Abstract
Patients with thin, low-risk melanomas have an excellent long-term prognosis and higher quality of life than those who are diagnosed at later stages. From an economic standpoint, treatment of early stage melanoma consumes a fraction of the health care resources needed to treat advanced disease. Consequently, early diagnosis of melanoma is in the best interest of patients, payers, and health care systems. This review describes strategies to ensure that patients receive an early diagnosis through interventions ranging from better utilization of primary care clinics, to in vivo diagnostic technologies, to new “apps” available in the market. Strategies for screening those at high risk due to age, male sex, skin type, nevi, genetic mutations, or family history are discussed. Despite progress in identifying those at high risk for melanoma, there remains a lack of general consensus worldwide for best screening practices. Strategies to ensure early diagnosis of recurrent disease in those with a prior melanoma diagnosis are also reviewed. Variations in recurrence surveillance practices by type of provider and country are featured, with evidence demonstrating that various imaging studies, including ultrasound, computed tomography, positron emission tomography, and magnetic resonance imaging, provide only minimal gains in life expectancy, even for those with more advanced (stage III) disease. Because the majority of melanomas are attributable to ultraviolet radiation in the form of sunlight, primary prevention strategies, including sunscreen use and behavioral interventions, are reviewed. Recent international government regulation of tanning beds is described, as well as issues surrounding the continued use artificial ultraviolet sources among youth. Health care stakeholder strategies to minimize UV exposure are summarized. The recommendations encompass both specific behaviors and broad intervention targets (eg, individuals, social spheres, organizations, celebrities, governments).
Introduction
In 2015, an estimated 73,870 US citizens will learn they have invasive melanoma, and an additional 63,440 people will receive a diagnosis of melanoma in situ.Citation1 Early detection remains the most important predictor of melanoma survival. If treatment outcomes and overall survival (OS) are to improve, current practices must be evaluated to ensure effective diagnosis and treatment.
For more than 150 years, surgical excision of early melanoma has proven curative for many patients. This widely accepted fact likely was first detailed in 1840 by Dr Samuel Cooper, a British surgeon, in his book The First Lines of the Theory and Practice of Surgery.Citation2 Pathologic disease stage, dictated by primary tumor characteristics like Breslow thickness and ulceration and regional nodal and metastatic disease status, has repeatedly been shown to predict outcome.Citation3–Citation5 Considering the excellent outcomes experienced by patients with thin, low-risk melanomas, education, awareness, and skin screening represent the earliest opportunities for diagnosis.
For patients with melanoma in situ (stage 0) and a low-risk subset of stage IA melanoma (≤0.75 mm Breslow thickness, without ulceration or mitotic figures), the treatment is wide local excision alone. For patients with higher risk primary tumors (>0.75–1 mm Breslow thickness), sentinel lymph node biopsy provides pathologic staging of regional lymph node basins. Complete lymph node dissection, adjuvant systemic therapy, and radiation are considered for those with more advanced stages of disease.Citation6 Lymph node dissections are not infrequently associated with complications including infection, wound separation, seroma, and chronic lymphedema.Citation7–Citation9 Likewise, systemic therapy, which may include chemotherapy, BRAF inhibitors, and/or immunotherapy, introduces potential toxicity.Citation6,Citation10–Citation14
Quality-of-life considerations
Early diagnosis is associated with improved quality of life for patients with melanoma. A Belgian study of 395 melanoma patients evaluated with the EQ-5D-5L questionnaire reported that postoperative stage I–II patients experienced better health-related quality of life >2 years after treatment than postoperative patients with stage III melanoma at least 4 months after treatment.Citation15 Similarly, in a German study of 664 melanoma patients evaluated with the EORTC-QLQ-C30 questionnaire at least 2 years following cancer treatment, patients with regional nodal disease had worse global quality of life (odds ratio [OR] 3.34, 95% confidence interval [CI] 1.4–8.0) than patients with no nodal disease.Citation16 Because those with stage III disease generally undergo therapeutic lymph node dissection and possible adjuvant pharmacologic therapy, the stage-appropriate treatments likely contribute to worsened quality of life. Adjuvant low-dose interferon-alpha (IFN-α) treatment has been associated with clinically meaningful, significantly worse scores for health-related quality of life in patients with stage II and III disease compared to those who did not receive (IFN-α) treatment.Citation13,Citation14
Cost savings from early diagnosis
Although cost generally is a secondary consideration in cancer treatment, early diagnosis may provide cost savings. The estimated US direct medical cost for prevalent melanoma in 2004 was $291 million (US dollars).Citation17 When indirect medical costs such as patient time, lost wages, and lost future earning potential attributable to early death are also taken into consideration, the estimated annual cost ballooned to $3.1 billion US dollars in 2004.Citation17 Morris et al conducted a study of annual melanoma costs in the United Kingdom. Direct medical costs were estimated at £24 million in 2002 UK pounds (or $36 million in 2002 US dollars), and direct plus indirect costs totaled £138 million 2002 UK pounds ($207 million in 2002 US dollars).Citation18 These numbers are consistent with the USA’s roughly doubled health expenditure per capita versus UK expenses during the early 2000s.Citation19 Despite the spending inequalities resulting from differences in health care delivery systems, few would dispute the significance of total melanoma costs to patients, families, and the health care systems.
Numerous studies demonstrate that increased melanoma treatment costs correspond to the disease stage.Citation20–Citation26 Alexandrescu calculated total health care costs by stage for up to 5 years following diagnosis of melanoma; costs increased from $4,648 2008 US dollars for in situ disease up to $159,808 2008 US dollars for stage IV disease.Citation20 He concluded that costs significantly decreased with early stage diagnosis. In another study, among patients with stage III melanoma who received high-dose IFN-α therapy versus patients with stage III disease who were observed postoperatively, the estimated cost for high-dose interferon treatment per quality-adjusted life year was $85,779 in 2005 US dollars.Citation27 Therefore, exponential savings can likely be realized if melanoma is diagnosed early.
