Abstract
Psoriasis is a common skin disease, with nail involvement in approximately 80% of patients. Nail psoriasis is often associated with psoriatic arthropathy. Involvement of the nails does not always have relationship with the type, gravity, extension, or duration of skin psoriasis. Nail psoriasis can occur at any age and all parts of the nails and the surrounding structures can be affected. Two clinical patterns of nail manifestations have been seen due to psoriasis: nail matrix involvement or nail bed involvement. In the first case, irregular and deep pitting, red spots of the lunula, crumbling, and leukonychia are seen; in the second case, salmon patches, onycholysis with erythematous border, subungual hyperkeratosis, and splinter hemorrhages are observed. These clinical features are more visible in fingernails than in toenails, where nail abnormalities are not diagnostic and are usually clinically indistinguishable from other conditions, especially onychomycosis. Nail psoriasis causes, above all, psychosocial and aesthetic problems, but many patients often complain about functional damage. Diagnosis of nail psoriasis is clinical and histopathology is necessary only in selected cases. Nail psoriasis has an unpredictable course but, in most cases, the disease is chronic and complete remissions are uncommon. Sun exposure does not usually improve and may even worsen nail psoriasis. There are no curative treatments. Treatment of nail psoriasis includes different types of medications, from topical therapy to systemic therapy, according to the severity and extension of the disease. Moreover, we should not underestimate the use of biological agents and new therapy with lasers or iontophoresis. This review offers an investigation of the different treatment options for nail psoriasis and the optimal management of nail disease in patients with psoriasis.
Introduction
Psoriasis is a chronic and recurrent inflammatory skin disease with nail involvement observed in approximately 80% of patients. Nail psoriasis may also occur as the only manifestation of the disease.Citation1,Citation2 Nail psoriasis can appear at any age and all nails can be affected. The nail matrix or nail bed can be involved in the disease. Nail psoriasis causes, above all, psychosocial and aesthetic problems, leading to significant repercussions in the quality of life, but many patients often also complain about functional damage.Citation3 Cosmetic and functional damage, referred by 93% of patients with nail psoriasis, is sometimes so extensive that the patients tend to hide their hands and/or feet or shy away from social and business activities.Citation4
The treatment of nail psoriasis involves different types of medications, from topical therapy to systemic therapy, according to the severity and extension of the disease. A standardized therapy does not exist, and the therapeutic choice is based on clinical manifestations and symptoms of the patient. Once the diagnosis has been defined, the severity of the disease should be assessed with a validated score, to decide the best treatment.
Clinical manifestations
Clinical manifestations of nail psoriasis depend on the nail site that is affected: the nail matrix, the nail bed, the proximal nail fold, or the hyponychium.Citation5 It is possible to observe an isolated involvement of a few fingers or lesions of all nails on both hands and feet.
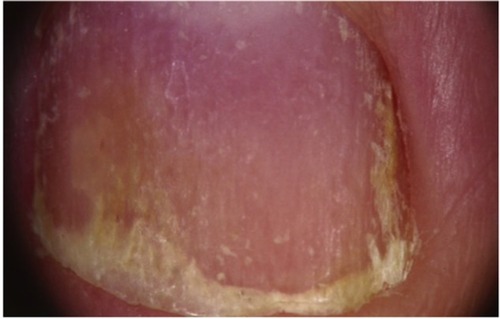
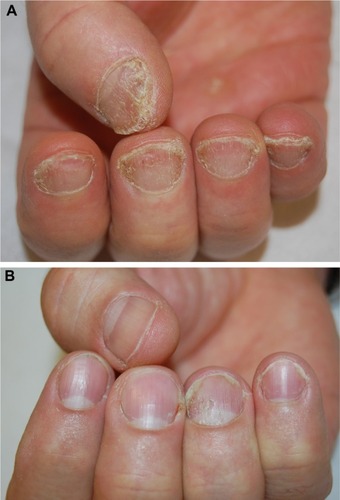
The severity of nail psoriasis depends largely on the nail part affected by the inflammatory reaction. The most severe changes are observed when the disease affects the nail matrix, a germinative epithelium that produces the nail plate. When the matrix is affected, psoriasis signs are pitting, leukonychia, lunula red spots, and nail plate crumbling (). The nail bed is responsible for the adhesion of the nail plate; it is richly vascularized by capillaries oriented longitudinally in parallel ridges. Alterations of the nail bed due to nail psoriasis include onycholysis, subungual hyperk-eratosis, oil drop or salmon spots, dyschromias, and splinter hemorrhages ().
