Abstract
Background
There is evidence that adverse childhood experiences (ACEs) and negative life events (NLEs) are associated with major depression (MDD).
Purpose
To determine whether ACEs affect all features of mild MDD, including suicidal tendencies, brooding, neuroticism, insomnia, cognitive deficits, severity of depression and anxiety, and cognitive deficits, and whether NLEs mediate these effects.
Sample of the Study and Methods
This study examines a cohort of 118 academic students, namely 74 students who satisfied the DSM-5-TR criteria for MDD and 44 normal control students. We assessed brooding, neuroticism, suicidal ideation and attempts, and the severity of depression, anxiety, insomnia, and the Stroop tests.
Results
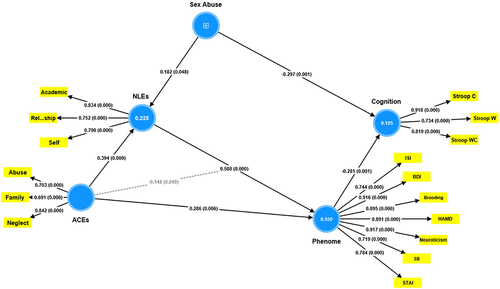
One validated factor could be extracted from brooding, neuroticism, current suicidal behaviors, and the severity of depression, anxiety, and insomnia, labeled the phenome of depression. A large part of the variance in the phenome of depression (55.0%) was explained by the combined effects of self-, relationships, and academic-related NLEs in conjunction with ACEs, including family dysfunction and abuse and neglect (both physical and emotional). The latter ACEs significantly interacted (moderating effect) with NLEs to impact the depression phenome. Although sexual abuse did not have direct effects on the phenome, its effects were mediated by NLEs. We discovered that increased sexual abuse, physical and emotional abuse and neglect, and ACEs related to family dysfunction predicted 22.5% of the variance in NLEs. Up to 18.5% of the variance in the Stroop test scores was explained by sexual abuse and the phenome of depression. The latter mediated the effects of NLEs and abuse, neglect, and family dysfunction on the Stroop test scores.
Conclusion
Complex intersections between ACEs and NLEs impact the phenome of depression, which comprises neuroticism, brooding, suicidal tendencies, and the severity of insomnia, anxiety, and depression, while sexual abuse together with other ACEs and NLEs may impact cognitive interference inhibition.
Introduction
Depressive episodes are reported by an approximate 4.7% of the worldwide populace within a 12-month timeframe, with the mean age of onset falling within the range of 17 to 37 years.Citation1 Depression is a condition that arises from an intricate interaction between genetic, biological, and psychosocial factors.Citation2 Depression is distinguished by depressed mood, diminished energy, loss of interest and insufficient daily activity for a minimum of two weeks. These symptoms are often accompanied by additional indications of mental and motor impairment, appetite fluctuations, insomnia, impaired concentration, feelings of worthlessness or unwarranted guilt, and recurrent suicidal ideation.Citation3,Citation4
There is substantial evidence to suggest that adverse childhood experiences (ACEs) are associated with a heightened likelihood of detrimental health outcomes, such as suicidal tendencies and depression.Citation5–9 ACEs encompass a range of challenges experienced during childhood and adolescence, such as physical, sexual, and emotional abuse; neglect (both physical and emotional); and exposure to dysfunctional households (including but not limited to domestic violence, and parental divorce, substance abuse, mental illness, or criminal behaviors).Citation10,Citation11 Neglect and emotional abuse considerably contribute more to the incidence of depression than other types of ACEs, such as sexual abuse and domestic violence, according to a recent meta-analysis.Citation12 In contrast, other meta-analysisCitation13 discovered a more robust association between depression and sexual and physical abuse compared to the aforementioned categories. Furthermore, ACEs have the potential to modify the default mode network, interfere with reward processing, and reduce the volume of the inferior frontal gyrus. These effects can result in compromised inhibitory control and emotional function.Citation14–16 A prospective cohort study discovered cognitive impairments and ACEs that were mediated in part by depressive symptoms.Citation5
Additionally, empirical support suggests that daily hassles and negative life events (NLEs) are correlated with symptoms of depression, negative affect, and neuroticism. NLEs and daily difficulties encompass disagreeable and anxiety-inducing obligations such as familial disputes, financial hardships, and work-related obligations.Citation17,Citation18 Cognitive dysfunction and emotional dysregulation, as well as an increased risk of developing psychopathology and late-life cognitive impairment, such as major depressive disorder (MDD), may result from daily hassles and exposure to NLEs.Citation19–25 MDD was predicted by increased daily hassles in a 14–24-year-old cohort.Citation23 MayberyCitation26 identified a correlation between perceived distress among university students and adverse interpersonal (eg, financial, and familial) and non-interpersonal (eg, academic) events. Longitudinal studies have found that cognitive impairments are significantly predicted by the severity and quantity of daily stressors.Citation20,Citation21 It was recently reported that NLEs partially mediate the effects of ACEs on the severity of depression.Citation27 This implies that ACEs increase the probability of developing NLEs, which in turn influences the severity of depression. However, the extent to which NLEs partially or completely mediate the effects of ACEs on the features of the phenome of depression (suicidal behaviors, rumination, neuroticism, insomnia, and cognitive deficits) is still unknown.
Consequently, the purpose of this research is to determine whether a) ACEs affect all characteristics of mild MDD in young adults, including suicidal tendencies, brooding, neuroticism, insomnia, cognitive deficits, and the severity of depression and anxiety; and b) whether NLEs partially or wholly mediate these effects. Furthermore, we examine whether solitary ACEs or the combined effects of ACEs are better predictors of the depression phenome. We intend to develop a mediation model that establishes the connection between ACEs and NLEs and depression characteristics, which could be utilized in clinical practice to predict suicidal tendencies and depression. In pursuit of this objective, we model the relationships between all features of the depression phenome using the nomothetic precision psychiatry approach.Citation27,Citation28 The latter is a new statistical approach developed by Michael Maes to construct new models of mental disease, including MDD, based on the causes (eg psychosocial stressors), and all phenome features (eg all lifetime and current symptoms and phenomenology as well) of the disease. To assemble a representative sample of individuals diagnosed with mild major depressive disorder (MDD) uncomplicated by chronic depression, we opted to enlist academic students whose mean age corresponds to the onset of depressive symptoms.Citation1
Materials and Methods
Participants
G*Power 3.1.9.4 was utilized to determine the a priori sample size. The following parameters were established for the case-control study: an analysis of covariance with the following characteristics: f = 0.3 effect size, alpha = 0.05 power, number of groups = 3, and variables = 6. Consequently, a minimum sample size of 111 participants was estimated. We conducted a study that included students of various genders and ages from different faculties (ie, law, science, medicine, veterinary science, psychology, and engineering) at Chulalongkorn University in Bangkok, Thailand. Recruiting occurred when students sought consultations at the department of psychiatry in order to receive treatment for their symptoms of depression. Therefore, we gathered a representative sample of Thai undergraduates pursuing scientific and social science degrees who seek treatment for depression in an outpatient setting.