The cost effectiveness of melanoma screening depends greatly upon the population being screened and the method used. Losina et al used a Markov model to predict the cost-effectiveness ratios per quality-adjusted life year (QALY) for visual melanoma screening in different populations.Citation28 Annual screening in the general population over 50 was not deemed cost effective ($586,800/QALY in 2004 US dollars), but screening higher risk populations was cost effective, such as screening siblings of melanoma patients every 2 years ($35,500/QALY) or a one-time screening in those over 50 years of age ($10,100/QALY). A recent systematic review of the topic also concluded that early detection of melanoma targeting high-risk populations may be cost effective, but updated studies are necessary.Citation29
Initial diagnosis of melanoma
Secondary prevention, ie, diagnosing disease as early as possible to limit morbidity and mortality, is critical for improved outcomes, quality, and cost. Johnson et alCitation30 proposed three secondary prevention strategies that may be utilized by primary care physicians (PCPs). First, they may provide verbal guidance and written pamphlets on skin cancer identification and self-skin examination; second, PCPs may identify patients at highest risk based on family history, personal phenotype, or high-risk behaviors and refer to a dermatologist for screening; the third and most time-intensive strategy recommended by these authors is to train PCPs to conduct thorough skin examinations for all patients during routine office visits. The authors examined medical training, physician workload, and career expectation gaps and identified that these strategies are viable but necessitate further study before wide-scale implementation. The shortage of general practitioners in the USA is expected to worsen as the population ages;Citation31 consequently, it is critical to identify cost-effective strategies to facilitate skin exams and early melanoma diagnosis.
Dermatologists may utilize more directed technologies to enhance early detection and minimize unnecessary diagnostic excisions. An in-depth review of these technologies is beyond the scope of this article, but in brief includes dermoscopy, reflectance confocal microscopy (an imaging technology that renders real-time images with near histologic-level resolution), automated dermoscopic analysis (MelaFind is one such technology that is FDA approved), and tape-stripping RNA analysis. Total body photography may also be utilized to obtain a baseline set of clinical images to which subsequent clinical examinations may be compared. Although some nonmalignant nevi may demonstrate interval change, nonchanging lesions are almost certainly benign and do not need to be removed. Comparison may also facilitate detection of subtle, early stage melanomas.
Outside of clinic-based primary prevention of melanoma, other resources may facilitate care and prevention for patients lacking intensive screening program access or awareness of their risk profile.Citation32,Citation33 A review of smartphone applications dedicated to evaluating melanoma revealed that 39 health applications (apps) were available as of July 2014.Citation34 Of these, 22 provide patient education on clinical features of melanoma, sun-protective practices, and outline appropriate techniques for self-skin examination. Nineteen apps allowed users to upload pictures of nevi and follow them over time. Nine of the apps allowed users to ask an “expert” to review an image, usually at additional cost. The authors did not contend that these apps were validated for widespread use, and many required additional evaluations before being widely marketable. Despite these limitations, the new technology has the potential to empower patients to identify melanoma at a time when it is more easily treated.
Screening and diagnosis for high-risk populations
Melanoma is associated with a well-defined set of risk factors, which include advancing age, male sex, lighter skin pigmentation, a history of intermittent intense sunlight exposure, a history of indoor tanning bed exposure, a personal history of dysplastic nevi or prior melanoma, or a strong family history of melanoma.Citation35 Identification of high-risk melanoma patients facilitates improved outcomes when education and surveillance guidelines are appropriately tailored.
Age and sex
Age has long been a known risk factor for melanoma, with studies reporting an increase in melanoma risk of 3.1% per year, and investigators have postulated that DNA damage accumulates over time.Citation36 There is no direct correlation between age, metastasis, and mortality, however. Balch et alCitation37 reported that in a series of 7,756 melanoma subjects from the American Joint Committee on Cancer database, younger patients demonstrated a higher rate of sentinel lymph node metastasis than their older counterparts, and subjects >70 years of age demonstrated a lower rate of regional disease but a more aggressive primary tumor, leading to a higher mortality rate.Citation37 In a series using 2014 National Cancer Registry data, a 2.9% risk for invasive melanoma among men was identified, with a reduced risk of 1.9% for melanoma in women.Citation38 Thus, as a group, older men are considered at higher risk as compared to other age and sex groups.
Skin type and nevi
Phenotypes with lower pigmentary density, such as red or blond hair, lightly colored skin with multiple freckles, and blue or hazel eyes, also have been associated with an increased risk of melanoma.Citation39 Overall, nevi are not considered premalignant lesions. Melanoma may arise from any nevus (typical or dysplastic) or normal skin. While the authors advocate for surveillance of both new and changing nevi,Citation40 specific surveillance recommendations vary by country, professional organization, and the presence of other known risk factors.
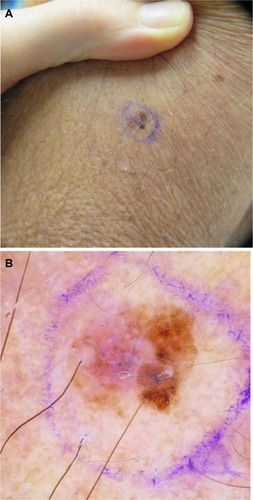
Dermoscopy, the examination of skin using skin surface microscopy, has become an important tool in the evaluation of patients at high risk with multiple nevi. A representative clinical and dermoscopic image from a stage IA melanoma demonstrates the increased detail visible with dermoscopic examination (). A randomized trial by Carli et al reported a reduction in the number of patients referred for biopsy (9% vs 15%) and a decrease in the benign-to- malignant excision ratio from 18:1 to 4:1 following the introduction of dermoscopy into clinical practice.Citation41 Watts et al reported in a systematic review published in 2015 that dermoscopy was particularly useful for patients with dysplastic nevi.Citation42 Widespread adoption of dermoscopy in the USA has been hampered by the need for dedicated provider training and, potentially, by the absence of provider reimbursement.
Figure 1 (A) Clinical image of a pink and brown macule of the left upper arm, diagnosed as a stage IA superficial spreading melanoma, with Breslow depth of 0.28 mm. (B) Dermoscopy demonstrates a globally asymmetrical lesion, with a disorganized reticular network on the right and a milky/pink homogenous area on the left.