The most common sign of nail psoriasis is pitting, which is a focal defect of keratinization of the proximal matrix, with persistence of groups of nucleated and incompletely keratinized (parakeratotic) cells within the upper layers in the dorsal nail plate. These clusters poorly adhere to each other and are easily detachable, leaving pits on the surface of the nail plate. The term pitting describes the presence of small depressions on the nail plate surfaceCitation6 (). Psoriatic pits are usually large and deep, with irregular and uneven shape and distribution; they may be covered by whitish, easily detachable scales. The fingernails are more often affected than the toenails. Pits may be the only manifestation of nail psoriasis or they may be associated with other signs.
Another possible sign of nail matrix psoriasis is the presence of red spots in the lunula (mottled lunula), a nonspecific sign that can also be due to nail lichen planus and eczema.
Severe nail matrix involvement induces nail plate crumbling, with a fragile and grossly deformed nail plate.
Onycholysis surrounded by an erythematous border is typical of nail bed psoriasis. Onycholysis is the detachment of the nail plate from the nail bed. In psoriasis, the onycholytic area is typically separated from the normal nail plate by an erythematous borderCitation6 ().
Figure 4 Enhanced visualization of onycholysis surrounded by an erythematous border with dermoscopy (original magnification: ×20).

Subungual hyperkeratosis describes the accumulation of scales under the distal portion of the nail plate, with nail thickening and uplifting. It most frequently involves the toenails. Splinter hemorrhages appear as longitudinal linear red–brown areas of hemorrhage, often seen in fingernails and located in the distal portion of the nail plate. They are a consequence of psoriatic involvement of the nail bed capillary vessels that run in a longitudinal direction along the nail bed dermal ridges. They are not specific of the disease.
Dyschromias of the nail are also frequent in nail psoriasis and the most typical signs are the ‘oil drop sign’ or salmon patches, which appear as irregular areas of yellow–orange discoloration easily visible through the transparent nail plate.Citation7
Diagnosis
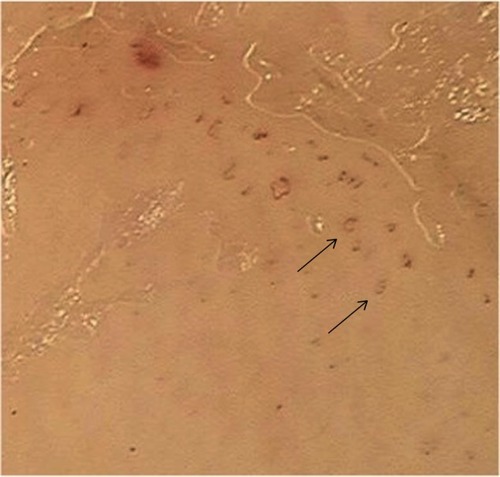
The diagnosis of nail psoriasis is usually based on clinical manifestations. As the clinical features of nail psoriasis are not exclusive for the disease, clinical differentiation between other conditions, such as onychomycosis, can be difficult. The nail discoloration and subungual hyper keratosis observed in nail psoriasis may also be present in onychomycosis. The use of dermoscopy, a noninvasive tool, can be useful in differential diagnosis: in nail psoriasis, it shows onycholysis with erythematous border (), represented by a reddish–orange stain surrounding the onycholytic area; whereas in onychomycosis, it shows a jagged proximal edge with spikes of onycholysis and longitudinal striae.Citation8,Citation9 Onychomycosis and psoriasis may also be present in the same nail.Citation10 Another dermoscopic sign of nail psoriasis is the presence of vascular abnormalities in the hyponichium, where the capillaries are visible, dilated, tortuous, elongated, and irregularly distributed (). The capillary density is correlated with the severity of the nail condition and improves with response to therapy.Citation11 Periungual capillaroscopy may be a useful diagnostic tool for detecting nail psoriasis, where it shows a decreased capillary density in the periungual area and the presence of coiled capillary loops.Citation12
Figure 5 Dilated tortuous vessels of hyponychium with dermoscopy (original magnification: ×40).
