Abstract
Research on healthcare shows that the relationship between empathy and burnout is complex. The aim of this systematic review and meta-analysis is to clarify the link between different empathic components and burnout components in healthcare professionals. A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidance. The search strategy was applied in PubMed, PsycINFO, CINAHL, Scopus, and Medline, from January 1990 to January 2021. Population included nurses and doctors. Key inclusion criteria were articles addressing the relationship between different components of empathy and professional performance and wellbeing or burn out, or studies using burnout and empathy measures with validity support from commonly accepted sources of evidence. Risk of bias was assessed using the Mixed Methods Appraisal Tool. From 1159 references identified, 22 studies were included in the systematic review, and 5 studies in the meta-analysis. Empathic Concern was significantly correlated with Depersonalization and Personal Accomplishment. Moreover, the links between Perspective Taking, Depersonalization and Personal Accomplishment were statistically significant. In conclusion, exploring and understanding the complex links between empathy and burnout could help healthcare professionals as well as institutions to reduce the risk of suffering burnout.
Introduction
Over the past few decades, advances in the behavioral sciences have generated numerous theories of empathy that attempt to explain a variety of different interconnected processes. However, despite the increasing knowledge developed in the last years, there is some controversy regarding the role of empathy in healthcare professionals’ wellbeing, especially in burnout. In an attempt to unravel the reasons for these inconsistent results, here we analyse whether the components of empathy are differently related to each of the components of burnout in healthcare professionals (physicians and nurses) through a systematic review of the literature and a meta-analysis of the available data.
What is (and What is Not) Empathy?
Empathy is a complex and multifaceted concept that has been described in the literature in many different ways.Citation1 The diversity in conceptual and operational definitions, and the unrestrained use of the term “empathy”, make the scientific advancement in the field a challenge. In an extensive review of the concept, Cuff et alCitation2 identified a total of 43 different definitions of the term empathy. For that reason, some researchers consider that empathy is an elusive term that describes a variety of distinct psychological phenomena.Citation3 Whereas some authors try to establish order by proposing a uniform definition to operationalise the construct,Citation2 other scholars have proposed that the word empathy should be replaced for the specific skills, traits, capacities, attitudes, responses, and behaviors that are represented in various definitions and measuring instruments.Citation4,Citation5 Hall and Schwartz (2019) performed a quantitative review and conceptual analysis of empathy definitions through 489 studies published between 2001 and 2017. Considering the wide diversity of definitions, as well as inconsistencies between conceptual terms and measurements employed, they concluded that it is important to sidestep the term empathy in favor of lower-level terms that specifically describe what is being measured in each study. Unfortunately, the number of competing conceptualizations in the literature makes it difficult to determine which process or mental state the term empathy refers to in any study or theoretical debate.Citation3
The difficulties linked to the definition of empathy are also transferred to its measurement. Among the instruments developed to assess empathy, the Interpersonal Reactivity IndexCitation6 is undoubtedly one of the most used. According to Davis,Citation6 empathy may be understood to have four main components. Perspective-taking is the tendency to adopt others’ point of view or knowing another person’s internal states from a cognitive viewpoint, that is, knowing that the other is suffering. Empathic concern is related to abilities to experience feelings of warmth, compassion, and concern for other people, assessing the other-oriented approach of empathy with a positive emotional response to the suffering. Personal Distress component refers to a self-oriented approach to empathy, a negative emotion resonance towards suffering, including feelings of distress and unease when observing others’ suffering. A fourth component, called Fantasy, is included in IRI, and refers to the individual’s tendency to get involved with fictional characters and situations in books, movies, and play. Complementary, the Jefferson Scale of EmpathyCitation7 has been broadly used for measuring empathy in the context of patient care. This scale has been translated into 47 languages and used in more than 70 countries. It contains three components of empathy: Perspective Taking, Compassionate Care, and Walking in Patient’s Shoes. Both instruments highlight the multifaceted conceptualization of empathy, and for that reason they offer the opportunity to explore the specific role of each of the components of empathy in burnout.
Supporting evidence for the complexity of empathy comes from social neuroscience research. Functional MRI (fMRI) studies have shown that empathic concern is associated with neural response in areas involved in social cognition and decision-making such as the striatum and ventromedial prefrontal cortex. On the other hand, the empathic component of personal distress is associated with activity in the insula, amygdala and the somatosensory cortex, that is, circuits involved in saliency, emotional resonance, and affect processing.Citation3 These differences are in line with research on perspective taking showing that the same brain areas involved in the affective and motivational processing of the direct (own) perception of pain are involved in the perception of the pain of others. Specifically, the fact that the observation of pain in others activates the brain structures involved in negative emotional experiences has important consequences regarding whether that observation will lead to empathic concern or personal discomfort. Despite the same neural circuits are activated when people adopt the self-perspective and the perspective of others, the frontal lobes may facilitate the distinction of perspectives, assisting one to keep from intrusions from one’s own perspective when adopting other’s perspective.Citation33,Citation34 This is especially relevant when observing other’s suffering and could explain the differences between self-other awareness linked with personal distress and empathic concern.
The Role of Empathy in Burnout
Research has shown that clinician’s empathy is a central element in healthcare context,Citation8 with a strong impact in patient’s satisfaction and adherence to treatments.Citation9 Whereas clinician’s empathy positively affects the patients’ overall wellbeing and contributes to their healing, it is less clear what is the effect of empathy in healthcare professionals’ wellbeing. There is a wide variety of ways in which empathy seems to add value to medical practice. Unfortunately, very few components in formal medical and nursing training focus on how to manage emotions.Citation3 Undoubtedly, empathy is an extremely difficult phenomenon for doctors and nurses, who day after day must cope with intense suffering from patients. Healthcare professionals face the challenge of devoting the right balance of cognitive and emotional resources to their patients’ pain experience, for their own wellbeing as well as for their patients’ wellbeing. Healthcare professionals must deal with their emotional reactions to stress and others’ suffering, and they are witnesses to highly demanding clinical situations day after day.