Family history and genetic predisposition
After a patient receives an initial melanoma diagnosis, his or her personal risk for a second primary melanoma is 3–8 times higher than that of the unaffected population.Citation35 A recent meta-analysis identified eight genomic loci specifi-cally associated with varying levels of statistically significant (P>0.05) increases in melanoma risk: MC1R, TYR, TYRP1, SLC45A2, ASIP/PIGU/MYH7B, and CDKN2A/MTAP.Citation43 The investigators noted there may be two different genetic drivers for melanoma development: those involved in pigmentation change and those involved in nevi development.Citation43 Numerous studies continue to shed light on the genetic components of melanoma and define them as potential targets for treatment. Screening for patients who are genetically predisposed to melanoma may include frequent clinical exams, referral to a specialist, dermoscopy by a trained professional, total-body photography, and/or sequential digital imaging over time (). Genetic testing is generally recommended only for those with a strong family history, although the level of evidence for this recommendation is weak.Citation42
Table 1 Summary of recommended screening practices that may be considered for specific high-risk populations
Familial atypical multiple mole melanoma syndrome, another high-risk variant, is associated with multiple atypical dysplastic nevi (often exceeding 50) and is an autosomal-dominant disorder associated with a defect in the CDKN2A gene.Citation44 Certain dermatology guidelines recommend digital dermoscopy every 3 months for patients with this syndrome.Citation45
Comparison of guidelines
Despite the many ongoing studies on self-examination, physical exam, dermoscopy, and new photographic techniques, there is a lack of evidence-based guidelines and no real consensus regarding surveillance practices for high-risk patients prior to melanoma diagnosis. The most recent National Comprehensive Cancer Network guidelines contained no specific recommendations for screening high-risk populations for primary cutaneous melanoma,Citation6 and the American Academy of Dermatology in 2010 recommended that clinicians evaluate patients at least annually and perhaps as often as every 3 months.Citation46 A 2015 systematic review summarized 34 sets of surveillance guidelines from 20 countries and reported large variation in recommendations for surveillance technologies and exam intervals, ranging from 3 months to 12 months for patients at high risk, as summarized in .Citation42,Citation47–Citation52
In 2014, Watts et alCitation53 completed a cost analysis of dermatological surveillance for individuals deemed high risk for melanoma who received a full skin examination enhanced by dermoscopy every 6 months. If a lesion was deemed concerning for malignancy, it was excised, and the patient returned after 3 months for additional screening. A total of 102 patients were screened in this manner, with a mean annual cost per patient to the health system of $882 in 2013 Australian dollars ($599 in 2013 US dollars). Three early stage melanomas and eight non-melanoma skin cancers were diagnosed at a sufficiently early stage to warrant therapeutic excision with local anesthetic. The authors note that although the sample size was small, the study supported the cost effectiveness of intensive screening for those at highest risk of cutaneous malignancy.Citation53
Controversy remains regarding the value of self-examination. While only 23%–61% of the general population worldwide engages in skin self-examinationCitation54 and only 24.1% of patients at high-risk perform an optimal self-exam defined as a monthly exam covering at least 80% of the body surface,Citation55 the National Cancer Institute conducted a population-based case–control study of 1,199 patients that suggested a possible decrease in mortality by as much as 63% for patients who practiced self-examination.Citation56 Shortly thereafter, the US Preventive Services Task Force (USPSTF) stated that evidence demonstrating improved outcomes resulting from self-examination was still lacking.Citation57 Azoury and Lange stated in Surgical Clinics of North America that “prevention and early detection programs lack a uniform approach worldwide, and targeting high-risk groups remains a challenge”.Citation58
Diagnosis of melanoma recurrence
Once a diagnosis of melanoma has been confirmed and treatment is completed, it is important to continue surveillance for both tumor recurrence and additional primary melanomas – both of which pose ongoing risk.
Current practices
In 2012, Cromwell et alCitation59 completed a systematic review to evaluate worldwide melanoma surveillance practices. Peer-reviewed literature from three medical indices was examined, and all articles that had an English translation were reviewed. A total of 43 articles were identified that discussed melanoma surveillance practices in Australia/New Zealand, Canada, Germany, the UK, the USA, the Netherlands, and Switzerland. An evaluation of surveillance practices by country identified several different practices. Among patients treated for stage I melanoma, the frequency of skin examinations ranged from one to six visits per year during the first 5 years after diagnosis, and, in certain instances, included an ultrasound of the regional nodal basin, chest X-ray, or photography. The highest intensity screening was observed in the UK. Patients with a history of stage II disease were screened at similar frequencies worldwide; however, imaging recommendations also included a computed tomography (CT) scan of the chest, abdomen, and pelvis in Germany and in the USA. For patients with stage III melanoma, surveillance was recommended two to four times per year, often including various imaging modalities and brain imaging. The findings of this systematic review are summarized in .
Table 2 Stage-specific surveillance guidelines by country during disease years 1–5
In the same systematic review,Citation59 surveillance strategies were identified and stratified by type of health care provider (eg, general practitioner, dermatologist, medical oncologist, or surgical oncologist), as shown in . Among these practices, the only universal recommendation was for patient self-examination of skin and nodal basins. General practitioners saw patients with all stages of disease four times per year but generally did not obtain surveillance imaging. Dermatologists, medical oncologists, and surgical oncologists all exercised more intensive surveillance both in terms of the number of examinations and types of imaging obtained, which increased progressively with stage.
Table 3 Stage-specific surveillance guidelines by physician specialty during disease years 1–5
Surveillance imaging
Imaging is a widely used tool to detect recurrence. Imaging of the regional nodal basins can be accomplished in patients with melanoma with ultrasonography, which is thought to be most sensitive, or with CT with or without positron emission tomography (PET) or magnetic resonance imaging (MRI) to evaluate for distant metastatic disease.Citation60 Highly utilized, nonsymptom-driven imaging may only identify late recurrences that may not be amenable to localized treatment. Risks associated with frequent imaging without a clinical indication include false-positive findings, which often necessitate additional testing such as biopsies and increase patient anxiety and cost. Additionally, radiation exposure poses risk for cumulative toxicity and second primary malignancies.Citation61
A meta-analysis conducted by Xing et al evaluated the use of ultrasound, CT, PET, and PET/CT for staging and surveillance of patients with melanoma.Citation62 In this analysis, a literature search identified 74 unique citations that reported patient-level data for 10,528 patients undergoing imaging for the staging or surveillance of melanoma. A Bayesian bivariate binomial model was developed to estimate the sensitivity and specificity of each test. For the primary staging of regional lymph nodes, ultrasound was the most sensitive technique (60% median score, 95% CI 33%–83%), followed by PET (30% median score, 95% CI 12%–55%), PET/CT (11% median score, 95% CI 1%–50%) and CT (9% median score, 95% CI 12%–55%). For patients with melanoma who were undergoing lymph node surveillance, the study found that ultrasound was again the most sensitive technique (96% median score, 95% CI 85%–99%). PET/CT was the most sensitive modality for both staging and surveillance of distant metastases (80% median score, 95% CI 53%–93% for staging; 86% median score, 95% CI 76%–93% for surveillance).
