diagnosed type 2 diabetes patients’ experiences and viewsDiabet Med20052291246125116108856
- LawtonJAhmadNHannaLDouglasMHallowellN‘I can’t do any serious exercise’: barriers to physical activity amongst people of Pakistani and Indian origin with type 2 diabetesHealth Educ Res2006211435415955792
- KishoreJAhmadIKaurRPK MBeliefs and perceptions about cancers among patients attending radiotherapy OPD in Delhi, IndiaAsian Pac J Cancer Prev20089115515818439096
- KumarKDaleyECarruthersDMDelay in presentation to primary care physicians is the main reason why patients with rheumatoid arthritis are seen late by rheumatologistsRheumatology (Oxford)20074691438144017578850
- KumarKDaleyEKhattakFBuckleyCDRazaKThe influence of ethnicity on the extent of, and reasons underlying, delay in general practitioner consultation in patients with RARheumatology (Oxford)20104951005101220189950
- El MiedanyEl GaafaryMPalmerDAssessment of the utility of visual feedback in the treatment of early rheumatoid arthritis patients: a pilot studyRheumatol Int201232103061306821909946
- TadmorOPZlotogorskiZGalron-DuniecMThe effect of feedback on anxiety levels during ultrasound scanning for ovarian cancerUltrasound Obstet Gynecol1995621351398535917
- ShahabLHallSMarteauTShowing smokers with vascular disease images of their arteries to motivate cessation: a pilot studyBr J Health Psychol200712227528317456286
- BovetPPerretFCornuzJQuilindoJPaccaudFImproved smoking cessation in smokers given ultrasound photographs of their own atherosclerotic plaquesPrev Med200234221522011817917