From November 2021 to February 2023, a cohort of 118 Thai-speaking individuals was enrolled in this research investigation at the outpatient Department of Psychiatry, King Chulalongkorn Memorial Hospital, Bangkok, Thailand. This study enrolled individuals who satisfied the DSM-5-TRCitation3 criteria for depressive episode, as diagnosed by senior psychiatrists. Additionally, participants who obtained a Hamilton Depression Rating Scale (HAM-D)Citation29 score over 7, as assessed by a clinical psychologist with adequate training, were eligible to participate. For their own protection, participants who exhibited signs of suicidal ideation during the interview phase were ineligible for inclusion in the study and were instead referred to a psychiatrist. The study excluded psychiatric diagnoses such as schizophrenia, alcohol or drug abuse disorders, psycho-organic disorders, anxiety disorders, autism, bipolar disorder, and schizoaffective disorder, in addition to current medical conditions including endocrine or autoimmune disorders, psoriasis, type 1 diabetes, lupus erythematosus, chronic kidney disease, multiple sclerosis, and carcinoma. Female students who were pregnant or nursing were not permitted to take part in the study. Seventy-four patients suffering from an acute phase of major depression were enrolled. Through word-of-mouth and online advertisements, 44 healthy controls devoid of psychiatric diagnoses and suicidality at any point in their lives were recruited for this study. Recruited were controls with a HAM-DCitation29 score of 7 or below.
The Institutional Review Board (IRB) of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand, reviewed and approved this study (IRB No.351/63) which is in compliance with the International Guideline for Human Research protection as required by the Declaration of Helsinki, The Belmont Report, CIOMS Guideline and International Conference on Harmonization in Good Clinical Practice (ICH-GCP). Consent in writing was obtained from every participant.
Methods
The students involved in the study were instructed to complete semi-structured interviews regarding sociodemographic information such as age, gender, number of years of education, current smoking status, lifetime history of COVID-19 infection, family history of psychiatric diagnoses (including major depression, bipolar disorder, anxiety, and psychosis), and suicidality. For the computation of body mass index (BMI), weight (kg) and height (m) were acquired. The prevalence of childhood adversities was evaluated for all participants through the utilization of the Adverse Childhood Experiences (ACEs) Questionnaire, as developed by Felitti et al.Citation10 Abuse (emotional, physical, and sexual), neglect (emotional and physical), household dysfunction (including domestic violence, substance abuse, mental illness, parental divorce, and criminal members in the household) were the categories applied to a self-report consisting of 28 items. The ACEs Questionnaire underwent a validated Thai translation by Rungmueanporn et al.Citation30 The Thai version of the questionnaire demonstrated internal consistency reliability values of 0.79 for the abuse domain, 0.82 for the neglect domain, and 0.66 for the household dysfunction domain.
The Negative Event Scale (NES) was employed to quantify the degree of NLEs.Citation26 The self-report questionnaire comprises 42 items, each assigned a score between 0 (indicating the event did not transpire) and 5 (indicating the event transpired with significant problems). The questionnaire assesses four non-interpersonal subscales (health, money, course interest, and academic limitation) and seven interpersonal subscales (friends, boyfriend/girlfriend, parents, relatives, lecturers, and fellow students) that are linked to the current (1-month period) NLEs. The scale, back-translated into Thai by BoonyamalikCitation31 demonstrated high reliability among Thai adolescents, as evidenced by Cronbach’s alpha values ranging from 0.94 to 0.96.
The present study utilized the subsequent rating scales to evaluate the phenome of depression. The symptoms and severity of depression were assessed using the Thai version of the HAM-D,Citation29 which was translated by Lotrakul et alCitation32 (17 items, ranging from not present (0) to severe (3)). Self-rating of depression was assessed using the Beck Depression Inventory-II (BDI-II),Citation33 translated by MungpanichCitation34 (21 items, ranging from 0 (not present) to 4 (severe)). Both Thai versions have a high degree of internal consistency (Cronbach’s alpha of 0.74 and 0.91, respectively).Citation32,Citation34 The Thai version of the State-Trait Anxiety Inventory (STAI)Citation35 was developed by Iamsupasit and Phumivuthisarn.Citation36 The STAI comprises twenty items that request respondents to assess their level of state anxiety on a four-point Likert scale ranging from “not at all” (1) to “mostly” (4). The Thai version has good internal consistency with a Cronbach’s alpha coefficient ranging from 0.86 to 0.92. The Thai translation of the Insomnia Severity Index (ISI),Citation37 a self-rating questionnaire utilized to evaluate the severity of sleep problems, was provided by the Mapi Research Trust.Citation38 The ISICitation37,Citation38 is comprised of seven Likert-scale items, where responses span from “no problem” (0) to “very severe problems” (4). It displays excellent internal consistency in both community and clinical samples (Cronbach’s alpha of 0.90 and 0.91 respectively). The Ruminative Response Scale (RRS),Citation39 which was translated into Thai by Thanoi et al,Citation40 comprises 22 items utilized to assess reflective rumination and pondering. Responses range from almost never (1) to almost always (4); the scale shows good internal consistency (Cronbach’s alpha of 0.90). The total score of eight questions from the Thai version of The International Personality Item Pool-NEO (IPIP-NEO)Citation41 was utilized to assess neuroticism, one of the Big Five personality traits, in this research investigation. The Thai version was translated by Yomaboot and CooperCitation42 and utilized items with a Cronbach’s alpha coefficient of 0.83. The researchers utilized the Columbia-Suicide Severity Rating Scale (C-SSRS)Citation43 to assess both past (up to one month prior to study enrollment) and present suicidal tendencies (within one month). The severity and intensity of suicidal ideation, the self-harm and attempt subscales, and the lethality subscale comprise the four components of the C-SSRS. The Columbia Lighthouse ProjectCitation44 translated the Thai version of this scale has high sensitivity and specificity of 95% in suicidal behavior classifications.
Previous studies have established that the traditional Stroop task yielded a significant effect size when used to compare cognitive impairments in patients with clinical depression to those in the control group.Citation45 Hence, the present investigation utilized the Stroop Color and Word Test (SCWT)Citation46 to evaluate cognitive interference. The SCWT comprises three stimulus sheets, which feature word, color, and word-color stimuli. Participants are given the task of rapidly identifying the colors of the ink or reading text. Body mass index (BMI) was computed as weight (in kg) divided by length (in meter) squared.
Statistical Analyses
The statistical analysis for this study is conducted utilizing IBM, SPSS windows version 29. The researchers utilized a contingency table analysis (Χ2-test) to evaluate the statistical associations among categorical variables. Utilizing Pearson’s product-moment correlation coefficients, the statistical relationships between continuous variables were ascertained. Analysis of variance was employed to investigate the relationships between diagnostic categories and clinical data. The researchers utilized analysis of covariance (ANCOVA) to investigate the variation in cognitive variables between groups while covarying for age, sex, and years of education. We used regression analysis to delineate the effects of different ACEs and NLEs on the clinical characteristics of depression. To reduce the number of items into a principal component (PC) score that could be utilized in subsequent statistical investigations, PC analysis (PCA) was implemented. Utilizing Bartlett’s sphericity test and the Kaiser-Meyer-Olkin (KMO) test for sample adequacy, factorability was ascertained; a KMO value greater than 0.6 indicates adequate sample adequacy. Acceptance of the initial PC is contingent upon the variance explained (VE) exceeding 50% and all loadings surpassing 0.66.
Using partial least squares (PLS) path analysis (SmartPLS),Citation47 the causal relationships between latent vectors derived from ACEs, NLEs, cognition, and the depressive phenome were evaluated. PLS path analysis was conducted exclusively on the condition that both the inner and outer models met predetermined quality criteria: a) all loadings on the latent vectors must be greater than 0.66 at a significance level of p<0.001; b) the model fit must be satisfactory when the standardized root mean square residuals (SRMR) do not exceed 0.08; c) all latent vectors must possess adequate composite reliability (>0.7) and Cronbach’s alpha (>0.6) values, with an average variance extracted (AVE) exceeding 0.50; d) the reflective models must not be incorrectly specified. We utilized the Heterotrait-Monotrait ratio (HTMT) with a significance level of 0.85 to assess the discriminant validity of the constructs. A complete PLS analysis was conducted utilizing 5000 bootstrap samples to ascertain the exact p-values associated with the path coefficients for specific, total indirect, and direct paths.