Subsequent analyses from a single institution have been completed using patient-level data from 1,600 patients treated for stages I–III melanoma between 1992 and 2007 using a probabilistic Markov model to evaluate the impact of routine surveillance for the detection of melanoma recurrence at a time at which it can be surgically treated.Citation63 To evaluate the impact of imaging, the model assumed that 80% of regionally detected recurrences and 20% of distant recurrences identified by routine imaging could be treated surgically. Using an interval of 6 months or 12 months for surveillance strategies, the model used CT and PET/CT to evaluate the impact of early detection on survival. For patients with stage I disease, CT imaging at 12-month intervals over 5 years detected treatable regional or distant recurrence in only 1.3% more patients than physical exam alone.Citation63 Patients with stage IIIC disease would theoretically experience the best survival advantage with frequent surveillance imaging, but the increase in life expectancy was only 2.0 months in this subgroup when PET/CT was obtained every 6 months.Citation63 The study concluded that the detection of surgically treatable recurrences with imaging provides only very minimal gains in life expectancy while greatly increasing cost and resource utilization.
The survival benefit associated with early detection of melanoma recurrence was evaluated by Leiter et al.Citation64 In this long-term survival analysis, 1,696 patients with stages I–III cutaneous melanoma were prospectively surveyed from 1996 to 1998 to evaluate the impact of lead-time bias on the diagnosis of metastatic disease. Surveillance included a combination of physical exam, ultrasound of nodal basins, abdominal ultrasound, chest X-ray, and blood draws measuring alkaline phosphatase and lactate dehydrogenase. Most tests were performed annually for patients with stages I–II disease and biannually for those with stage III disease. CT, MRI, PET scans, or other imaging techniques were used only if findings were inconclusive on the initial tests. In this cohort, 112 patients developed recurrence, and 52.7% of these recurrences were detected at an early stage. Among patients with early recurrence, 64.4% died as a result of melanoma, whereas 86% of those detected at a late stage died. Results showed a statistically significant survival benefit among patients whose metastases were detected early (40.5% OS) rather than late (25.6% OS, P=0.013). However, when stratified by locoregional or distant metastases, differences in OS were not statistically significant between early and late detection.
Advances in immunotherapy and targeted therapies have ushered in a new era in treating advanced and metastatic melanoma. Presently, six drugs have been approved for this use in the USA, Europe, and/or Japan (ipilimumab, nivolumab, pembrolizumab, vemurafenib, dabrafenib, and trametinib).Citation65 Early diagnosis of recurrent or metastatic disease may lead to improved survival by optimizing early initiation of the above new therapies. Trials are going on to determine optimal timing and combination of treatments to produce maximum benefit.
Primary prevention of melanoma
Primary prevention is designed to inhibit UV radiation-induced malignant cellular transformation by increasing sun-protective behaviors and reducing indoor tanning at individual and population levels. Sun protection and indoor tanning have been recent targets by governmental regulation and behavior modification efforts.
Increasing sun-protective behaviors
The percentage of melanomas attributable to sunlight exposure ranges between 68% and 97%.Citation66 As a result, limiting UV radiation by changing behaviors and attitudes regarding sun exposure has the potential to eliminate the majority of malignant melanoma cases worldwide. The spectrum of concerning UV radiation includes UVA (320–400 nm) and UVB (290–320 nm) rays, which induce mutagenic and immunomodulatory effects.Citation67 UVB is the main culprit behind DNA damage; however, UVA comprises 90%–95% of the UV spectrum that comes into contact with epithelial cells.Citation67 Gandini et al demonstrated that intermittent sun exposure and sunburn history are more strongly associated with melanoma, whereas a high level of continuous exposure is protective against melanoma.Citation39 Thus, the manner of exposure – not solely the exposure itself – is associated with increased risk.
Governments have become involved in sun exposure by endorsing sun-protective behaviors and by regulating the sale of sunscreen products. In the last 10 years, Europe, Australia, and North America have introduced tighter legislation on sunscreen and increasingly emphasized sunscreens that are “broad spectrum” (or protect against both UVA and UVB radiation) as the only sunscreens that can reduce cancer risk.Citation68–Citation71
Critics say insufficient evidence demonstrates that sunscreen use reduces melanoma incidence, citing poor internal validity and inconsistency in reported studies.Citation72,Citation73 The largest randomized adult study to test the sunscreen hypothesis was performed by Green et al as part of the Nambour Skin Cancer Prevention Trial.Citation74 More than 1,600 patients were followed for nearly 15 years after randomization to daily application of sun protection factor (SPF) 16 sunscreen vs a comparison group that continued their usual, pretrial sunscreen application practices. While the results were of borderline statistical significance, eleven patients developed first primary melanomas (eight in situ, three invasive) in the daily sunscreen group compared to 22 patients (eleven in situ, eleven invasive) in the control group (hazard ratio [HR] 0.50, 95% CI 0.24–1.02, P=0.51).
Major skin cancer organizations, including the American Cancer Society, Cancer Council Australia, and the World Health Organization (WHO), do recommend sunscreen use to prevent skin cancer. The American Academy of Dermatology recommends everyone use broad-spectrum, water-resistant SPF 30 or higher sunscreen whenever outdoors. All areas not covered by clothing should be generously coated 15 minutes before exposure, and reapplication should occur every 2 hours and after swimming or sweating heavily; SPF 30 or higher lip balm also should be worn to protect the lips.Citation75 Sunscreen use should be combined with other sun-protective behaviors such as limiting midday exposure, covering exposed skin with clothing, seeking shade, and monitoring the UV index.Citation75–Citation78
Children are particularly vulnerable to sun exposure, and children who sustain sunburns are at highest risk for developing melanoma among all age groups (OR 1.91, 95% CI 1.59–2.30) in one meta-analysis.Citation79 To this end, the WHO recommends teaching sun protection in schools and has developed its own curriculum, as have nations in Europe, North America, and Australia.Citation80 The SunWise Program created by the US Environmental Protection Agency has been used in more than 40,000 schools and organizations since 2000Citation81 and is estimated to save $2–$4 in health care and productivity losses for every dollar spent.Citation82 Unfortunately, governmental oversight of sunscreen by the FDA has had the unintended effect of limiting sunscreen use in US schools; in many areas, a physician’s note or prescription is now required to bring sunscreen to school.