Nail biopsy maybe necessary in selected cases. Matrix or nail bed biopsy is performed based on the clinical manifestation of nail psoriasis. Hanno et alCitation13 identified some criteria for pathological diagnosis of nail psoriasis: presence of neutrophils in nail bed epithelium as the major criterion; and hyperkeratosis with parakeratosis, exudates on corneal epithelium, focal hypogranulosis, and psoriasiform hyperplasia as minor criteria. It is important to perform periodic acid–Schiff staining for differential diagnosis between psoriasis and onychomycosis.Citation14
Recently, new diagnostic techniques have been suggested. Ultrasonography of the psoriatic nails shows hyperechoic parts or loss of definition of the nail plates, which can involve only the ventral part or the whole nail. The nail bed is thickened and shows an increased blood flow with power Doppler technique.Citation15 Optical coherence tomography provides images of tissue pathology in situ. In nail psoriasis, this technique shows a grossly irregular ventral nail plate irregularly fused with the underlying epidermis.Citation16 Another new technique is confocal laser scanning microscopy, which can visualize, in a noninvasive manner, cell structures of the skin up to a depth of 300 µm in vivo. This tool allows one to measure in a better way the thickness and the different layers of nail plate and gives better information on the microscopic structures than ultrasonography and optical coherence tomography.Citation17
The most difficult differential diagnosis of nail psoriasis is onychomycosis, which may produce nail changes very similar to nail bed psoriasis. Another important disease to distinguish is nail lichen planus, which can be distinguished by absence of pitting and presence of longitudinal fissuring and, sometimes, dorsal pterygium. Pits are not exclusive to psoriasis; they can also be seen in alopecia areata and eczema.Citation2 Nail pitting of alopecia areata is usually differentiated from that of nail psoriasis by the regular pattern of the depressions, which are superficial and geometrically distributed.
Assessment of psoriatic nail disease
There are many different scores specifically developed to assess the severity and to evaluate the courses of both disease and therapy in nail psoriasis. The only validated method to diagnose nail psoriasis is the NAPSI (Nail Psoriasis Severity Index), which is the most commonly used worldwide.
The NAPSI divides the affected nail into four quadrants, investigating each part for the presence of typical lesions. It exams both nail matrix (pitting, leukonychia, red spots of the lunula, and crumbling) and bed (oil drop patches, onycholysis, hyper keratosis, and splinter hemorrhage). A value ranging from 0 to 8 is added for each nail affected; so the maximum score for each hand or foot is 0–160. The higher the NAPSI score, the worse is the nail involvement.Citation18
Nail psoriasis causes both physical and psychological discomfort, and this is not included in the NAPSI score. In 2010, Ortonne et alCitation19 therefore devised the NPQ10 (Nail Psoriasis Quality of Life Scale) to evaluate the impact of nail psoriasis on quality of life. This questionnaire is a valid and reproducible method based on ten specific questions that investigate the impact of nail psoriasis on life. The questionnaire was administered to 1,309 patients and the results showed that nail psoriasis is evaluated as unsightly in 87% of patients and painful in 59% of patients.Citation19 Klaassen et alCitation20 showed that nail psoriasis can have devastating effects on quality of life, especially in female patients, in patients with associated psoriatic arthritis, and more particularly, in those with severe nail psoriasis. The NPQ10 highlighted the daily restrictions of patients with nail psoriasis, especially in patients with major chronic diseases such as cardiovascular disease, diabetes mellitus, and depression. Using this questionnaire was useful to individualize treatment strategies for each patient.Citation20
The newest and internationally validated method of measuring the severity of nail psoriasis is the NAPPA (Nail Assessment in Psoriasis and Psoriatic Arthritis) score. This score evaluates both the quality of life and the therapeutic course of the disease.Citation21 The NAPPA has been used in clinical studies as well as in routine care.
Treatment of nail psoriasis
The choice of treatment for nail psoriasis is a dilemma to the dermatologist for various reasons. To ensure that each patient receives the right treatment, it is necessary to evaluate many factors, such as the severity of the nail condition, the extension of the clinical manifestations on the skin, the joint involvement, and the previous response to therapeutic treatment. Often, patients have already been visited by other specialists without attaining good results and the impact on quality of life is very high. Sometimes, treatment failure occurs for various reasons that do not depend on the patient or dermatologist.
The nail has an anatomical structure that does not allow the absorption of topical medications at the level of the nail plate and this is amplified in nail psoriasis due to the presence of subungual hyperkeratosis. Nail psoriasis rarely responds to topical treatment and is often aggravated by exposure to the sun. The degree of penetration of topical medications is crucial. Furthermore, nail growth is very slow and therefore requires long-term treatment that may decrease patient compliance and increase the risk of drug toxicity. For this reason, the use of systemic drugs is recommended in cases of skin or joint involvement or in cases of severe nail psoriasis with poor therapeutic response to topical drugs.