Results
Results of PCA
We were unable to extract one validated PC from all ACEs items or subtypes. Nonetheless, we managed to isolate a single PC (referred to as “PC ACEs”) from the cumulative score of the emotional abuse, physical abuse, emotional neglect, and physical neglect subcategories, as illustrated in . We constructed four PCs based on specific sets of items: a) The ACEs abuse items 1, 2, 3, and 4, which represent emotional and physical abuse (referred to as “PC-ACE abuse”) (KMO=0.776, Bartlett’s sphericity test χ2 =121.660, df=6, p<0.001, VE=57.66%, all loadings>0.740). b) The items 5, 6, and 7, which indicate sexual abuse (referred to as “PC-ACE sexual abuse”) (KMO=0.639, Bartlett’s sphericity test χ2 =178.575, df=3, p<0.001, VE=76.14%, all loadings>0.781). c) The items 9, 10, 11, 12, 13, and 15, which represent emotional and physical neglect (referred to as “PC-ACE neglect”) (KMO=0.896, Bartlett’s sphericity test χ2 =616.214, df=15, p<0.001, VE=77.44%, all loadings>0.821). d) The “PC-ACE family”, which reflects household dysfunction, including domestic violence, mental illness in the household, and parental divorce subtypes (KMO=0.618, Bartlett’s sphericity test χ2 =23.269, df=3, p<0.001, VE=51.54%, all loadings>0.717). The Electronic Supplementary File (ESF), provides a comprehensive explanation of all ACEs items.
Table 1 Results of Principal Component (PC) Analyses and Construction of Adverse Childhood Experiences (ACEs) and Negative Life Event (NLE) Principal Components (PCs)
In addition, we were unable to extract one PC from all NLE items. As a result, we recovered three validated PCs and assigned them the labels “PC-NLE self”, “PC-NLE relationship”, and “PC-NLE academic”, as shown in and ESF, . The total score of all NLEs items was computed (labeled total NLEs).
Based on prior studies,Citation8,Citation28,Citation48 we created a reliable and validated psychological construct (PC) to represent the phenome of depression. This construct was developed by considering the combined scores from different measures such as HAM-D, BDI-II, STAI, ISI, neuroticism, brooding, and suicidal behavior (SB).Citation28 For more details, please refer to and ESF, . Furthermore, presents a PC that was created using three Stroop Color-Word Test (SCWT)Citation49 domains: word, color, and word-color. This PC accurately represents the capacity to suppress cognitive interference, which is labelled as PC Stroop.
Table 2 Demographic and Clinical Data of Patients with Major Depression (MDD) with High versus Low Adverse Childhood Experiences (ACEs), and Healthy Controls (HC)
Socio-Demographic and Clinical Data
displays the socio-demographic and clinical data. The group of patients with MDD was categorized into two subgroups based on their ACEs levels, specifically those with high ACEs and those with low ACEs. This categorization was done using the median-split approach performed on PC ACEs. Depressive patients did not show any significant differences compared to the control group in terms of age, sex, BMI, relationship status, current smoking, or lifetime COVID-19 history. Depressive patients with high ACEs had a downward trend in their level of education compared to other individuals. There were no significant differences observed between patients with high and low ACEs in terms of the length of depression, and family history of mental disorders such as depression, bipolar disorder, anxiety, psychosis, and suicide.
Clinical Features of Patients with High and Low ACEs
provides a comprehensive overview of the clinical characteristics exhibited by both patients and controls. Patients had significantly elevated scores on the HAM-D, BDI-II, STAI, ISI, brooding, neuroticism, present phenome, and SB measures, in comparison to the control group. Patients with elevated ACEs had significantly higher scores on the HAM-D and BDI-II, as well as greater rates of both current and total SB. Additionally, these patients reported a higher prevalence of NLEs in their relationships compared to patients with MDD who had low ACEs scores. The patients had significantly lower Stroop subdomains and cognition scores compared to the controls.
Table 3 Clinical Features of Patients with Major Depression (MDD) with High versus Low Adverse Childhood Experiences (ACEs) and Healthy Controls (HC)
Intercorrelation Matrix
displays the associations between PC ACEs, PC-ACE sexual abuse and PC-ACE family, as well as total scores of NLEs, and various clinical features of depression. These features include HAM-D, BDI-II, STAI, ISI, brooding, neuroticism, present phenome, lifetime and current SB, and cognition. Positive correlations were found between PC ACEs and total NLEs with all clinical characteristics, but negative associations were observed with cognition. The PC-ACE sexual abuse showed a strong negative correlation with cognitive abilities, while it exhibited a positive correlation with the total scores of NLEs, ISI, and lifetime SB. PC ACEs, Total NLEs, and PC-ACE family (excluding cognition) were strongly linked to every aspect of depression.
Table 4 Correlation Matrix Between Adverse Childhood Experiences (ACEs) and Negative Life Events (NLEs) and Other Clinical Features of Depression
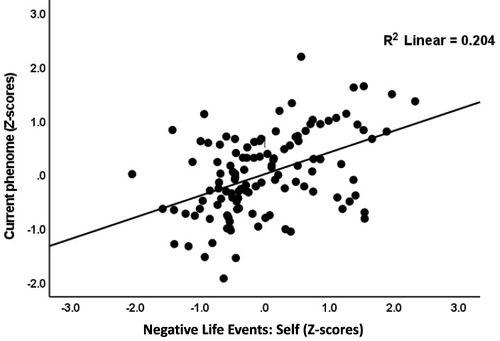
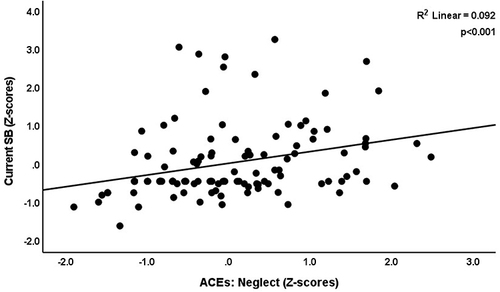
We conducted multiple regression analyses to examine the relationship between the current phenome, including current SB, and cognitive impairments. We included age, sex, number of education years, current regular smoking, and PCs of ACEs and NLEs subtypes as explanatory factors. The results are presented in . The stepwise technique revealed that the current phenome (#regression 1) was most accurately predicted by PC-NLE self, PC-NLE academic, and PC-ACE abuse, which collectively accounted for 53.4% of its variability. The most accurate predictors of current SB were PC-ACE neglect and PC-ACE family, which accounted for 17.8% of the observed variation in the data (regression 2). In Regression #3, specifically, the predictor variable of PC-NLE relationship accounted for 15.5% of the variance in current SB. The cognitive PC (#regression 4) was most accurately predicted by PC-ACE sexual abuse, PC-ACE neglect, and current smoking, which collectively accounted for 18.5% of the variability. displays the partial regression analysis of the present phenome on PC-NLE self, while accounting for the influences of age, sex, number of schooling years, and current smoking. displays the partial regression analysis of current SB on PC-ACE neglect, while accounting for the influence of age, sex, number of schooling years, and current smoking.