Employees with occupation-related sun exposure with three or more hours of sun exposure per workday represent another group at risk for melanoma.Citation83 The SUNWISE Letter Carriers Study, an intervention involving 70 postal stations and more than 2,000 postal workers in Southern Califor-nia, randomized workers to receive educational sun safety messages and access to protective hats and sunscreen. The intervention also included visual cues as behavior prompts, placement of large pump bottles of sunscreen in locker rooms, and the distribution of sunscreen to each worker. At 2 years, those in the intervention group demonstrated significantly higher rates of sunscreen use (OR 2.0, 95% CI 1.6–2.6) and hat use (OR 2.9, 95% CI 2.3–3.6) versus controls.Citation84 While workplace interventions require extra planning, time, and money to implement, they can influence individual practices, especially with a supportive workplace culture.Citation83
Clinicians play an important role in counseling patients about sun-protective behaviors. Less than half of patients report receiving counseling about sun protection,Citation85–Citation87 but multiple studies have shown that when counseling is delivered, it is associated with the performance of sun-protective behav-iors, especially sunscreen use.Citation85,Citation87,Citation88 The USPSTF recommends counseling children, adolescents, and fair-skinned young adults younger than age 24 to limit UV radiation exposure by performing many of the behaviors listed in the left side of . However, the USPSTF concludes there is insufficient evidence of the risks versus benefits of counseling those older than 24 years of age about minimizing risk of skin cancer.Citation89
Table 4 Health care stakeholder recommendations and strategies to reduce UV radiation exposure
The right side of summarizes targets for dissemination of skin safety information. Depending on the age and demographics of the target group (young, old, male, female, urban, rural, etc) tailored messages can be created and directed at multiple target levels for maximal effect on behavior. For example, occupationally-exposed adults may be reached by influencing the workplace (target organizations), influencing individual workers’ practices (target the Individual), and influencing governmental regulations regarding workplace sun exposure (partner with government and nonprofit organizations). Or, if trying to change adolescent behaviors, leveraging parents and peers (target the individual’s social sphere), celebrity influence (employ mass media, celebrities, and public figures), and government regulations may be the solution. The goal with all dissemination strategies is to create campaigns that target the group of interest on multiple levels to create maximum behavior change.
Reducing indoor tanning
The dangers of UV exposure posed by tanning beds and devices have prompted health leaders and governments to intervene and limit the use of such products. In 2009, WHO reclassified UV tanning devices as a human carcinogen,Citation90 citing a systematic review of seven studies demonstrating tanning bed exposure before age 35 was associated with relative risk of 1.75 (95% CI 1.35–2.26) for melanoma.Citation91
Within the past year, the FDA reclassified UV lamps from class I (general controls) to class II devices (special controls), thus increasing regulation and issued a “black box warning” requiring device labeling that people younger than age 18 should not use sunlamp products.Citation92 However, this reclassifi-cation carried no effective limitation at the point of service, which has been left to the discretion of individual states. In the USA, 23 of 50 states have enacted indoor tanning bans for minors, but laws among states are heterogeneous. Certain states prohibit indoor tanning for those 14 and younger, and other states extend the ban to teenagers 15 years, 16 years, or 17 years of age.Citation93 Enforcement of existing laws is sporadic, with underage tanners purchasing indoor tanning sessions from 81% of approached facilities in one study.Citation94 Several member countries in the European Union also have bans for minors,Citation95 and two countries have banned indoor tanning for all ages, Brazil in 2011Citation95 and Australia in 2015.Citation96
Multiple interventions may be needed to simultaneously target individual and societal beliefs about the attractiveness of a tanned appearance in conjunction with educating parents, launching school-based programs, and leveraging celebrity influence. outlines the different target levels to be considered when created educational campaigns to combat indoor tanning. Continual assessment and evaluation of outcomes would inform progress of programs and help dictate future programming directions.Citation97
Summary
Early diagnosis of melanoma provides opportunities for improved patient survival, better quality of life, and additional cost savings for health care systems. Primary prevention techniques include physician counseling and skin-protection behaviors that reduce UV exposure. Governments play a role by introducing policies that encourage and promote skin protection, such as sunscreen regulation and bans on tanning devices, especially for minors. Secondary prevention strategies can be used by PCPs or dermatologists and may be supported by technology such as dermoscopy and total-body photography.
There is a general lack of worldwide consensus on optimal screening of high-risk patients. Frequent skin self-exams, physical exams, dermoscopy, and a low intervention threshold are the mainstays of early detection, but recommended intervals for clinical encounters range between 3 months and 12 months and vary by organization, patient anxiety level, and self-awareness. Surveillance for recurrent disease varies by provider and country as well. Ultrasound appears most sensitive for detecting nodal metastases, and PET/CT is the most sensitive for distant metastatic disease. However, the survival benefit for detection of surgically resectable recurrences is minimal, and more research is needed to identify how early detection of recurrence can maximally benefit these patients.
Acknowledgments
The authors would like to thank the Department of Scientific Publications at MD Anderson for their editing assistance. This work was supported in part by National Institutes of Health grant T32 CA009599.
Disclosure
The authors declare no conflicts of interest in this work.
References
- SiegelRLMillerKDJemalACancer statistics, 2015CA Cancer J Clin201565152925559415
- CooperSThe First Lines of the Theory and Practice of SurgeryLondonLongman Orme, and Co1840