From a theoretical approach, one of the assumptions about empathy in healthcare is that there are emotional costs for displaying an empathic approach day after day towards patients and their families.Citation10,Citation11 Specifically, one of these personal costs linked to empathy has been the burnout syndrome.Citation12,Citation13
The burnout syndrome can be defined as a prolonged response to chronic stressors at work that includes physical depletion, feelings of helplessness, negative attitudes towards work, life, the self, and others.Citation14,Citation15 There is a strong scientific consensus on the multidimensionality of burnout.Citation16 A central component of burnout is emotional exhaustion, a felt depletion of emotional energy and resources.Citation17,Citation18 The second component of burnout is the development of depersonalization, which could lead to the view that patients deserve what they suffer. Finally, the lack of personal accomplishment is conceived as the tendency to evaluate oneself negatively, with feelings of unhappiness at work.Citation19
Burnout is considered one of the main problems for quality of life in healthcare professionals.Citation20 The high levels of burnout in physicians and nursesCitation21,Citation22 are considered a threat to the professionals themselves, but also to their patients and the organizations where they work.Citation23 This syndrome involves severe health problems, such as anxiety, depression, irritability, changes in mood, insomnia, and drug use,Citation24 as well as reduced productivity, increased turnover, and increased costs to the healthcare system.Citation21,Citation25
Notwithstanding its interest for both healthcare professionals and patients, findings of the specific role of empathy and related processes in burnout are inconsistent.Citation26 To explain the relationship between burnout and empathy, Zenasni et alCitation27 proposed three theoretical hypotheses: (1) burnout reduces the ability of clinicians to respond empathically; (2) being empathic draws significantly on personal resources and thus causes burnout; and (3) being empathic protects clinicians from burnout. However, empirical evidence about the impact of empathy in burnout is inconclusive.Citation10,Citation28,Citation29 Whereas several studies have reported a positive relationship between empathic concern and burnout,Citation30 other studies found a negative relationship between burnout and empathy among primary care physicians and nurses.Citation28,Citation31 In the same vein, a systematic review of 10 studies correlating empathy and burnout in healthcare professionals concluded that most of the studies provided empirical support for a negative relationship between empathy and burnout; one study showed a positive relationship between burnout and empathy, and one study reported contradictory evidence with positive and negative correlations between different subscales of the empathy and burnout measures.Citation26 Likewise, Williams et alCitation32 found similar conclusions in a scoping review.
In their research, Wilkinson et alCitation26 considered that the original three hypotheses from Zenasni et alCitation27 could be reduced to 1) there is a negative association between burnout and empathy (as one construct increases the other decreases), and 2) there is a positive association between burnout and empathy (high burnout is associated with high empathy). However, there are a large number of possibilities that are not being considered, such as that each component of empathy could play a particular role in each component of burnout. The importance of analyzing the relationships between each component of burnout and each component of empathy lies in increasing the possibilities to reduce the risk of suffering burnout and promoting empathic skills that mitigate the effect of exposure to constant suffering.
The Present Research
The COVID-19 pandemic has brought an extremely pressure on hospitals, with specialists seriously affected for the terribly hard conditions to work that they suffered. Undoubtedly, the pandemic has accentuated the need to deal with the emotional wellbeing and stress-related problems of healthcare professionals. But even before this critical period, health problems among healthcare professionals resulting in compassion fatigue, burnout, and professional distress were unacceptably common. The need to cope with emotionally distressing situations day after day could be part of the problem.Citation3 In this line, the purpose of this study is to analyze the link between empathy and burnout by considering their specific components instead of the general measure of each of the concepts.
Most studies that explore the relationship between empathy and burnout have important limitations. In healthcare contexts, limitations of correlational studies, characteristics of the samples, potential biases, and type of measurement instruments used to explore empathy make it difficult to get determine the role of empathy in burnout. As Clark et alCitation35 pointed out, most of studies do not reflect the multidimensionality of empathy, which has undermined the advancement in the study of differential effects of each of the empathic components on other relevant phenomena. For those reasons, a systematic review and meta-analysis could be especially useful in obtaining consistent conclusions regarding the links between empathy and burnout in healthcare.
Specifically, this research aims at identifying whether the components of empathy are differently related to each of the components of burnout in both physicians and nurses. More precisely, the research question was formulated as follows: In healthcare professionals (doctors and nurses), are the components of empathy (eg, perspective-taking, empathic concern, and personal distress) differently related to each of the components of burnout (emotional exhaustion, depersonalization, and lack of accomplishment)?
Materials and Methods
This research was developed following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses http://www.prisma-statement.org/) guidelines, and PRISMA Checklist is available. Data were analyzed using R, version 4.0.0Citation36 and the package meta,Citation37 package metacorCitation38 and package metaphor.Citation39 The protocol for this systematic review and meta-analysis on the link between different components of empathy and burnout was registered with the online database PROSPERO (CRD42021235359).
Search Strategy
We sought both quantitative and qualitative empirical studies. Full details of the Search Strategy are accessible. The search was focused on publications from January 1990 to October 2022, and it was carried out between October 29, 2020 and October 1, 2022. The databases consulted with language restrictions to English or Spanish (when possible) were PubMed, PsycINFO, CINAHL, Scopus, and Medline. Four authors participated independently in the relevance assessment of retrieved articles, first by title and abstract, and then by full text.