Unfortunately, there is no standardized treatment regimen for the treatment of nail psoriasis and the choice of therapy depends on several factors, including the patient’s history and clinical manifestations such as sex, age, severity of nail psoriasis, the disease’s course over time, concomitant diseases and medications, and the benefits and risks of treatment.
Treatment options for nail psoriasis are summarized in .
Table 1 Treatment options for nail psoriasis
Before starting treatment for nail psoriasis, it is necessary to consider various factors that are often underestimated. First of all, we must teach patients to keep nails short and cut off the onycholytic area so that topical therapies penetrate more and the exogenous material does not accumulate. Trauma should be avoided, so that the clinical manifestations do not deteriorate due to the Koebner phenomenon. For example, removal of the subungual material with sharp objects worsens the onycholysis.
Topical therapies
Topical treatments are often the first choice, but their effectiveness is limited to nail bed psoriasis; they are not effective on nail matrix psoriasis because they do not penetrate the nail plate and proximal nail fold. Topical treatments are formulated using different vehicles, including lacquer, creams, ointments, and tinctures, and may be applied on the nail plate or massaged into the nail bed and hyponychium or utilized under occlusion in order to increase their effect. Corticosteroids and vitamin D3 analogues are the first choice of treatment for nail bed psoriasis. Other local therapies used in nail psoriasis are 5-fluorouracil, cyclosporin A tazarotene, anthralin, and urea. Topical therapy is effective in nail bed psoriasis for the remedial action on onycholysis and subungual hyperkeratosis.
Corticosteroids
Potent or very potent corticosteroids are the most effective drugs in nail psoriasis, the most common being clobetasol propionate (0.05%)Citation22 and betamethasone dipropionate (0.05%).Citation23 They can be used once or twice daily. Recently, a pilot studyCitation24 of 15 patients published in 2012 compared the efficacy of clobetasol in nail lacquer at concentrations of 0.5%, 1.0%, and 8.0%. The formulation containing 8% clobetasol-17-propionate in colorless nail lacquer showed good clinical results and proved cosmetically highly acceptable for the treatment of nail bed and matrix psoriasis without joint involvement.Citation24 The side effects of corticosteroids, especially under occlusion and when applied for long periods, are skin atrophy and, rarely, if prolonged for more than a year, the atrophy of the underlying phalanx known as “disappearing digit”,Citation25,Citation26 formation of striae and telangiectasia, tachyphylaxis, and systemic absorption.Citation6
Vitamin D3 analogues
The efficacy of topical calcipotriol in nail psoriasis was compared with that of the high-potency corticosteroids. In an open study, 62 patients were treated with topical calcipotriol once daily 5 days a week, as well as with clobetasol propionate (0.05%) cream twice a week, for a total of 6 months. The authors reported a reduction of hyperkeratosis by 35.2% in fingernails and 72.3% in the toenails.Citation22 In a controlled double-blind study of 58 patients for a period of 6 months, the authors demonstrated that twice a day of calcipotriol ointment had a similar efficacy as betamethasone dipropionate (0.05%) in treating subungual hyperkeratosis after 3–9 months.Citation23 The use of calcipotriol is preferred to avoid the side effects such as atrophy caused by steroids, but vitamin D3 analogues may cause erythema, periungual irritation, and burning sensation at the site of application and should never be applied under occlusion. After stopping therapy, the patient’s nail condition generally worsens again.
Tazarotene
Tazarotene is a topical retinoid with already proven effectiveness in onycholysis, discoloration, pitting, and hyperkeratosis. It is used in gel or cream form for a period of 12–24 weeks. In 2007, Rigopoulos et alCitation27 demonstrated a similar efficacy of tazarotene (0.1%) cream and clobetasol propionate (0.05%) cream treatment in a double-blind study involving 46 patients for 12 weeks.Citation27 The drug may cause local irritation.
Other topical treatments that have been shown to be effective against nail psoriasis include tacrolimus, 5-fluorouracil, cyclosporin A, and anthralin.