- HowladerNNooneAKrapchoMSEER Cancer Statistics Review, 1975–2011 Available from: http://seer.cancer.gov/csr/1975_2011/Accessed October 3, 2015
- BalchCMGershenwaldJESoongSJFinal version of 2009 AJCC melanoma staging and classificationJ Clin Oncol200927366199620619917835
- XingYChangGJHuCYConditional survival estimates improve over time for patients with advanced melanoma: results from a population-based analysisCancer201011692234224120187100
- National Comprehensive Cancer NetworkNCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Melanoma Version 22015 Available from: http://www.nccn.org/professionals/physician_gls/pdf/melanoma.pdfAccessed February 23, 2015
- MortonDLCochranAJThompsonJFMulticenter Selective Lymphadenectomy Trial GroupSentinel node biopsy for early-stage melanoma: accuracy and morbidity in MSLT-I, an international multicenter trialAnn Surg20052423302311 discussion 311–30316135917
- HyngstromJRChiangYJCromwellKDProspective assessment of lymphedema incidence and lymphedema-associated symptoms following lymph node surgery for melanomaMelanoma Res201323429029723752305
- ChangSBAskewRLXingYProspective assessment of postoperative complications and associated costs following inguinal lymph node dissection (ILND) in melanoma patientsAnn Surg Oncol201017102764277220336388
- RobertCKaraszewskaBSchachterJImproved overall survival in melanoma with combined dabrafenib and trametinibN Engl J Med20153721303925399551
- HodiFSLeeSMcDermottDFIpilimumab plus sargramostim vs ipilimumab alone for treatment of metastatic melanoma: a randomized clinical trialJAMA2014312171744175325369488
- FlahertyLEOthusMAtkinsMBSouthwest Oncology Group S0008: a phase III trial of high-dose interferon Alfa-2b versus cisplatin, vinblastine, and dacarbazine, plus interleukin-2 and interferon in patients with high-risk melanoma – an intergroup study of cancer and leukemia Group B, Children’s Oncology Group, Eastern Cooperative Oncology Group, and Southwest Oncology GroupJ Clin Oncol201432333771377825332243
- ZiefleSEgbertsFHeinzeSHealth-related quality of life before and during adjuvant interferon-alpha treatment for patients with malignant melanoma (DeCOG-trial)J Immunother201134440340821499123
- BottomleyACoensCSuciuSAdjuvant therapy with pegylated interferon alfa-2b versus observation in resected stage III melanoma: a phase III randomized controlled trial of health-related quality of life and symptoms by the European Organisation for Research and Treatment of Cancer Melanoma GroupJ Clin Oncol200927182916292319433686
- TrommeIDevleesschauwerBBeutelsPHealth-related quality of life in patients with melanoma expressed as utilities and disability weightsBr J Dermatol201417161443145025039853
- Schlesinger-RaabASchubert-FritschleGHeinRQuality of life in localised malignant melanomaAnn Oncol201021122428243520494965
- BickersDRLimHWMargolisDAmerican Academy of Dermatology Association, Society for Investigative DermatologyThe burden of skin diseases: 2004 a joint project of the American Academy of Dermatology Association and the Society for Investigative DermatologyJ Am Acad Dermatol200655349050016908356
- MorrisSCoxBBosanquetNCost of skin cancer in EnglandEur J Health Econ200910326727318791757
- The World BankHealth Expenditure Per Capita (Current US$)2015 Available from: http://data.worldbank.org/indicator/SH.XPD.PCAP?page=2
- AlexandrescuDTMelanoma costs: a dynamic model comparing estimated overall costs of various clinical stagesDermatol Online J200915111
- ReyesCDaCosta ByfieldSLinkeRSatram-HoangSTeitelbaumAHThe burden of metastatic melanoma: treatment patterns, healthcare use (utilization), and costsMelanoma Res201323215916623370422
- DavisKLMitraDKotapatiSIbrahimRWolchokJDDirect economic burden of high-risk and metastatic melanoma in the elderly: evidence from the SEER-Medicare linked databaseAppl Health Econ Health Policy200971314119558193
- TsaoHRogersGSSoberAJAn estimate of the annual direct cost of treating cutaneous melanomaJ Am Acad Dermatol1998385 pt 16696809591809
- SeidlerAMPennieMLVeledarECullerSDChenSCEconomic burden of melanoma in the elderly population: population-based analysis of the surveillance, epidemiology, and end results (SEER) – Medicare dataArch Dermatol2010146324925620231494
- YabroffKRLamontEBMariottoACost of care for elderly cancer patients in the United StatesJ Natl Cancer Inst2008100963064118445825
- SouzaRJMattediAPRezendeMLCorrea MdePDuarteEMAn estimate of the cost of treating melanoma disease in the state of Sao Paulo – BrazilAn Bras Dermatol200984323724319668936
- CormierJNXingYDingMCost effectiveness of adjuvant interferon in node-positive melanomaJ Clin Oncol200725172442244817557957
- LosinaEWalenskyRPGellerAVisual screening for malignant melanoma: a cost-effectiveness analysisArch Dermatol20071431212817224538
- GordonLGRowellDHealth system costs of skin cancer and cost-effectiveness of skin cancer prevention and screening: a systematic reviewEur J Cancer Prev201524214114925089375
- JohnsonNMantDNewtonJYudkinPLRole of primary care in the prevention of malignant melanomaBr J Gen Pract1994443885235267748650
- PettersonSMLiawWRTranCBazemoreAWEstimating the residency expansion required to avoid projected primary care physician shortages by 2035Ann Fam Med201513210711425755031
- ZouridakisGWadhawanTSituNMelanoma and other skin lesion detection using smart handheld devicesMethods Mol Biol2015125645949625626557
- StoeckerWVRaderRKHalpernADiagnostic inaccuracy of smart-phone applications for melanoma detection: representative lesion sets and the role for adjunctive technologiesJAMA Dermatol2013149788423864094
- KassianosAPEmeryJDMurchiePWalterFMSmartphone applications for melanoma detection by community, patient and generalist clinician users: a reviewBr J Dermatol201517261507151825600815
- FeigBWChingCDThe MD Anderson Surgical Oncology Handbook5th edPhiladelphia, PALippincott Williams & Wilkins20126667
- LinosESwetterSMCockburnMGColditzGAClarkeCAIncreasing burden of melanoma in the United StatesJ Invest Dermatol200912971666167419131946
- BalchCMThompsonJFGershenwaldJEAge as a predictor of sentinel node metastasis among patients with localized melanoma: an inverse correlation of melanoma mortality and incidence of sentinel node metastasis among young and old patientsAnn Surg Oncol20142141075108124531700
- SiegelRMaJZouZJemalACancer statistics, 2014CA Cancer J Clin201464192924399786
- GandiniSSeraFCattaruzzaMSMeta-analysis of risk factors for cutaneous melanoma: II. Sun exposureEur J Cancer2005411456015617990
- GoodsonAGGrossmanDStrategies for early melanoma detection: Approaches to the patient with neviJ Am Acad Dermatol2009605719735 quiz 736–71819389517