The primary outcome was to clarify the relationship between different components of empathy and consequences in both performance and professional wellbeing with a special focus on burnout, in healthcare professionals (doctors and nurses). Additional outcomes were a) to identify the role of different components of empathy in healthcare providers’ experiences of burnout, and b) to identify interventions related to empathy in healthcare providers, the evidence for these, and their outcomes. Full details of the inclusion and exclusion criteria are described in Search Strategy. In brief, key inclusion criteria were articles addressing the relationship between different components of empathy and professional performance and wellbeing, burnout or moral distress, or studies to provide specific data about the relationship between burnout and empathy using burnout and empathy measures with validity support from commonly accepted sources of evidence. Population included nurses and doctors, including residents. Studies conducted with healthcare professionals different from doctors and nurses, such as nurse assistants, paramedics, pharmaceutics, clinical psychologists, physiotherapists, ambulance technicians, were excluded. Students also were excluded since the research focuses in professional contexts. Studies estimating rates of burnout in general or studies considering just empathy without differentiation of empathic components were excluded. The articles were screened by two authors independently and in duplicate, following the inclusion and exclusion criteria. Articles were first screened by title and abstract, and secondly by full-text reading. Disagreements were discussed by the four authors, and an agreement reached.
Data Extraction
Data extraction and quality assessment were undertaken by two authors independently and in duplicate using a table developed by the authors ad hoc to facilitate the data extraction and to gather relevant information. The two reviewers independently and in duplicate collected data from reports, the results were compared, and a synthesis was done. The Quality Assessment of the selected studies was performed with the Mixed Methods Appraisal Tool (MMAT).Citation40
Results
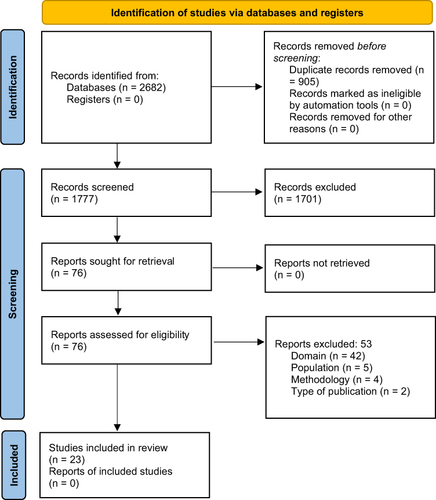
A total of 1982 references were identified. After checking for duplicated articles and executing an initial review for four reviewers by title and abstract, 76 articles were selected to screen by full text. Finally, 23 articles met the criteria for inclusion (see ).
Figure 1 Systematic review flow diagram adopted in this study based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA).
Study Characteristics
The characteristics of the selected studies are shown in . Most of the papers (12) were from Europe or the UK, whilst 7 were from the USA, 3 papers were from Asian countries, and one paper was from Israel. Of the 23 included papers, 6 were performed in both nurses and physicians, while only 4 were performed exclusively in nurses, 13 studies were conducted only in doctors. Of those, the majority (9) was performed with residents, and the remaining 4 with specialists in different fields.
Table 1 Characteristics of Included Studies
The 23 reviewed articles differed in terms of research design. Fifteen of them described cross-sectional studies: 13 studies were correlational designs,Citation8,Citation23,Citation41–51 one was a cohort study,Citation52 and one was an observational study.Citation53 Four studies included an interventional design, using one of them a randomized experiment with a control group,Citation54 whereas the other three were quasi-experimental studies.Citation55–57 Four articles described a longitudinal cohort design.Citation58–61
The Maslach Burnout Inventory (MBI) was the most common instrument used to measure burnout levels in healthcare professionals, although six studies utilized a version of the original scale, such as MBI-General Service,Citation8 MBI-Human Service Survey,Citation51,Citation52,Citation54 an abbreviated version of MBICitation47 and a Danish adaptation composed of 20 items.Citation54 As Personal Accomplishment can be expressed as a positive achievement (e.g.Citation44,Citation50) or as a reduced self-development (e.g.Citation45,Citation48), for clarity of findings, it is reported through the results section as a reduced Personal Accomplishment. The Oldenburg Burnout Inventory (OLBI)Citation66 was utilized by one study.Citation23 This instrument comprises two components of burnout: exhaustion and disengagement. All articles break their findings down into components of burnout, except for one that calculated it as a global variable.Citation47 Moreover, one studyCitation61 used the Copenhagen Burnout Inventory (CBICitation62), which is composed by three subscales: Personal burnout (general state of prolonged physical and psychological exhaustion), Work-related burnout, and Patient-related burnout.
In contrast, a variety of instruments were used to assess empathy. Interpersonal Reactivity Index (IRI)Citation6 was utilized by 12 studiesCitation8,Citation41,Citation43–48,Citation50,Citation58–60 although some of them only evaluated some of the components of the scale. For example, Omdahl and O’DonnellCitation48 and Kelly-Hedrick et alCitation46 measured Empathic Concern, while Winkel et alCitation57 assessed Empathic Concern and Perspective Taking, and Reed et alCitation59 included both Empathic Concern and Personal Distress. Likewise, the component of Fantasy is frequently excluded from the assessment, but it has been evaluated in some studies (egCitation50). Moreover, one article reports the results of empathy as a single global score, although all their components, except Empathic Concern, were evaluated.Citation8 Nine studiesCitation42,Citation49,Citation51–56,Citation58 used the Jefferson Scale of Physician Empathy (JSPE).Citation7 Although this measure consists of three components, it is frequently analyzed as a single variable (e.g.Citation42,Citation52,Citation53). The Basic Empathy Scale short version (BES-A),Citation67 which comprises two components (affective and cognitive empathy) was used by one study.Citation23 Altmann and RothCitation61 assessed empathy through three instruments: The Toronto Empathy Questionnaire (TEQCitation63), as a measure of affective empathy, the Geneva Emotion Recognition Test (GERTCitation64) that is a computer-based test to examine the ability to correctly detect emotions in other people, and the Social Mindfulness Paradigm (SOMICitation65), which is another computer-based procedure to measure prosocial behavior as recognizing the needs and wishes of others.