Table 5 Results of Multiple Regression Analyses with Current Phenome, Suicidal Behaviors and Neurocognition as Dependent Variables and Adverse Childhood Experiences (ACEs) and Negative Life Events (NLEs) as Input Variables
Results from PLS Analysis
displays the final PLS model, highlighting the significant paths. Based on prior research,Citation8,Citation28,Citation48 we create a latent vector representing the phenome of depression using the HAM-D, BDI-II, STAI, ISI, brooding, neuroticism, and current SB scores. We successfully developed a factor by considering ACEs abuse, neglect, and familial dysfunctions. We created a validated latent vector for NLEs by utilizing self, relationships, and academic scores. The three Stroop domains were utilized to form a cognitive factor. We utilized the ACEs and NLEs factors and sexual abuse as indicators for predicting the depression phenome and cognitive functioning. Additionally, we examined how NLEs can work as mediators for the impact of ACEs on the phenome. In addition, we incorporated a moderator model that encompasses the ACEs factor and the impact of NLEs on the phenome. The model fit indicates a satisfactory level of quality, as evidenced by the SRMR value of 0.058. The ACEs, NLEs, current phenome, and cognition factors demonstrate sufficient construct validity and convergence. The AVEs for these factors are 0.560, 0.629, 0.708, and 0.684, respectively. The Cronbach’s alpha values for these factors are 0.610, 0.704, 0.929, and 0.766, respectively. Additionally, the composite reliability (rho_C) values for these factors are 0.791, 0.835, 0.944, and 0.866, respectively. All loadings of the outer model exceeded 0.7, except for family difficulties, which had a loading of 0.692. The ACEs and NLEs factors accounted for 55.0% of the phenome variance, while the ACE indicators explained 22.5% of the NLEs variance. Sexual abuse and the phenome factor accounted for 18.5% of the variance in the cognition factor. The moderation term “ACEs X NLEs” was significant. The ACEs factor had a significant specific indirect effect on cognition, which was mediated via the pathway from the NLEs factor to the phenome factor (t=2.38, p=0.017). Furthermore, the NLEs factor had a specific indirect impact on the cognition factor mediated by the phenome, as evidenced by a statistically significant t-value of 2.88 and a p-value of 0.004. The PLS Predict analysis indicated that all Q2 values were above zero. Additionally, the PLS cross-validated predictive ability test analysis revealed that the PLS-SEM against indicator average had a significant result (p=0.008), suggesting that the model is replicable.
Figure 3 Results of PLS analysis. The significant pathways are presented, including the path coefficients (along with their exact p values) of the inner model and the loadings (with p values) of the outer model. One factor was extracted from the subcategories in adverse childhood experiences (ACEs), such as abuse, neglect, and family dysfunction. Sexual abuse was included as a single indicator (denoted as +). Negative life events (NLEs), the depression phenome, and cognition were entered as latent vectors extracted from their manifestations. Figures in blue circles indicate explained variances. Shown are path coefficients (with p values) and factor loadings (with p values). “Abuse” reflects the emotional and physical abuse subcategories of ACEs; “Neglect” reflects the emotional and physical neglect subcategories of ACEs; “Family” reflects household dysfunction, including domestic violence, mental illness in the household, and parental divorce subcategories of ACEs; “Self” reflects NLEs self-subcategories, such as hassles in health issues and insufficient money; “Academic” reflects NLEs academic-subcategories, such as hassles in academic course, course interest, and limitation in academic ability; “Relationship” reflects NLEs relationship-subcategories, such as hassles with friends, parents, relatives, and other students.
Discussion
Effects of ACEs on the Depression Phenome
The first important finding from this research is that ACEs were substantially correlated with the phenome of depression. Our research distinguished the various ACEs types using a data-centric approach and identified the significant pathways by which ACEs may influence the phenome via PLS analysis. The latter analysis allowed us to extract latent vectors from physical and emotional abuse and neglect as well as family problems, and from different NLEs, and to compute that these constructs together had a substantial, significant direct effect on the phenome, explaining 55.5% of the variance. These results build upon the conclusions drawn by Almulla et al,Citation22 which indicated that ACEs could predict the phenome of depression. Consistent with previous research (eg, Hein et al;Citation50 Peckins et al;Citation51 Gizdic et al),Citation52 our findings demonstrate that distinct subtypes of ACEs are associated with psychopathology in unique ways. Prior studies have established a correlation between neglect, physical and emotional maltreatment, and an elevated susceptibility to psychological and behavioral complications, including depression and suicidal ideation.Citation53 Similarly, an increase in depressive symptoms is correlated with higher cumulative ACEs scores.Citation54 The threat-deprivation model, alternatively referred to as the Dimension Model of Adversity and Psychopathology, elucidates the biological mechanisms that underlie a multitude of ACEs.Citation14,Citation55 Threat is defined as initial exposure to violence or injury, while deprivation is characterized by the absence of anticipated demands from one’s surroundings.Citation14,Citation55 There is evidence that individuals who are threatened or deprived may display increased emotional reactivity and struggle to regulate their emotions.Citation56 This has been associated with symptoms of anxiety and depression.Citation57,Citation58 Moreover, there is a positive correlation between physical abuse history and poverty among adultsCitation59 which is linked to depression and anxiety.Citation60 According to Dube et al,Citation11 ACEs are strongly associated with suicide attempts.
Furthermore, by incorporating the ACEs items pertaining to parental divorce, domestic violence, mental illness, and suicide within the household, our research successfully constructed a validated family dysfunction factor. A potential explanation for the high loadings of those different items on the latter factor is that all items could be attributed to hereditary influences. This factor exhibits a significant association with every characteristic of depression, except for cognitive dysfunctions. MDD patients exhibit heritability ranging from 30% to 50% explained variance, suggesting that genetics significantly impact the development of depression.Citation61 Furthermore, there is evidence to suggest that parental mental health issues account for around 50% of the genetic transmission of suicide attempts.Citation62 Furthermore, completed suicide has been linked to genetic factors.Citation63 Therefore, it is probable that the existence of mental disorders, regardless of their genetic predisposition, contributed to domestic violence and parental divorce, as well as to the exacerbation of depression symptoms such as suicidal ideation, brooding, insomnia, and overall severity of the condition.
Effects of Sexual Abuse on the Depression Phenome
The results of our study indicate that sexual abuse did not have a statistically significant direct impact on the phenome of depression. However, it did have a minimal effect size on lifetime SB and ISI scores. These results are consistent with those of Gizdic et al,Citation52 who discovered no association between sexual abuse and psychopathology using PCA. However, our research revealed that sexual abuse exerted a substantial indirect influence on the phenome of depression, and that this influence was mediated by NLEs. Positive results indicating a significant association between childhood sexual abuse and depression are also explicable by this effect. As an illustration, a longitudinal investigation conducted by Ferguson et alCitation64 identified a correlation that was statistically significant between sexual abuse and various socioecological outcomes pertaining to adult development, including psychological well-being, sexual risk-taking, and physical health. Sexual abuse was statistically associated with a lifetime diagnosis of psychiatric disorders, including anxiety disorder, depression, eating disorders, posttraumatic stress disorder, sleep disorders, and suicide attempts, according to meta-analysis and longitudinal study.Citation65,Citation66 A higher probability of exhibiting symptoms consistent with severe depression was found in individuals whose sexual abuse took place prior to the age of twelve, according to a study by Schoedl et alCitation67 Adams et alCitation68 discovered that, unlike during childhood and adolescence, a prior history of sexual abuse prior to the age of six did not exhibit a significant predictive effect on psychopathology.