- CarliPde GiorgiVChiarugiAAddition of dermoscopy to conventional naked-eye examination in melanoma screening: a randomized studyJ Am Acad Dermatol200450568368915097950
- WattsCGDiengMMortonRLMannGJMenziesSWCustAEClinical practice guidelines for identification, screening and follow-up of individuals at high risk of primary cutaneous melanoma: a systematic reviewBr J Dermatol20151721334725204572
- ChatzinasiouFLillCMKypreouKComprehensive field synopsis and systematic meta-analyses of genetic association studies in cutaneous melanomaJ Natl Cancer Inst2011103161227123521693730
- Eckerle MizeDBishopMResseESluzevichJFamilial atypical multiple mole melanoma syndromeRiegert-JohnsonDLBoardmanLAHefferonTRobertsMCancer SyndromesBethesda, MDNational Center for Biotechnology Information (US)2009
- HaenssleHAKorpasBHansen-HaggeCSelection of patients for long-term surveillance with digital dermoscopy by assessment of melanoma risk factorsArch Dermatol2010146325726420231495
- BichakjianCKHalpernACJohnsonTMAmerican Academy of DermatologyGuidelines of care for the management of primary cutaneous melanoma. American Academy of DermatologyJ Am Acad Dermatol20116551032104721868127
- health.govt.nz [webpage on the Internet]Clinical practice guidelines for the management of melanoma in Australia and New Zealand2008 [cited June 02, 2008]. Available from: http://www.health.govt..nz/publication/clinical-practice-guidelines-management-melanoma-australia-and-new-zealandAccessed August 25, 2015
- BC Cancer AgencyCancer management guidelines: melanomaVancouverBC Cancer Agency Available from: http://www.bccancer.bc.ca/health-professionals/professional-resources/cancer-management-guidelines/skin/melanomaAccessed on May 1, 2015
- Finnish Medical Society Duodecim and Chirugia Plastici Fenniaen Working GroupIhomelanooma (Melanoma of the Skin)HelsinkiDuodecim Medical Publications Ltd2012
- PflugfelderAKochsCBlumAMalignant melanoma S3-guideline “diagnosis, therapy and follow-up of melanoma”J Dtsch Dermatol Ges201311Suppl 6111624028775
- Dutch Working Group on MelanomaMelanoma guideline 2012UtrechtIntegraal Kankercentrum Nederland2013 Available from: http://www.oncoline.nl/uploaded/docs/melanoom/201208_vertaling%20Richtlijn%20melanoom%20def.pdfAccessed August 25, 2015
- Guidelines Working GroupNational guidelines for diagnosis, treatment and follow-up of malignant melanomasOsloNorwegian Directorate of Health2011
- WattsCGCustAEMenziesSWCoatesEMannGJMortonRLSpecialized surveillance for individuals at high risk for melanoma: a cost analysis of a high-risk clinicJAMA Dermatol2015151217818625389712
- KasparianNAMcLooneJKMeiserBSkin cancer-related prevention and screening behaviors: a review of the literatureJ Behav Med200932540642819521760
- BertolinMCercattoMCRequenaCAwareness, attitude, and adherence to preventive measures in patients at high risk of melanoma. A cross-sectional study on 185 patientsJ Cancer Educ Epub20141216
- BerwickMBeggCBFineJARoushGCBarnhillRLScreening for cutaneous melanoma by skin self-examinationJ Nat Cancer Inst199688117238847720
- BergAOAllanJDIntroducing the third US Preventive Services Task ForceAm J Prev Med2001203 Suppl3411306224
- AzourySCLangeJREpidemiology, risk factors, prevention, and early detection of melanomaSurg Clin North Am2014945957
- CromwellKDRossMIXingYVariability in melanoma post-treatment surveillance practices by country and physician specialty: a systematic reviewMelanoma Res201222537638522914178
- XingYCromwellKDCormierJNReview of diagnostic imaging modalities for the surveillance of melanoma patientsDermatol Res Pract2012201294192121876688
- MathewsJDForsytheAVBradyZCancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million AustraliansBMJ2013346f236023694687
- XingYBronsteinYRossMIContemporary diagnostic imaging modalities for the staging and surveillance of melanoma patients: a meta-analysisJ Natl Cancer Inst2011103212914221081714
- RuethNMXingYChiangYJIs surveillance imaging effective for detecting surgically treatable recurrences in patients with melanoma? A comparative analysis of stage-specific surveillance strategiesAnn Surg201425961215122224096759
- LeiterUBuettnerPGEigentlerTKForschnerAMeierFGarbeCIs detection of melanoma metastasis during surveillance in an early phase of development associated with a survival benefit?Melanoma Res201020324024620216239
- MichielinOHoellerCGaining momentum: New options and opportunities for the treatment of advanced melanomaCancer Treat Rev Epub201564
- ArmstrongBKKrickerAHow much melanoma is caused by sun exposure?Melanoma Res1993363954018161879
- RigelDSCancer of the SkinPhiladelphiaSaunders2005
- Therapeutic Goods AdministrationAustralian Regulatory Guidelines for SunscreensAustraliaTherapeutic Goods Administration2012
- Health CanadaSunscreen Monograph2013 Available from: http://webprod.hc-sc.gc.ca/nhpid-bdipsn/atReq.do?atid=sunscreen-ecransolaire&Accessed March 30, 2015
- US Food Drug AdministrationFDA Sheds Light on Sunscreen2012 Available from: http://www.fda.gov/forconsumers/consumerupdates/ucm258416.htmAccessed March 30, 2015
- Cosmetics EuropeThe European Commission Recommendation on the Efficacy of Sunscreen Products n.d. Available from: https://www.cosmeticseurope.eu/using-cosmetics-colipa-the-european-cosmetic-cosmetics-association/sun-products/the-european-commission-recommendation-on-the-efficacy-of-sunscreen-products.htmlAccessed March 30, 2015
- National Cancer InstituteNational Cancer Institute: PDQ Skin Cancer Prevention Available from: http://cancer.gov/cancertopics/pdq/prevention/skin/HealthProfessionalAccessed March 30, 2015
- GimottyPAGlanzKSunscreen and melanoma: what is the evidence?J Clin Oncol201129324925021135278
- GreenACWilliamsGMLoganVStruttonGMReduced melanoma after regular sunscreen use: randomized trial follow-upJ Clin Oncol201129325726321135266
- American Academy of DermatologySunscreen FAQs2015 Available from: https://www.aad.org/media-resources/stats-and-facts/prevention-and-care/sunscreen-faqsAccessed April 10, 2015
- American Cancer SocietyCan Melanoma Skin Cancer be Prevented?2015 Available from: http://www.cancer.org/cancer/skincancer-melanoma/detailedguide/melanoma-skin-cancer-preventionAccessed April 1, 2015
- Cancer Council AustraliaPreventing Skin Cancer2015 n.d. Available from: http://www.cancer.org.au/preventing-cancer/sun-protection/preventing-skin-cancer/Accessed March 31, 2015
- World Health OrganizationSun Protection Available from: http://www.who.int/uv/sun_protection/en/Accessed April 1, 2015
- DennisLKVanbeekMJBeane FreemanLESmithBJDawsonDVCoughlinJASunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysisAnn Epidemiol200818861462718652979