Links Between Burnout and IRI Empathy Components
Five studies of those that used the IRI reported correlations between components of empathy and burnoutCitation44,Citation45,Citation50,Citation59,Citation60 with consistent results. All of them found that Depersonalization was negatively correlated to Perspective Taking. In addition, four studiesCitation44,Citation45,Citation50,Citation60 showed that Depersonalization was also negatively associated with Empathic Concern, and a reduced Personal Accomplishment was negatively correlated with Perspective Taking. Three studiesCitation44,Citation45,Citation50 found that Emotional Exhaustion was positively linked to Personal Distress. Moreover, two studies showed a significant and positive correlation between Personal Distress and reduced Personal Accomplishment.Citation44,Citation45 Likewise, two papers noted that Empathic Concern was negatively related to reduced Personal Accomplishment.Citation44,Citation60 Although Ren et alCitation8 also indicated correlations between burnout and empathy, findings were reported through IRI total score.
Regarding regressions, five studies reported these analyses,Citation8,Citation44,Citation47,Citation48,Citation50 but results were inconsistent. While a study found that Empathic Concern predicted high levels of Emotional Exhaustion,Citation50 this link was statistically non-significant in two other papers.Citation44,Citation48 Omdahl and O’DonnellCitation48 only measured Empathic Concern as a component of empathy and is the only one that has shown Empathic Concern also predicted low levels of reduced Personal Accomplishment and Depersonalization. Perspective Taking predicted low levels of Depersonalization,Citation44,Citation50 Emotional Exhaustion,Citation50 and reduced Personal Accomplishment.Citation44 Likewise, only the study of Delgado et alCitation44 indicated that Personal Distress predicted high levels of Emotional Exhaustion, and a low reduced Personal Accomplishment. McManus et alCitation47 examined the MBI as a single dimension without finding significant links between it and empathy components, while Ren et alCitation8 also reported regressions through IRI total score.
Four studies measured both burnout and empathy through their componentsCitation41,Citation43,Citation46,Citation57; however, they were not focused on exploring the association between these variables. Therefore, these findings were not reported.
Links Between Burnout and JSPE Empathy Components
Although the JSPE is a common instrument to assess empathy in healthcare professionals, the literature tends to describe their findings joining the components as a single score. This is the case of three of the reviewed studies.Citation42,Citation52,Citation53
Only three studies exposed their results by components of empathy and burnout.Citation49,Citation51,Citation58 All of them reported that Perspective Taking was negatively linked to reduced Personal Accomplishment, also finding this correlation in transversal and longitudinal analyses.Citation58 In addition, Sturzu et alCitation51 indicated that Compassionate Care and Standing in the Patient’s Shoes components were negatively related to Depersonalization, and Standing in the Patient’s Shoes was also negatively associated with low levels of Personal Accomplishment.
As happened with studies that used IRI, three articles aimed to examine the effect of an intervention in several variables, such as burnout and empathy, but their results do not inform of links between components of both scales.Citation54–56
Links Between Burnout and Other Empathy Components
Only one study examined empathy components with the BES-A instrument, separately analyzing nurses and doctors.Citation23 Its findings showed that Cognitive Empathy was negatively correlated to Disengagement in doctors, while Affective Empathy was positively linked to Emotional Exhaustion in nurses. Results of regression analyses indicated that Affective Empathy predicted high levels of Emotional Exhaustion, whereas Cognitive Empathy was unrelated to components of burnout both in nurses and doctors.
Altmann and RothCitation61 analyzed the link between empathy and burnout was analyzed in a nursing sample. Cross-sectional correlations indicated that Affective Empathy was positively related to Personal Burnout but negatively associated with Patient-related Burnout. Longitudinal findings showed that Work-related Burnout predicted Emotion Recognition, while Patient-related and Personal Burnout predicted Prosocial Behavior related to affection identification of others. By contrast, there were no significant cross-lagged relation between Affective Empathy and Burnout dimensions.
Meta-Analysis with Correlations
A separate meta-analysis was performed for each Empathy-Burnout subscales correlation using the metaphor package in R.Citation39 This meta-analysis meets all the criteria Cochrane Consumers and Communication Group reviews for meta-analysis.Citation67 Only 5 studiesCitation44,Citation45,Citation51,Citation59,Citation60 reported enough data about subscales to be included in the meta-analysis. For each pair of correlations, a random-effects model using the unweighted mean r, which is based on ks (the total number of studies), was applied because it indicates whether the variance in effect sizes is no greater than what would be expected by sampling error and, therefore, it allows the generalization of the findings. Effect sizes were estimated applying an algorithm of maximum likelihood (ML). The effect size r is used here because it represents both the strength and direction of the associations. All calculations involving r were performed by first transforming r to the Fisher’s z transformation of r, and then returning results to the r metric. Measures for estimating the amount of heterogeneity were computed.Citation68
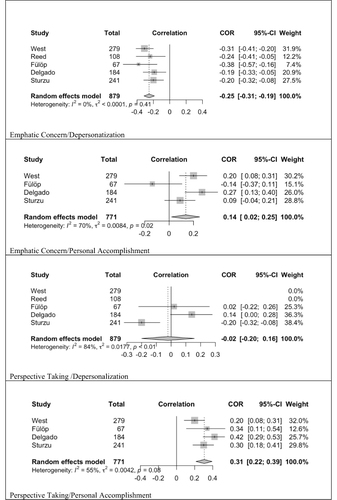
Results revealed that Empathic Concern was significantly and negatively correlated with Depersonalization, and positively correlated with Personal Accomplishment. Moreover, the links between Perspective Taking and Depersonalization and Personal Accomplishment were statistically significant (see ). Results revealed that effect size for the relationship between Empathic Concern with Depersonalization was significant [−0.252, p< 0.01]. The same significant effect size was found for Empathic Concern and Personal Accomplishment [0.13 p<0.01]. Moreover, the effect size links between Perspective Taking and Depersonalization [−0.27, p<0.01] and Personal Accomplishment [0.30 p<0.01] were significant. Confidence interval for tau heterogeneity index was included for different size effect tested (see ).
Table 2 Meta-Analysis Correlation Coefficient Estimates Between the Subscales for Empathy and Subscales for Burnout
shows the forest plot of correlations is statistically significant. Heterogeneity indexes were moderate–high, indicating variability across the studies. The highest levels of variability were due to the inclusion of Fülöp et al,Citation45 with prediction of a negative correlation between Empathic Concern and Personal Accomplishment, as well as Perspective Taking and Depersonalization, with a small sample size.