Combined Effects of ACEs and NLEs on the Phenome of Depression
A third significant finding of the present study is that ACEs and NLEs are predictors of the MDD phenotype, which includes suicidal behaviors. Self- and academic-related difficulties in conjunction with ACEs predicted the depression phenome, whereas neglect, family dysfunction, or relationship difficulties predicted current suicidal behaviors. Chronic stress can be induced by everyday difficulties, particularly when these difficulties coincide with other personal and environmental risk factors that increase the likelihood of developing mental disorders.Citation23 Previous studies have established clear associations between NLEs and neuroticism,Citation69 brooding,Citation70,Citation71 poor sleep quality,Citation70,Citation72 suicide,Citation27,Citation71 and all of these factors are known to increase the likelihood of developing depression.Citation23,Citation24,Citation73
Furthermore, increased NLEs were found to partially mediate the effects of ACEs on rumination, SB, neuroticism, and the phenome of depression, according to the current study. Almulla et alCitation22 discovered that NLEs combined with ACEs substantially predict the manifestation of very severe MDD, as well as the lifetime and current suicidal behaviors. These results build upon those of Almulla et al.Citation22 The effects of ACEs on the increases in affective symptoms during the COVID-19 pandemic are partially mediated by increased NLE scores.Citation74 Maes and AlmullaCitation27 identified a similar pattern to the present study: ACEs predict the severity of NLEs, and the latter are correlated with heightened illness severity and recent suicidal behaviors. As previously mentioned, individuals who have experienced ACEs are more likely to reside in environments that are more problematic, which increases their exposure to NLEs.Citation27
Furthermore, we identified a noteworthy moderating effect in which dysfunctions within the family and physical and emotional neglect and abuse serve as moderators to diminish the impact of NLEs on the phenome of depression. Another study that documented this moderation effect was Maes and Almulla.Citation27 The latter authors proposed the moderation effect depends on the number of ACEs, whereby a higher number of ACE may be linked to NLE having less of an effect.
ACEs Predict Cognitive Impairments in MDD
The fourth significant discovery of this research is that ACEs are notably correlated with cognitive impairments in individuals with depression. Significantly, our research revealed that various ACEs had distinct impacts on cognitive impairments associated with depression. Specifically, sexual abuse had direct effects, while neglect and family issues and a combination of physical and emotional abuse had indirect effects. The latter effects were mediated in part by NLEs and the depressive phenome.
The Classic Stroop test was employed in this investigation as it was deemed a reliable benchmark for depression in a prior meta-analysis.Citation45 Cognitive interference occurs when the processing of one attribute influences the simultaneous processing of another attribute in response to the same stimuli.Citation46,Citation75 The Stroop test measures the capacity to prevent cognitive interference. Interference control is a critical cognitive principle that is potentially indispensable for numerous memory tasks and exhibits connections with other cognitive processes.Citation76 Like working memory and set shifting (flexibility), inhibitory control is an essential component of the executive functions, which are higher-order cognitive processes.Citation77 Thus, our findings extend those of Tjoelker et al,Citation78 who found that a history of physical maltreatment and emotional neglect is associated with diminished interference control in older individuals with depressive, anxious, and somatic symptoms. A significant correlation was identified by Lund et alCitation79 in a systematic review between ACEs and executive deficits in children, specifically in relation to maternal depression. According to a study by Saleh et al,Citation80 exposure to ACEs negatively impacted working memory performance and processing speed. In a study of adults aged 18–45 years, both with and without MDD, who had been exposed to ACEs before the age of 13, Gould et alCitation81 found that ACEs may cause impairments in affective processing/inhibition, spatial working memory, and executive functions. Furthermore, ACEs have the potential to induce cognitive dysfunctions, disrupt reward systems, promote avoidant-emotion coping, and reduce problem-focused coping strategies. These combined effects may heighten an individual’s susceptibility to NLEs.Citation11,Citation14,Citation82
Significantly, our PLS analysis revealed that sexual abuse exerted a considerable direct impact on cognitive impairments. These results build upon the research conducted by Barrera et al,Citation83 which suggested that children who have been subjected to sexual assault might struggle to maintain focus. Further supporting the results are those of Hawkins et al,Citation84 who found that neglect and sexual abuse were associated with decreased performance on short-term and long-term memory assessments among individuals aged 24–32.
Different Pathways May Explain the Effects of ACEs/NLEs on the Phenome of Depression
The impact of physical and emotional abuse and neglect on the manifestation of depression could potentially be elucidated through the influence of ACEs on various cognitive function-affecting pathways. ACEs may increase the production of M1 macrophages and T-helper (Th) cells, specifically Th-1 and Th-17 cells, thereby activating the immune-inflammatory response system (IRS), while diminishing neuroprotective factors such as nerve growth factor.Citation9,Citation85 Furthermore, nitro-oxidative pathways are stimulated, and antioxidant defenses are compromised by ACEs.Citation86–88 Furthermore, research suggests that ACEs, such as neglect, could potentially interfere with the functioning of the hypothalamic-pituitary-adrenal (HPA) axis.Citation89,Citation90 Fourthly, childhood exposure to domestic violence shortened telomere length, according to a meta-analysisCitation91 and ACEs can alter epigenetic methylation patterns of HPA-axis-related genes.Citation92 Furthermore, it has been observed that ACEs are linked to alterations in the microbiome, which result in a distinct enterotype reflecting dysbiosis of the gut.Citation7 ACEs elevate atherogenicity, a factor that has been linked to suicidal tendencies and depression.Citation93 Finally, ACEs have been linked to reduced volume in the amygdala, hippocampus, and anterior cingulate cortex—regions of the brain responsible for emotion regulation and self-control—along with impairments in executive functions, which are indicative of impaired memory and cognitive flexibility.Citation6,Citation25,Citation84,Citation94–96
The potential impact of sexual abuse on neurocognitive function could be accounted for by the known cognitive function-altering effects of ACEs on various pathways, such as inflammation,Citation66,Citation88,Citation97 alterations in the HPA-axis,Citation97 and disruptions in the cortical and subcortical regions.Citation98 Likewise, NLEs have a plethora of detrimental effects on the same pathways, including the IRS,Citation99,Citation100 oxidative stress pathways,Citation101 HPA-axis function,Citation102 and methylation processes.Citation102
Limitations
Our research was limited to depression among university students between the ages of 18 and 35; consequently, the findings might not be applicable to chronic and recurrent depression, and depression in old age. Furthermore, the age of initial exposure to ACEs was not included in the Thai version of the Adverse Childhood Experiences Questionnaire,Citation10,Citation30 which was utilized in this research. Third, recall bias may be present due to the retrospective nature of the ACEs assessment in this study.Citation103 While some may contend that a more substantial sample size is imperative for examining the associations between ACEs/NLEs and the phenome, our research utilized a sample size that possessed an adequate power of 0.8. Furthermore, the association between ACEs/NLEs and the phenome has a post-hoc power of 1.0. Furthermore, the model exhibited replicability and the fit quality of the data was satisfactory. Further investigation into associated biomarkers is necessary to establish a more precise intervention strategy, given the involvement of ACEs in neurobiological pathways. While our study sample is representative of undergraduate students from scientific and social science faculties seeking help for mild depression, it may not be representative of MDD, depression in older age, different cultures, or other countries. It is possible that there are differences in the connections between psychosocial stressors and the MDD phenotype among various populations. Hence, it is important to replicate our findings in various cultural and geographical settings. In addition, other elements apart from ACEs and NLEs could play a role in the development of MDD, such as coping mechanisms, social support, family dynamics, and parental upbringing.
Conclusions
A significant proportion of the variability observed in the phenome of depression was accounted for by the combined influence of ACEs, including family dysfunction, abuse, and neglect (both physical and emotional), and self-, relationship, and academic-related NLEs. ACEs interacted substantially with NLEs to influence the depression phenome. While sexual abuse did not exert a direct influence on the phenome, its consequences were mediated through NLEs. We discovered that increased sexual abuse, physical and emotional abuse and neglect, and family dysfunction-related adverse childhood experiences predicted 22.5% of the variance in NLEs. Sexual abuse and depression as a phenotype accounted for as much as 18.5% of the variance in Stroop test scores. Sexual abuse coupled with other ACEs and NLEs may have an effect on cognitive interference inhibition. These findings have important practical implications for the clinical practice. Since a large part of the variance in the MDD phenome is explained by NLEs and ACEs, treatments of MDD should target coping with these NLEs and deprogramming the effects of ACEs. Future research should focus on the biological pathways underlying the effects of ACEs and NLEs on the phenome of depression, including activated neuro-immune pathways.Citation22
Ethics Statement
The studies involving humans were approved by The Institutional Review Board of Chulalongkorn University’s institutional ethics board, Bangkok, Thailand. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
This paper has been uploaded to medRxiv as a preprint: https://www.medrxiv.org/content/10.1101/2024.01.04.24300880v1. Asara Vasupanrajit and Michael Maes are joint first authors.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Additional information
Funding
References
- Herrman H, Patel V, Kieling C, et al. Time for united action on depression: a lancet-world psychiatric association commission. Lancet. 2022;399(10328):957–1022. doi:10.1016/s0140-6736(21)02141-3
- Lopizzo N, Bocchio Chiavetto L, Cattane N, et al. Gene-environment interaction in major depression: focus on experience-dependent biological systems. Front Psychiatry. 2015;6:68. doi:10.3389/fpsyt.2015.00068
- American Psychiatric Association. Depressive Disorders. Diagnostic and statistical manual of mental disorders (5th ed. text rev); 2022.