- World Health OrganizationSun Protection and Schools: How to Make a Difference2003 Available from: http://www.who.int/uv/publications/en/sunprotschools.pdf?ua=1Accessed March 30, 2015
- US Environmental Protection AgencyLearn about SunWise2014 Available from: http://www2.epa.gov/sunwise/learn-about-sunwiseAccessed April 1, 2015
- KyleJWHammittJKLimHWEconomic evaluation of the US Environmental Protection Agency’s SunWise program: sun protection education for young childrenPediatrics20081215e1074e108418450850
- HorshamCAusterJSendallMCInterventions to decrease skin cancer risk in outdoor workers: update to a 2007 systematic reviewBMC Res Notes201471024397996
- MayerJASlymenDJClappEJPromoting sun safety among US Postal Service letter carriers: impact of a 2-year interventionAm J Pub Health200797355956517267715
- DavyLBoyettTWeathersLCampbellRJRoetzheimRGSun protection counseling by pediatriciansAmbul Pediatr20022320721112014981
- DolanNCNgJSMartinGJRobinsonJKRademakerAWEffectiveness of a skin cancer control educational intervention for internal medicine housestaff and attending physiciansJ Gen Intern Med19971295315369294786
- BandiPCokkinidesVEWeinstockMAWardEMPhysician sun protection counseling: prevalence, correlates, and association with sun protection practices among US adolescents and their parents, 2004Prev Med201051217217720478331
- RobinsonJDSilkKJParrottRLSteinerCMorrisSMHoneycuttCHealthcare providers’ sun-protection promotion and at-risk clients’ skin-cancer-prevention outcomesPrev Med200438325125714766106
- US Preventive Services Task ForceRecommendation Summary2012 Available from: http://www.uspreventiveservicestaskforce.org/Page/Topic/recommendation-summary/skin-cancer-counselingAccessed March 30, 2015
- El GhissassiFBaanRStraifKA review of human carcinogens – part D: radiationLancet Oncol200910875175219655431
- International Agency for Research on Cancer Working Group on Artificial Ultraviolet Light and Skin CancerThe association of use of sunbeds with cutaneous malignant melanoma and other skin cancers: A systematic reviewInt J Cancer200712051116112217131335
- Food, Drug Administration HHSGeneral and plastic surgery devices: reclassification of ultraviolet lamps for tanning, henceforth to be known as sunlamp products and ultraviolet lamps intended for use in sunlamp products. Final orderFed Regist201479105312053121424908684
- National Conference of State LegislaturesIndoor Tanning Restrictions for Minors – A State-by-State Comparison Available from: http://www.ncsl.org/research/health/indoor-tanning-restrictions.aspxAccessed March 11, 2015
- ForsterJLLazovichDHickleASorensenGDemierreMFCompliance with restrictions on sale of indoor tanning sessions to youth in Minnesota and MassachusettsJ Am Acad Dermatol200655696296717097392
- PawlakMTBuiMAmirMBurkhardtDLChenAKDellavalleRPLegislation restricting access to indoor tanning throughout the worldArch Dermatol201214891006101222801924
- MulcahyNAustralia Bans Tanning Salons2015 Available from: http://www.medscape.com/viewarticle/838407Accessed March 11, 2015
- HolmanDMFoxKAGlennJDStrategies to reduce indoor tanning: current research gaps and future opportunities for preventionAm J Prev Med201344667268123683986
- Australian-Cancer-Network-Melanoma-Guidelines-Revision-Working-PartyClinical Practice Guidelines for the Management of Melanoma in Australia and New ZealandWellingtonSydney and New Zealand Guidelines Group2008
- ThompsonJFShawHMStretchJRMcCarthyWHMiltonGWThe Sydney Melanoma Unit – a multidisciplinary melanoma treatment centerSurg Clin North Am200383243145112744618
- FranckenABAccorttNAShawHMFollow-up schedules after treatment for malignant melanomaBr J Surg200895111401140718844268
- KerseyPAIscoeNAGapskiJAThe value of staging and serial follow-up investigations in patients with completely resected, primary, cutaneous malignant melanomaBr J Surg19857286146174027532
- GarbeCHauschildAVolkenandtMEvidence and interdisciplinary consense-based German guidelines: diagnosis and surveillance of melanomaMelanoma Res200717639339917992123
- UgurelSEnkASkin cancer: follow-up, rehabilitation, palliative and supportive careJ Dtsch Dermatol Ges200866492498 quiz 49918494711
- GarbeCPaulAKohler-SpäthHProspective evaluation of a follow-up schedule in cutaneous melanoma patients: recommendations for an effective follow-up strategyJ Clin Oncol200321352052912560444
- RobertsDLAnsteyAVBarlowRJBritish Association of Dermatologists, Melanoma Study GroupUK guidelines for the management of cutaneous melanomaBr J Dermatol2002146171711841361
- MeierFWillSEllwangerUMetastatic pathways and time courses in the orderly progression of cutaneous melanomaBr J Dermatol20021471627012100186
- MarsdenJRNewton-BishopJABurrowsLBritish Association of Dermatologists (BAD) Clinical Standards UnitRevised UK guidelines for the management of cutaneous melanoma 2010J Plast Reconstr Aesthet Surg20106391401141920728418
- NCCN Clinical Practice Guidelines in Oncology: Melanoma2010 Available from: http://www.nccn.org/professionals/physician_gls/PDF/melanoma.pdfAccessed August 22, 2011
- SoberAJChuangTYDuvicMGuidelines of care for primary cutaneous melanomaJ Am Acad Dermatol200145457958611568750
- American Cancer Society, National Comprehensive Cancer NetworkMelanoma: treatment guidelines for patients (part 2)Dermatol Nurs200517319119816035420
- OlsonJAJrJaquesDPCoitDGHwuWJStaging work-up and post-treatment surveillance of patients with melanomaClin Plast Surg2000273377390viii10941559
- RomeroJBStefanatoCMKopfAWBartRSFollow-up recommendations for patients with stage I malignant melanomaJ Dermatol Surg Oncol19942031751788151030
- RumkePvan EverdingenJEConsensus on the management of melanoma of the skin in The Netherlands. Dutch Melanoma Working PartyEur J Cancer1992282–36006041591078
- NiewegOEKroonBBThe conundrum of follow-up: should it be abandoned?Surg Oncol Clin N Am200615231933016632217
- KroonBBNiewegOEHoekstraHJLejeuneFJPrinciples and guidelines for surgeons: management of cutaneous malignant melanoma. European Society of Surgical Oncology BrusselsEur J Surg Oncol19972365505589484929
- FranckenABBastiaannetEHoekstraHJFollow-up in patients with localised primary cutaneous melanomaLancet Oncol20056860862116054572
- DummerRPanizzonRBlochPHBurgGUpdated Swiss guidelines for the treatment and follow-up of cutaneous melanomaDermatology20052101394415604544
- DummerRGuggenheimMArnoldAWBraunRvon MoosRUpdated Swiss guidelines for the treatment and follow-up of cutaneous melanomaSwiss Med Wkly2011141w1332022180245
- ManceboSEHuJYWangSQSunscreens: a review of health benefits, regulations, and controversiesDermatol Clin2014323427438x24891063