Discussion
This systematic review and meta-analysis explored the relationship between the different components of empathy and each of the different components of burnout in doctors and nurses. As expected, the findings were complex. Specifically, results indicated that healthcare professionals with high levels of Personal Accomplishment also show high levels of Perspective Taking, Empathic Concern and Standing in the Patient’s Shoes. On the other hand, results supported a negative association between Depersonalization and Perspective Taking, Empathic Concern, Compassionate Care, and Standing in the Patient’s Shoes. Together, these results highlight the importance of studying different components of empathy separately, since their impact on burnout components are different.
Among the three components of burnout, Emotional Exhaustion is the least related to empathy components; three studies reported a positive correlation between Personal Distress and Emotional Exhaustion. According to the job demands-resources model of burnout,Citation69 these results could suggest that exhaustion would be more linked with demands than with resources, and highlight the relevance to explore specific predictors of Emotional Exhaustion by differentiating it for the rest of components of burnout.
The pattern of results obtained with Personal Distress considerably differs from the rest of empathic components. This finding underlines the important differences across components that constitute empathy and invites to rethink whether all of them are actually part of what we call empathy. Besides, this result is in line with previous research showing that negative self-oriented emotions elicited by perceiving others’ suffering were associated with burnout and compassion fatigue.Citation12,Citation70 In this sense, there are two distinct ways in which people can take the perspective of others’ suffering. One form is thinking about how a suffering other feels or imagine-other perspective-taking (IOPT), and the other form is imagining oneself in the suffering other’s place or imagine-self perspective-taking (ISPT). A novel line of research suggests that empathy is less due to self–other merging (or a blurring in the distinction between the two), but rather that it is motivated by the recognition that the self is distinct from the other, and that one’s experience is distinct from the experience of others.Citation33,Citation71 Furthermore, social neuroscience research would help to increase the knowledge of the role of empathic components in burnout. More studies that clarify the role of the frontal lobes in avoiding intrusions from one’s own perspective when adopting other’s perspective could be essential to clarify differences between personal distress and the rest of components of empathy. Together, these promising lines of study could lead to a deeper understanding of the central role of the self-other merging versus distinctiveness perspective in empathy and their relationship with burnout.
As we have confirmed with this study, most research that explores empathy in the healthcare context does not differentiate what type of empathy is studied. This lack of specificity makes it difficult to understand and identify what is the role of empathic components in burnout. Importantly, results indicate that it is not necessary to reduce the empathic approach towards patients to decrease burnout. Instead of that, it is essential to identify which empathic component is unfolding for healthcare professionals and try to promote perspective taking and empathic concern. However, results indicate that personal distress should be minimised in healthcare contexts. In this line, working at identifying the different empathic approaches in healthcare is a key element to improve interventions aimed at supporting healthcare professionals’ wellbeing. Other ways to deal with the differential effect of the empathic components imply the improvement of specialized training and communication about the differences and specific effects of each of the empathic components.
We emphasize that only five studies (from a total of initial 1982 references) show the relationships between the components of IRI and Burnout, which was the main objective of this study. The absence of studies that show data on the relationship between empathy and burnout components might be a limitation among the published studies that have used these scales and have not given data on the correlation between them, or, as in most cases, these correlations were out of their scope. Hence, we claim that there is a need for research to show data on the correlation between the different dimensions of burnout and empathy using relevant instruments in the field.
From all the studies that we screened, none of them paid particular attention to the circumstances of the pandemic. What we have seen is that most of the studies carried out during the pandemic about burnout focused more on the relationship between burnout and working conditions under the pressure of the pandemic, and the relationship between burnout and some mindfulness practices, instead of the relationship with empathy in the circumstances of the pandemic. While these two areas are also interesting, those are out of our scope. It could be interesting to address how the relationship between the different dimensions of burnout and empathy are related under specific conditions such as the pandemic. However, the very difficult circumstances that the healthcare workers have experienced may have made it difficult to carry out some studies, so as not to overwhelm them with more questionnaires to fill out.
Our results constitute an advance in the knowledge of the links between empathy and burnout with relevant implications. From a theoretical approach, scholars usually link empathy to negative consequences for healthcare professionals (egCitation11,Citation13), while empirical work leads to more precise conclusions, revealing that the type of empathic component is crucial to determine potential personal costs when displaying empathy in healthcare contexts. In this way, and in line with recent recommendations (e.g.Citation35), the current study emphasizes the importance to continue in the advancement of the distinction between empathic components and other related concepts, such as compassionCitation72 and concern.Citation73 Therefore, future research should separately examine empathic and burnout components instead of considering them as a single factor. In addition, empirical research examining the components of empathy and potential associated emotional dysfunctions among healthcare professionals may be a key element to develop effective educational interventions for medical and nursing students.
Furthermore, this study has also a relevant practical impact. On the one hand, healthcare professionals need to handle the emotional costs of their work and the risk of suffering burnout. During the Covid-19 pandemic, healthcare professionals are facing important emotional demands, including grief from seeing so many patients die, fears of contracting the virus and infecting their family members, and anger over healthcare disparities and other systems’ failures.Citation74 These stressors have triggered or intensified burnout, depression, or anxiety, as well as the fear of suffering for displaying empathy, which also have negative consequences.Citation75 On the other hand, the study of the role of empathy in burnout could reformulate the way professionals think toward their own work. The culture of medicine in particular and healthcare in general reinforces the belief that physical and emotional exhaustion are part of the job.Citation74 Exploring and understanding the complex links between empathy and burnout could help healthcare professionals as well as institutions to reduce the risk of suffering burnout.