Combination therapies
The use of combined local therapies has been demonstrated to produce better results in nail psoriasis. A combination of corticosteroids and vitamin D3 analogues shows better efficacy both on the clinical manifestations and on the symptoms reported by patients in nail bed psoriasis. Moreover, the effectiveness of corticosteroids can be enhanced in combination with keratolytic creams, such as topical retinoids or vitamin D3 analogues, allowing greater penetration. Finally, the combination of tazarotene with corticosteroids may help in reducing local irritation and thus enhance its effectiveness.
Intralesional therapies
Intralesional therapy is the injection of small doses of the drug directly into or near the specific structure of the nail unit: nail bed or nail matrix. The drug most frequently used in nail psoriasis is triamcinolone acetonide with a dose ranging from 2.5 mg/mL to 10 mg/mL. There are many methods to inject drugs with different types of needles or with Dermo-Jet syringes. Doses, concentrations, and frequency of injections have not yet been standardized. The most important side effect is pain at the injection site, but this may be reduced with the use of ice or ethyl chloride spray.
Another drug recently used in the treatment of nail psoriasis is intralesional methotrexate. It was used at a dose of 2.5 mg in a single finger of a patient with severe nail psoriasis at the level of the proximal nail fold, once a week for 6 weeks. During the 4-month follow-up, there was evidence of an improvement in pitting and subungual hyperkeratosis, and the results were maintained after 2 years. The only side effect reported was pain, but this is still defined as tolerable.Citation28
Phototherapy, radiotherapy
Phototherapy (ultraviolet B, ultraviolet A [UVA], or psoralen with UVA (PUVA)) is a therapeutic option widely used in skin psoriasis, but it has never found support in nail psoriasis because the rays have a low ability to penetrate the nail plate. Phototherapy requires multiple sessions each week and a therapeutic effect is evident only after a long period. Published studies are not recent and showed an improvement only at the level of the proximal nail fold with the use of PUVA therapy, while no effect was reported with UVB therapy. A recent study proved the ability of penetration of UV lights in normal human cadaveric fingernails and suggested that PUVA could be considered a possible treatment in nail psoriasis,Citation29 although clinical studies are needed.
Radiation therapy in nail psoriasis has been described in a few recent studies. Superficial radiotherapy induced a significant reduction in nail thickness in a double-blind study,Citation30,Citation31 while, more recently, a prospective study of electron beam therapy showed improvement in 9 of 12 patients with nail psoriasis and without joint involvement after 8 weeks of therapy, but the results were lost after 12 months of follow-up.Citation32 However, in addition to the side effects of radiation therapy, such as fibrosis, inflammation, and local pigmentation, there is also the potential risk of carcinogenesis.
Laser therapies
Most studies on lasers for nail psoriasis were performed with the pulsed-dye laser (PDL), which specifically targets blood vessels. The most frequently chosen wavelengths for PDL therapeutic use are 585 nm and 595 nm, which can effectively reach the nail bed through the nail plate. Most recently, PDL has been investigated in nail psoriasis. Four recent studies used PDL for nail psoriasis. The first study compared the efficacy of photodynamic therapy (PDT) and PDL in the therapy of nail psoriasis and compared treatment responses of lesions of the nail matrix versus those of the nail bed in a comparative pilot study of 14 patients. Results showed a reduction in NAPSI score in both treatment groups for both types of nail psoriasis without statistical differences between PDT and PDL.Citation33 The second study evaluated the effect of PDL in nail psoriasis and showed an improvement on onycholysis and subungual hyperkeratosis in five patients.Citation34 The third study compared, in 20 patients, the efficacy and safety of different types of lasers to determine the optimal pulse duration of PDL in nail psoriasis in a randomized, double-blind, intrapatient left-to-right study and showed no significant difference between the groups.Citation35 The last study evaluated the efficacy and safety of PDL with topical retinoid in nail psoriasis of 25 patients and showed a marked improvement in the experimental group versus the control group in a single-blind, intrapatient left-to-right controlled study.Citation36 These studies suggest that PDL may be clinically useful in treating lesions caused by nail matrix and bed psoriasis, but more randomized controlled trials are still needed to standardize PDL in nail psoriasis. Recently, a new single left-to-right comparison study, in 42 patients, compared excimer laser versus PDL and showed that PDL has a good response for treating nail psoriasis, with minimal side effects, while excimer laser is conversely more effective for plaque psoriasis than is PDL.Citation37
Systemic therapies
Systemic therapy is recommended in patients with skin psoriasis or joint involvement but not for those with only nail manifestations. On account of the possible systemic toxicity, the European Consensus recommends the use of systemic therapy only in cases of moderate-to-severe nail psoriasis or when topical therapy, intralesional therapy, or phototherapy has failed.