- World Health Organization. ICD-11: international classification of diseases (11th revision); 2022.
- Lowry E, McInerney A, Schmitz N, Deschênes SS. Adverse childhood experiences and cognitive function in adulthood: examining the roles of depressive symptoms and inflammation in a prospective cohort study. Soc Psychiatry Psychiatric Epidemiol. 2022;57(12):2367–2377. doi:10.1007/s00127-022-02315-w
- Soares S, Rocha V, Kelly-Irving M, Stringhini S, Fraga S. Adverse Childhood Events and Health Biomarkers: a Systematic Review. Front Public Health. 2021;9:649825. doi:10.3389/fpubh.2021.649825
- Maes M, Vasupanrajit A, Jirakran K, et al. Adverse childhood experiences and reoccurrence of illness impact the gut microbiome, which affects suicidal behaviours and the phenome of major depression: towards enterotypic phenotypes. Acta Neuropsychiatr. 2023;35(6):328–345. doi:10.1017/neu.2023.21
- Jirakran K, Vasupanrajit A, Tunvirachaisakul C, Maes M. The effects of adverse childhood experiences on depression and suicidal behaviors are partially mediated by neuroticism: a subclinical manifestation of major depression. Front Psychiatry. 2023;14:1158036. doi:10.3389/fpsyt.2023.1158036
- Maes M, Rachayon M, Jirakran K, Sodsai P, Sughondhabirom A. Lower nerve growth factor levels in major depression and suicidal behaviors: effects of adverse childhood experiences and recurrence of illness. Brain Sci. 2023;13(7). doi:10.3390/brainsci13071090
- Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi:10.1016/s0749-3797(98)00017-8
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the adverse childhood experiences study. JAMA. 2001;286(24):3089–3096. doi:10.1001/jama.286.24.3089
- Mandelli L, Petrelli C, Serretti A. The role of specific early trauma in adult depression: a meta-analysis of published literature. Childhood trauma and adult depression. Eur Psychiatry. 2015;30(6):665–680. doi:10.1016/j.eurpsy.2015.04.007
- Lindert J, von Ehrenstein OS, Grashow R, Gal G, Braehler E, Weisskopf MG. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. Int J Public Health. 2014;59(2):359–372. doi:10.1007/s00038-013-0519-5
- McLaughlin KA, Sheridan MA. Beyond cumulative risk: a dimensional approach to childhood adversity. Curr Dir Psychol Sci. 2016;25(4):239–245. doi:10.1177/0963721416655883
- Luby JL, Barch D, Whalen D, Tillman R, Belden A. Association between early life adversity and risk for poor emotional and physical health in adolescence: a putative mechanistic neurodevelopmental pathway. JAMA Pediatr. 2017;171(12):1168–1175. doi:10.1001/jamapediatrics.2017.3009
- Oltean LE, Șoflău R, Miu AC, Szentágotai-Tătar A. Childhood adversity and impaired reward processing: a meta-analysis. Child Abuse Negl. 2023;142(Pt 1):105596. doi:10.1016/j.chiabu.2022.105596
- Kanner AD, Coyne JC, Schaefer C, Lazarus RS. Comparison of two modes of stress measurement: daily hassles and uplifts versus major life events. J Behav Med. 1981;4(1):1–39. doi:10.1007/bf00844845
- Ruffin CL. Stress and health—little hassles vs. major life events. J Austral Psychol. 1993;28(3):201–208.
- Monroe SM. Major and minor life events as predictors of psychological distress: further issues and findings. J Behav Med. 1983;6(2):189–205. doi:10.1007/bf00845380
- Desmond P, Cummins T, Ames D, Dennerstein L, Szoeke C. P2–270: the relationship between hassle severity, anxiety and cognitive performance: an 8-year follow-up in the women’s healthy aging project. Alzheimers Dement. 2013;9(4S_Part_11):P457–P457.
- Rickenbach EH, Almeida DM, Seeman TE, Lachman ME. Daily stress magnifies the association between cognitive decline and everyday memory problems: an integration of longitudinal and diary methods. Psychol Aging. 2014;29(4):852–862. doi:10.1037/a0038072
- Almulla AF, Algon AAA, Maes M. Adverse childhood experiences and recent negative events are associated with activated immune and growth factor pathways, the phenome of first episode major depression and suicidal behaviors. Psychiatry Res. 2024;334:115812. doi:10.1016/j.psychres.2024.115812
- Asselmann E, Wittchen HU, Lieb R, Beesdo-Baum K. A 10-year prospective-longitudinal study of daily hassles and incident psychopathology among adolescents and young adults: interactions with gender, perceived coping efficacy, and negative life events. Soc Psychiatry Psychiatric Epidemiol. 2017;52(11):1353–1362. doi:10.1007/s00127-017-1436-3
- Yan J, Kong T, He Y, McWhinnie CM, Yao S, Xiao J. Daily hassles and depression in individuals with cognitive vulnerability to depression: the mediating role of maladaptive cognitive emotion regulation strategies. Nordic Psychol. 2015;67(1):87–100. doi:10.1080/19012276.2014.957717
- Ji S, Wang H. A study of the relationship between adverse childhood experiences, life events, and executive function among college students in China. Psicol Reflex Crit. 2018;31(1):28. doi:10.1186/s41155-018-0107-y
- Maybery D. Incorporating interpersonal events within hassle measurement. Stress Health. 2003;19(2):97–110.
- Maes M, Almulla AF. Research and Diagnostic Algorithmic Rules (RADAR) and RADAR Plots for the First episode of major depressive disorder: effects of childhood and recent adverse experiences on suicidal behaviors. Neurocognition and Phenome Features Brain Sci. 2023;13(5). doi:10.3390/brainsci13050714
- Vasupanrajit A, Maes M, Jirakran K, Tunvirachaisakul C. Brooding and neuroticism are strongly interrelated manifestations of the phenome of depression. Frontiers in Psychiatry. 2023;14. doi:10.3389/fpsyt.2023.1249839
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56–62. doi:10.1136/jnnp.23.1.56
- Rungmueanporn L, Buathong N, Chandarasiri P, Wittayasai W. Development of the Adverse Childhood Experiences (ACE) questionnaire Thai version. Chula Me Bull. 2019;1(3):251–260.
- Boonyamalik P. Epidemiology of Adolescent Suicidal Ideation: Roles of Perceived Life Stress, Depressive Symptoms, and Substance Use. The Johns Hopkins University; 2005.
- Lotrakul M, Sukanich P, Sukying C. The reliability and validity of Thai version of Hamilton Rating Scale for Depression. J Psychiatr Assoc Thailand. 1996;41(4):235–246.
- Beck AT, Steer RA, Brown GJP. Beck depression inventory–II; 1996.