There are some limitations that should be considered when interpreting the conclusions. Recognizing the diversity of expressions that can be considered as components of empathy, it is possible that some terms have been left out of the search strategy. However, the authors tried to include all relevant terms. Furthermore, the current review only included studies in English and Spanish, which means that there may be other relevant studies that have been conducted and published in languages other than these. An important limitation of this review is also that many of the studies do not report correlations between components, which means a lack of reported data necessary to include the studies in the meta-analysis. We contacted the authors of the studies included in the SR to request the data, but we only obtained the data from one study.Citation60 Another limitation is that some of the studies included do not report the results separately for profession, and only in some of these studies it was possible to have the separate data after contacting the authors. Importantly, the studies included in this review have heterogeneous samples of both physicians and nurses, with different functions, responsibilities, and experience. Therefore, part of the difference in the results of review studies might be due to considering different groups of physicians and nurses equally and integrating their data.
Moreover, although the inclusion criteria contained papers that had qualitative or mixed methodology, in addition to quantitative one, the comparison of studies that utilized standardized psychometric assessments to measure the constructs was only possible and more reliable through quantitative designs. While qualitative studies can provide a richness of data that is lost in the numerical values assigned in standardized measures, in this review we found that no one of the qualitative studies potentially selected could be included because none of them reported results regarding the relationship between the different components of burnout and empathy. It should be noted that, while all the included studies have used MBI to measure burnout, the diversity of instruments to capture empathy have made this systematic review more difficult to carry out.
Finally, the use of self-reported measures of empathy in the studies leads to a series of limitations that should be considered. Recent research has shown that self-reports of empathy seem to be unrelated with empathic abilities.Citation76,Citation77 It is important to complement the use of self-reported measures of empathy with other measures, such as physiological or neurological measures, as well as measures provided by patients and colleagues.
Conclusion
Under the term empathy, a multitude of processes and different phenomena are collected. Therefore, it is expected that this set of differentiated processes will give rise to different effects on burnout, and more specifically, on each of its components. In recent years, numerous studies have identified the neurobiological mechanisms underlying the various elements grouped under the concept of empathy in the field of healthcare. More research will help to clarify the complex links between each of these elements and each of the burnout components, as well as the way they are influenced by the type of clinical task, service or unit where healthcare professionals are involved, and other mediated factors. The development of empirical knowledge about the role of empathy in burnout is relevant for multiple reasons. Undoubtedly, this systematic review led to the conclusion that more research is needed to disentangle the specific contribution of empathic components in burnout.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
This research was funded by the Office of Scientific and Technical Research (DGICYT), grant number PID2019-108800RA-I00.
References
- Batson. These things called empathy.pdf. In: Decety J, Ickes W, editors. The Social Neuroscience of Empathy. Massachussetts: MIT Press; 2009.
- Cuff BMP, Brown SJ, Taylor L, Howat DJ. Empathy: a review of the concept. Emot Rev. 2016;8(2):144–153. doi:10.1177/1754073914558466
- Decety J. Empathy in medicine: what it is, and how much we really need it. Am J Med. 2020;133(5):561–566. doi:10.1016/j.amjmed.2019.12.012
- Decety J, Cowell JM. The complex relation between morality and empathy. Trends Cogn Sci. 2014;18(7):337–339. doi:10.1016/j.tics.2014.04.008
- Hall JA, Schwartz R. Empathy present and future. J Soc Psychol. 2019;159(3):225–243. doi:10.1080/00224545.2018.1477442
- Davis MH. The effects of dispositional empathy on emotional reactions and helping: a multidimensional approach. J Pers. 1983;51(2):167–184. doi:10.1111/j.1467-6494.1983.tb00860.x
- Hojat M, Mangione S, Nasca TJ, et al. The Jefferson scale of physician empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61(2):349–365. doi:10.1177/00131640121971158
- Ren Y, Song H, Li S, Xiao F. Mediating effects of nursing organizational climate on the relationships between empathy and burnout among clinical nurses. J Adv Nurs. 2020;76(11):3048–3058. doi:10.1111/jan.14525
- Capozza D, Falvo R, Boin J, Colledani D. Dehumanization in medical contexts: an expanding research field. Test Psychom Methodol Appl Psychol. 2016;23(4):545–559.
- Decety J, Yang CY, Cheng Y. Physicians down-regulate their pain empathy response: an event-related brain potential study. Neuroimage. 2010;50(4):1676–1682. doi:10.1016/j.neuroimage.2010.01.025
- Haque OS, Waytz A. Dehumanization in medicine: causes, solutions, and functions. Perspect Psychol Sci. 2012;7(2):176–186. doi:10.1177/1745691611429706
- Gleichgerrcht E, Decety J. Empathy in clinical practice: how individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLoS One. 2013;8(4):1–12. doi:10.1371/journal.pone.0061526
- Gleichgerrcht E, Decety J. The relationship between different facets of empathy, pain perception and compassion fatigue among physicians. Front Behav Neurosci. 2014;8:1–9. doi:10.3389/fnbeh.2014.00243
- Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. 1981;2(2):99–113. doi:10.1002/job.4030020205
- Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52(1):397–422. doi:10.1146/annurev.psych.52.1.397
- Maslach C, Goldberg J. Prevention of burnout: new perspectives. Appl Prev Psychol. 1998;7(1):63–74. doi:10.1016/S0962-1849(98)80022-X
- Figley CR. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in Those Who Treat the Traumatized. New York: Taylor & F; 1995.
- Maslach C, Zimbardo PG. Burnout: The Cost of Caring. Englewood Cliffs, New Jersey: Prentice-Hall, Inc.; 1982.
- Maslach C, Jackson SE, Leiter MP. The maslach burnout inventory manual. In: Zalaquett CP, Wood R, editors. Evaluating Stress: A Book of Resources. The Scarecrow Press; 1999:191–217.
- Brockhouse R, Msetfi RM, Cohen K, Joseph S. Vicarious exposure to trauma and growth in therapists: the moderating effects of sense of coherence, organizational support, and empathy. J Trauma Stress. 2011;24(6):735–742. doi:10.1002/jts.20704
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–529. doi:10.1111/joim.12752
- Woo T, Ho R, Tang A, Tam W. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J Psychiatr Res. 2020;123:9–20. doi:10.1016/j.jpsychires.2019.12.015
- Correia I, Almeida AE. Organizational justice, professional identification, empathy, and meaningful work during COVID-19 pandemic: are they burnout protectors in physicians and nurses? Front Psychol. 2020;11:1. doi:10.3389/fpsyg.2020.566139
- Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Int Med. 2002;136:1. doi:10.7326/0003-4819-136-5-200203050-00008
- Bakhamis L, Paul DP, Smith H, Coustasse A. Still an epidemic: the burnout syndrome in hospital registered nurses. Health Care Manag. 2019;38(1):3–10. doi:10.1097/HCM.0000000000000243
- Wilkinson H, Whittington R, Perry L, Eames C. Examining the relationship between burnout and empathy in healthcare professionals: a systematic review. In: Burnout Research. Vol. 6. Elsevier GmbH; 2017:18–29.
- Zenasni F, Boujut E, Woerner A, Sultan S. Burnout and empathy in primary care. Br J Gen Pract. 2012;62(600):346–347. doi:10.3399/bjgp12X652193
- Lamothe M, Boujut E, Zenasni F, Sultan S. To be or not to be empathic: the combined role of empathic concern and perspective taking in understanding burnout in general practice. BMC Fam Pract. 2014;15(1):1. doi:10.1186/1471-2296-15-15
- Thirioux B, Birault F, Jaafari N. Empathy is a protective factor of burnout in physicians: new neuro-phenomenological hypotheses regarding empathy and sympathy in care relationship. Front Psychol. 2016;7:1–11. doi:10.3389/fpsyg.2016.00763
- Duarte J, Pinto-Gouveia J, Cruz B. Relationships between nurses’ empathy, self-compassion and dimensions of professional quality of life: a cross-sectional study. Int J Nurs Stud. 2016;60:1–11. doi:10.1016/j.ijnurstu.2016.02.015
- Yuguero O, Marsal JR, Esquerda M, Vivanco L, Soler-González J. Association between low empathy and high burnout among primary care physicians and nurses in Lleida, Spain. Eur J Gen Pract. 2017;23(1):4–10. doi:10.1080/13814788.2016.1233173
- Williams B, Lau R, Thornton E, Olney LS. The relationship between empathy and burnout – lessons for paramedics: a scoping review. Psychol Res Behav Manag. 2017;10:329. doi:10.2147/PRBM.S145810
- Decety J, Jackson PL. The functional architecture of human empathy. Behav Cogn Neurosci Rev. 2004;3:71–100. doi:10.1177/1534582304267187
- Decety J, Lamm C. Empathy versus personal distress: recent evidence from social neuroscience. In: Decety J, William I, editors. The Social Neuroscience of Empathy. Massachussetts: The MIT Press; 2009:199–214.
- Clark MA, Robertson MM, Young S. “I feel your pain”: a critical review of organizational research on empathy. J Organ Behav. 2019;40(2):166–192. doi:10.1002/job.2348
- R Core Team. European environment agency; 2020. Available from: https://www.eea.europa.eu/data-and-maps/indicators/oxygen-consuming-substances-in-rivers/r-development-core-team-2006. Accessed February 9, 2023.
- Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153–160. doi:10.1136/ebmental-2019-300117
- Laliberté E. Package “metacor” title meta-analysis of correlation coefficients; 2019. Available from: http://www.elaliberte.info/. Accessed February 9, 2023.
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2019; 36(3):1–48.
- Hong QN, Fàbregues S, Bartlett G, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–291.
- Beckman TJ, Reed DA, Shanafelt TD, West CP. Resident physician well-being and assessments of their knowledge and clinical performance. J Gen Intern Med. 2012;27(3):325–330. doi:10.1007/s11606-011-1891-6
- Bogiatzaki V, Frengidou E, Savakis E, Trigoni M, Galanis P, Anagnostopoulos F. Empathy and burnout of healthcare professionals in public hospitals of Greece. Int J Caring Sci. 2019;12(2):611–626.
- Carmel S, Glick SM. Compassionate-empathic physicians: personality traits and social-organizational factors that enhance or inhibit this behavior pattern. Soc Sci Med. 1996;43(8):1253–1261. doi:10.1016/0277-9536(95)00445-9
- Delgado N, Bonache H, Betancort M, Morera Y, Harris LT. Understanding the links between inferring mental states, empathy, and burnout in medical contexts. Healthcare. 2021;9(2):158. doi:10.3390/healthcare9020158
- Fülöp E, Devecsery Á, Hausz K, Kovács Z, Csabai M. Relationship between empathy and burnout among psychiatric residents. New Med. 2011;2011:143–147.