- Mungpanich A Development of the Thai version of the BDI-II depression assessment form at Khon Kaen Rajanagarindra hospital. 7th Annual International Mental Health Conference; Ambassador Hotel Bangkok; 2008.
- Spielberger CD State-Trait Anxiety Inventory for adults; 1983.
- Iamsupasit S, Phumivuthisarn P A study of cognitive factors related to anxiety sensitivity. Paper presented at: Proceedings of the East-West Psychology Science Research Center. Bangkok, Thailand; 2005.
- Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. doi:10.1093/sleep/34.5.601
- Mapi Language Services. Linguistic validation certificate paper version of the Insomnia Severity Index (ISI). Mapi Research Trust; 2015.
- Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. J Pers Soc Psychol. 1991;61(1):115–121. doi:10.1037//0022-3514.61.1.115
- Thanoi W, Panitrat R, Phancharoenworakul K, Thompson EA, Nityasuddhi D. The Adolescent ruminative response scale (Thai version): psychometric properties. J Nurs Sci J Thailand. 2011;29(3):19–38.
- Socha A, Cooper CA, McCord DM. Confirmatory factor analysis of the M5-50: an implementation of the International Personality Item Pool item set. Psychol Assess. 2010;22(1):43–49. doi:10.1037/a0017371
- Yomaboot P, Cooper A. Factor structure and psychometric properties of the International Personality Item Pool-NEO (IPIP-NEO) Thai version. J Somdet Chaopraya Instit Psychiatr. 2016;10(2):1.
- Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–1277. doi:10.1176/appi.ajp.2011.10111704
- The Columbia Lighthouse Project. Linguistic validation process. 2016; Available from: http://cssrs.wpengine.com/the-columbia-scale-c-ssrs/translations/. Accessed April 3, 2020.
- Epp AM, Dobson KS, Dozois DJ, Frewen PA. A systematic meta-analysis of the Stroop task in depression. Clin Psychol Rev. 2012;32(4):316–328. doi:10.1016/j.cpr.2012.02.005
- Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18(6):643.
- Ringle CM, Wende S, Becker J-M SmartPLS 3. Boenningstedt; 2015.
- Maes M, Moraes JB, Bonifacio KL, et al. Towards a new model and classification of mood disorders based on risk resilience, neuro-affective toxicity, staging, and phenome features using the nomothetic network psychiatry approach. Metab Brain Dis. 2021;36(3):509–521. doi:10.1007/s11011-020-00656-6
- Golden C, Freshwater SM, Golden Z Stroop color and word test; 1978.
- Hein TC, Muz B, Ahmadi-Montecalvo H, Smith T. Associations among ACEs, health behavior, and veteran health by service Era. Am J Health Behav. 2020;44(6):876–892. doi:10.5993/ajhb.44.6.11
- Peckins MK, Roberts AG, Hein TC, et al. Violence exposure and social deprivation is associated with cortisol reactivity in urban adolescents. Psychoneuroendocrinology. 2020;111:104426. doi:10.1016/j.psyneuen.2019.104426
- Gizdic A, Sheinbaum T, Kwapil TR, Barrantes-Vidal N. Empirically-derived dimensions of childhood adversity and cumulative risk: associations with measures of depression, anxiety, and psychosis-spectrum psychopathology. Eur J Psychotraumatol. 2023;14(2):2222614. doi:10.1080/20008066.2023.2222614
- Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9(11):e1001349. doi:10.1371/journal.pmed.1001349
- Giampetruzzi E, Tan AC, LoPilato A, et al. The impact of adverse childhood experiences on adult depression severity and treatment outcomes. J Affect Disord. 2023;333:233–239. doi:10.1016/j.jad.2023.04.071
- McLaughlin KA, Sheridan MA, Lambert HK. Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev. 2014;47:578–591. doi:10.1016/j.neubiorev.2014.10.012
- Sheridan MA, Shi F, Miller AB, Salhi C, McLaughlin KA. Network structure reveals clusters of associations between childhood adversities and development outcomes. Dev Sci. 2020;23(5):e12934. doi:10.1111/desc.12934
- Gonçalves SF, Chaplin TM, Turpyn CC, et al. Difficulties in emotion regulation predict depressive symptom trajectory from early to middle adolescence. Child Psychiatry Hum Dev. 2019;50(4):618–630. doi:10.1007/s10578-019-00867-8
- Ruan QN, Chen CM, Yang JS, Yan WJ, Huang ZX. Network analysis of emotion regulation and reactivity in adolescents: identifying central components and implications for anxiety and depression interventions. Front Psychiatry. 2023;14:1230807. doi:10.3389/fpsyt.2023.1230807
- Storrie CL, Kitissou K, Messina A. The effects of severe childhood physical and sexual abuse on adult socioeconomic prosperity. J Child Adolesc Trauma. 2023;16(1):55–68. doi:10.1007/s40653-022-00499-6
- Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: causal evidence and mechanisms. Science. 2020;370(6522). doi:10.1126/science.aay0214
- Kendall KM, Van Assche E, Andlauer TFM, et al. The genetic basis of major depression. Psychol Med. 2021;51(13):2217–2230. doi:10.1017/s0033291721000441
- Kendler KS, Ohlsson H, Sundquist J, Sundquist K, Edwards AC. The sources of parent-child transmission of risk for suicide attempt and deaths by suicide in Swedish national samples. Am J Psychiatry. 2020;177(10):928–935. doi:10.1176/appi.ajp.2020.20010017
- Coon H, Darlington TM, DiBlasi E, et al. Genome-wide significant regions in 43 Utah high-risk families implicate multiple genes involved in risk for completed suicide. Mol Psychiatry. 2020;25(11):3077–3090. doi:10.1038/s41380-018-0282-3
- Fergusson DM, McLeod GF, Horwood LJ. Childhood sexual abuse and adult developmental outcomes: findings from a 30-year longitudinal study in New Zealand. Child Abuse Negl. 2013;37(9):664–674. doi:10.1016/j.chiabu.2013.03.013
- Chen LP, Murad MH, Paras ML, et al. Sexual abuse and lifetime diagnosis of psychiatric disorders: systematic review and meta-analysis. Mayo Clin Proc. 2010;85(7):618–629. doi:10.4065/mcp.2009.0583
- Guiney H, Caspi A, Ambler A, et al. Childhood sexual abuse and pervasive problems across multiple life domains: findings from a five-decade study. Dev Psychopathol. 2022:1–17. doi:10.1017/s0954579422001146
- Schoedl AF, Costa MC, Mari JJ, et al. The clinical correlates of reported childhood sexual abuse: an association between age at trauma onset and severity of depression and PTSD in adults. J Child Sex Abus. 2010;19(2):156–170. doi:10.1080/10538711003615038
- Adams J, Mrug S, Knight DC. Characteristics of child physical and sexual abuse as predictors of psychopathology. Child Abuse Negl. 2018;86:167–177. doi:10.1016/j.chiabu.2018.09.019
- Sun J-W, Xue J-M, Bai H-Y, Zhang -H-H, Lin P-Z, Cao F-L. The association between negative life events, neuroticism and aggression in early adulthood. Pers Individ Dif. 2016;102:139–144. doi:10.1016/j.paid.2016.06.066
- Li Y, Gu S, Wang Z, et al. Relationship between stressful life events and sleep quality: rumination as a mediator and resilience as a moderator. Frontiers in Psychiatry. 2019:10. doi:10.3389/fpsyt.2019.00348
- Wang S, Jing H, Chen L, Li Y. The influence of negative life events on suicidal ideation in college students: the role of rumination. Int J Environ Res Public Health. 2020;17(8). doi:10.3390/ijerph17082646
- Ren Z, Zhang X, Shen Y, et al. Associations of negative life events and coping styles with sleep quality among Chinese adolescents: a cross-sectional study. Environ Health Prev Med. 2021;26(1):85. doi:10.1186/s12199-021-01007-2
- Ji L, Chen C, Hou B, et al. A study of negative life events driven depressive symptoms and academic engagement in Chinese college students. Sci Rep. 2021;11(1):17160. doi:10.1038/s41598-021-96768-9
- Supasitthumrong T, Maes M, Tunvirachaisakul C, et al. Predictors of increased affective symptoms and suicidal ideation during the COVID-19 pandemic: results from a large-scale study of 14,271 Thai adults; 2023.