- Kelly-Hedrick M, Rodriguez MM, Ruble AE, Wright SM, Chisolm MS. Measuring flourishing among internal medicine and psychiatry residents. J Grad Med Educ. 2020;12(3):312–319. doi:10.4300/JGME-D-19-00793.1
- McManus IC, Jonvik H, Richards P, Paice E. Vocation and avocation: leisure activities correlate with professional engagement, but not burnout, in a cross-sectional survey of UK doctors. BMC Med. 2011;9(1):100. doi:10.1186/1741-7015-9-100
- Omdahl BL, O’ C, Phd D, O’donnell OBL. Emotional contagion, empathic concern and communicative responsiveness as variables affecting nurses’ stress and occupational commitment. J Adv Nurs. 1999;29:1. doi:10.1046/j.1365-2648.1999.01021.x
- Penšek L, Selič P. Empathy and burnout in Slovenian family medicine doctors: the first presentation of Jefferson scale of empathy results. Zdr Varst. 2018;57(3):155–165. doi:10.2478/sjph-2018-0020
- Salvarani V, Rampoldi G, Ardenghi S, et al. Protecting emergency room nurses from burnout: the role of dispositional mindfulness, emotion regulation and empathy. J Nurs Manag. 2019;27(4):765–774. doi:10.1111/jonm.12771
- Sturzu L, Lala A, Bisch M, Guitter M, Dobre D, Schwan R. Empathy and burnout - A cross-sectional study among mental healthcare providers in France. J Med Life. 2019;12(1):21–29. doi:10.25122/jml-2018-0050
- Lee PT, Loh J, Sng G, Tung J, Yeo KK. Empathy and burnout: a study on residents from a Singapore institution. Singapore Med J. 2018;59(1):50. doi:10.11622/smedj.2017096
- Seo HY, Lee DW, Nam S, et al. Burnout as a mediator in the relationship between work-life balance and empathy in healthcare professionals. Psychiatry Investig. 2020;17(9):951–959. doi:10.30773/pi.2020.0147
- Verweij H, van Ravesteijn H, van Hooff MLM, Lagro-Janssen ALM, Speckens AEM. Mindfulness-based stress reduction for residents: a randomized controlled trial. J Gen Intern Med. 2018;33(4):429–436. doi:10.1007/s11606-017-4249-x
- Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302:1. doi:10.1001/jama.2009.1384
- Lusilla-Palacios P, Castellano-Tejedor C. Training a spinal cord injury rehabilitation team in motivational interviewing. Rehabil Res Pract. 2015;2015:1–7.
- Winkel AF, Feldman N, Moss H, Jakalow H, Simon J, Blank S. Narrative medicine workshops for obstetrics and gynecology residents and association with burnout measures. Obstet Gynecol. 2016;128(4):27s–33s. doi:10.1097/AOG.0000000000001619
- Galam E, Soupault CV, Bunge L, Buffel du Vaure C, Boujut E, Jaury P. “Intern life”: a longitudinal study of burnout, empathy, and coping strategies used by French GPs in training. BJGP Open. 2017;1:2. doi:10.3399/bjgpopen17X100773
- Reed S, Kemper KJ, Schwartz A, et al. Variability of burnout and stress measures in pediatric residents: an exploratory single-center study from the pediatric resident burnout–resilience study consortium. J Evid Based Integr Med. 2018;23:5. doi:10.1177/2515690X18804779
- West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. J Am Med Assoc. 2006;296(9):1071–1078. doi:10.1001/jama.296.9.1071
- Altmann T, Roth M. The risk of empathy: longitudinal associations between empathy and burnout. Psychol Health. 2020;36(12):1441–1460. doi:10.1080/08870446.2020.1838521
- Kristensen TS, Borritz M, Christensen KB, Christensen KB. The Copenhagen burnout inventory: a new tool for the assessment of burnout. Work Stress. 2007;19(3):192–207. doi:10.1080/02678370500297720
- Spreng RN, McKinnon MC, Mar RA, Levine B. The Toronto empathy questionnaire: scale development and initial validation of a factor-analytic solution to multiple empathy measures. J Pers Assess. 2009;91(1):62–71. doi:10.1080/00223890802484381
- Schlegel K, Grandjean D, Scherer KR. Introducing the Geneva emotion recognition test: an example of Rasch-based test development. Psychol Assess. 2014;26(2):666–672. doi:10.1037/a0035246
- Van Doesum NJ, Van Lange DA, Van Lange PAM. Social mindfulness: skill and will to navigate the social world. J Pers Soc Psychol. 2013;105(1):86–103. doi:10.1037/a0032540
- Bakker AB, Demerouti E, Verbeke W. Using the job demands-resources model to predict burnout and performance. Hum Resour Manage. 2004;43(1):83–104. doi:10.1002/hrm.20004
- Salas-Wright CP, Olate R, Vaughn MG. Assessing empathy in Salvadoran high-risk and gang-involved adolescents and young adults: a Spanish validation of the basic empathy scale. Int J Offender Ther Comp Criminol. 2013;57(11):1393–1416. doi:10.1177/0306624X12455170
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi:10.1002/sim.1186
- Demerouti E, Nachreiner F, Bakker AB, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86(3):499–512. doi:10.1037/0021-9010.86.3.499
- Duarte J, Pinto-Gouveia J. Empathy and feelings of guilt experienced by nurses: a cross-sectional study of their role in burnout and compassion fatigue symptoms. Appl Nurs Res. 2017;35:42–47. doi:10.1016/j.apnr.2017.02.006
- Abu-Akel A, Palgi S, Klein E, Decety J, Shamay-Tsoory S. Oxytocin increases empathy to pain when adopting the other- but not the self-perspective. Soc Neurosci. 2015;10(1):7–15. doi:10.1080/17470919.2014.948637
- Klimecki OM, Leiberg S, Ricard M, Singer T. Differential pattern of functional brain plasticity after compassion and empathy training. Soc Cogn Affect Neurosci. 2013;9(6):873–879. doi:10.1093/scan/nst060
- Jordan MR, Amir D, Bloom P. Are empathy and concern psychologically distinct? Emotion. 2016;16(8):1107–1116. doi:10.1037/emo0000228
- Shapiro J, McDonald TB. Supporting clinicians during Covid-19 and beyond — learning from past failures and envisioning new strategies. N Engl J Med. 2020;383(27):e142. doi:10.1056/NEJMp2024834
- Cameron CD, Harris LT, Payne BK. The emotional cost of humanity: anticipated exhaustion motivates dehumanization of stigmatized targets. Soc Psychol Personal Sci. 2016;7(2):105–112. doi:10.1177/1948550615604453
- Murphy BA, Lilienfeld SO. Are self-report cognitive empathy ratings valid proxies for cognitive empathy ability? Negligible meta-analytic relations with behavioral task performance. Psychol Assess. 2019;31(8):1062–1072. doi:10.1037/pas0000732
- Stosic MD, Fultz AA, Brown JA, Bernieri FJ. What is your empathy scale not measuring? The convergent, discriminant, and predictive validity of five empathy scales. J Soc Psychol. 2022;162(1):7–25. doi:10.1080/00224545