- Scarpina F, Tagini S. The stroop color and word test. Front Psychol. 2017;8:557. doi:10.3389/fpsyg.2017.00557
- Unsworth N. Interference control, working memory capacity, and cognitive abilities: a latent variable analysis. Intelligence. 2010;38(2):255–267. doi:10.1016/j.intell.2009.12.003
- Naglieri JA, Goldstein SJH. Using the Comprehensive Executive Function Inventory (CEFI) to assess executive function: from theory to application; 2013:223–244.
- Tjoelker FM, Jeuring HW, Aprahamian I, et al. The impact of a history of child abuse on cognitive performance: a cross-sectional study in older patients with a depressive, anxiety, or somatic symptom disorder. BMC Geriatr. 2022;22(1):377. doi:10.1186/s12877-022-03068-6
- Lund JI, Toombs E, Radford A, Boles K, Mushquash C. Adverse Childhood experiences and executive function difficulties in children: a systematic review. Child Abuse Negl. 2020;106:104485. doi:10.1016/j.chiabu.2020.104485
- Saleh A, Potter GG, McQuoid DR, et al. Effects of early life stress on depression, cognitive performance and brain morphology. Psychol Med. 2017;47(1):171–181. doi:10.1017/s0033291716002403
- Gould F, Clarke J, Heim C, Harvey PD, Majer M, Nemeroff CB. The effects of child abuse and neglect on cognitive functioning in adulthood. J Psychiatr Res. 2012;46(4):500–506. doi:10.1016/j.jpsychires.2012.01.005
- Sheffler JL, Piazza JR, Quinn JM, Sachs-Ericsson NJ, Stanley IH. Adverse childhood experiences and coping strategies: identifying pathways to resiliency in adulthood. Anxiety Stress Coping. 2019;32(5):594–609. doi:10.1080/10615806.2019.1638699
- Barrera M, Calderón L, Bell V. The cognitive impact of sexual abuse and PTSD in children: a neuropsychological study. J Child Sex Abus. 2013;22(6):625–638. doi:10.1080/10538712.2013.811141
- Hawkins MAW, Layman HM, Ganson KT, et al. Adverse childhood events and cognitive function among young adults: prospective results from the national longitudinal study of adolescent to adult health. Child Abuse Negl. 2021;115:105008. doi:10.1016/j.chiabu.2021.105008
- Maes M, Rachayon M, Jirakran K, et al. Adverse childhood experiences predict the phenome of affective disorders and these effects are mediated by staging, neuroimmunotoxic and growth factor profiles. Cells. 2022;11(9). doi:10.3390/cells11091564
- Maes M, Congio A, Moraes JB, et al. Early life trauma predicts affective phenomenology and the effects are partly mediated by staging coupled with lowered lipid-associated antioxidant defences. Biomol Concepts. 2018;9(1):115–130. doi:10.1515/bmc-2018-0010
- Horn SR, Leve LD, Levitt P, Fisher PA. Childhood adversity, mental health, and oxidative stress: a pilot study. PLoS One. 2019;14(4):e0215085. doi:10.1371/journal.pone.0215085
- Moraes JB, Maes M, Roomruangwong C, et al. In major affective disorders, early life trauma predict increased nitro-oxidative stress, lipid peroxidation and protein oxidation and recurrence of major affective disorders, suicidal behaviors and a lowered quality of life. Metab Brain Dis. 2018;33(4):1081–1096. doi:10.1007/s11011-018-0209-3
- Blaisdell KN, Imhof AM, Fisher PA. Early adversity, child neglect, and stress neurobiology: from observations of impact to empirical evaluations of mechanisms. Int J Dev Neurosci. 2019;78:139–146. doi:10.1016/j.ijdevneu.2019.06.008
- Tinajero R, Williams PG, Cribbet MR, et al. Reported history of childhood trauma and stress-related vulnerability: associations with emotion regulation, executive functioning, daily hassles and pre-sleep arousal. Stress Health. 2020;36(4):405–418. doi:10.1002/smi.2938
- Chen XY, Lo CKM, Chan KL, Leung WC, Ip P. Association between childhood exposure to family violence and telomere length: a meta-analysis. Int J Environ Res Public Health. 2022;19(19). doi:10.3390/ijerph191912151
- Everson TM, Kaczor K, Makoroff K, et al. Epigenetic differences in stress response gene FKBP5 among children with abusive vs accidental injuries. Pediatr Res. 2023;94(1):193–199. doi:10.1038/s41390-022-02441-w
- Maes M, Zhou B, Jirakran K, et al. Towards a major methodological shift in depression research by assessing continuous scores of recurrence of illness, lifetime and current suicidal behaviors and phenome features. J Affect Disord. 2024;350:728–740. doi:10.1016/j.jad.2024.01.150
- Walsh ND, Dalgleish T, Lombardo MV, et al. General and specific effects of early-life psychosocial adversities on adolescent grey matter volume. Neuroimage Clin. 2014;4:308–318. doi:10.1016/j.nicl.2014.01.001
- Oshri A, Gray JC, Owens MM, et al. Adverse Childhood experiences and amygdalar reduction: high-resolution segmentation reveals associations with subnuclei and psychiatric outcomes. Child Maltreat. 2019;24(4):400–410. doi:10.1177/1077559519839491
- Koyama Y, Fujiwara T, Murayama H, Machida M, Inoue S, Shobugawa Y. Association between adverse childhood experiences and brain volumes among Japanese community-dwelling older people: findings from the NEIGE study. Child Abuse Negl. 2022;124:105456. doi:10.1016/j.chiabu.2021.105456
- Lo Iacono L, Trentini C, Carola V. Psychobiological consequences of childhood sexual abuse: current knowledge and clinical implications. Front Neurosci. 2021;15:771511. doi:10.3389/fnins.2021.771511
- Blanco L, Nydegger LA, Camarillo G, Trinidad DR, Schramm E, Ames SL. Neurological changes in brain structure and functions among individuals with a history of childhood sexual abuse: a review. Neurosci Biobehav Rev. 2015;57:63–69. doi:10.1016/j.neubiorev.2015.07.013
- van West D, Maes M. Activation of the inflammatory response system: a new look at the etiopathogenesis of major depression. Neuro Endocrinol Lett. 1999;20(1–2):4.
- Maes M, Van Bockstaele DR, Gastel A, et al. The effects of psychological stress on leukocyte subset distribution in humans: evidence of immune activation. Neuropsychobiology. 1999;39(1):1–9. doi:10.1159/000026552
- Maes M, Galecki P, Chang YS, Berk M. A review on the oxidative and nitrosative stress (O&NS) pathways in major depression and their possible contribution to the (neuro)degenerative processes in that illness. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35(3):676–692. doi:10.1016/j.pnpbp.2010.05.004
- Chubar V, Vaessen T, Noortgate WVD, et al. Mild daily stress, in interaction with NR3C1 DNA methylation levels, is linked to alterations in the HPA axis and ANS response to acute stress in early adolescents. Psychoneuroendocrinology. 2023;150:106045. doi:10.1016/j.psyneuen.2023.106045
- Reuben A, Moffitt TE, Caspi A, et al. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J Child Psychol Psychiatr. 2016;57(10):1103–1112. doi:10.1111/jcpp.12621