Systemic therapy used in nail psoriasis comprises immu-nosuppressant drugs such as methotrexate, cyclosporin A, and retinoids.
Methotrexate is one of the most important immunosup-pressive drugs used in inflammatory diseases. The use of methotrexate in nail psoriasis is less studied than its use in skin psoriasis, and its effectiveness is not significantly different from that of other drugs. Methotrexate at low doses (5 mg/week) has been used in a patient with severe 20-nail psoriasis with success in both the fingernails and toenails, which were cured after 9 months and 13 months of therapy, respectively.Citation38 The dosage of methotrexate varies from 5 mg/week to 15 mg/week, and the recommended dose should not exceed 22.5 mg/week. The effectiveness is evident after about 4–6 weeks of therapy. A recent study showed a reduction from 36.8% to 43.3% after 24–52 weeks of therapy and showed a better response in nail matrix psoriasis.Citation39 Possible side effects include liver and kidney toxicity and bone marrow suppression.
Data on the use of cyclosporin A in nail psoriasis are sparse. In a small, uncontrolled study of 16 patients with nail psoriasis and without joint involvement, where cyclosporin A was administered at a dose of 3 mg/kg of body weight, 14 of 16 patients improved, including 10 showing significant improvement and two cured completely.Citation40 Another comparative single-blind study of 54 patients compared the effectiveness of cyclosporin A alone with a combination of cyclosporin A at a dose of 3.5–4.5 mg/kg/day and topical calcipotriol (50 µg/kg twice daily) for 3 months. Results showed an improvement in nail psoriasis of 79% in the combination group and 48% in patients receiving cyclosporin A alone. Furthermore, the relapses after 6 months were less in the combined group.Citation41 In a retrospective evaluation, cyclosporin A was found to improve the NAPSI score after 12, 24, and 48 weeks by 40%, 72%, and 89%, respectively.Citation42
Acitretin is a derivative of vitamin A used successfully in the treatment of pustular psoriasis. Therapeutic response is observed after 4–8 weeks (). An open study involving 36 patients with moderate-to-severe nail psoriasis with low-dose acitretin (0.2–0.3 mg/kg/day) showed an improvement of the NAPSI score in 40.9% patients and a complete healing in 25% patients after 6 months of therapy.Citation43 On the contrary, a Brazilian open study conducted on 20 patients did not show any improvement after 4 months of therapy.Citation44 Side effects are dryness of skin and mucous membranes, hypertriglyceri-demia, and hepatitis.
Biologics
New treatments for nail psoriasis include biological therapies, which have already been proven effective in skin psoriasis and show interesting results in nail psoriasis. Biologics showed a high efficacy in the treatment of nail psoriasis and a higher response when compared to classical therapy, improving both signs and symptoms of severe nail psoriasis. No biological agent showed greater efficacy compared with another agent.
The most studied drug is infliximab, a chimeric monoclonal antibody that blocks tumor necrosis factor (TNF)-α. A phase III multicenter, double-blind, placebo- controlled study evaluated the safety and efficacy of long-term infliximab treatment in 378 patients with moderate-to-severe plaque psoriasis. The second end point of the study was an improvement of nail manifestations. The percentage of improvement in NAPSI was 28.9% after 12 weeks and 51% after 54 weeks of therapy. A complete cure was reported in 30% of patients.Citation45
Another antagonist of the TNF-α receptor is adalimumab. van den Bosch et alCitation46 showed an improvement in NAPSI score of 65% after 20 weeks of therapy with adalimumab 40 mg/week in an open-label uncontrolled study in 442 patients with psoriatic arthritis. Recently, a subanalysis of the effects on scalp and nails of adalimumab in severe psoriasis showed a 39.5% reduction of the NAPSI score after 16 weeks of treatment.Citation47
In an open-label, randomized trial (CRYSTAL) of 711 patients, wherein 80% had nail involvement, etanercept showed a 51% reduction of NAPSI score after 54 weeks of therapy.Citation48
Golimumab is a human monoclonal antibody. A study on arthropathic psoriasis showed a 33% reduction in the NAPSI score after 24 weeks.Citation49
The biologic drug most recently used is ustekinumab, an interleukin-12/23 receptor inhibitor, which has shown good efficacy in nail psoriasis.Citation50 Recently, the efficacy of ustekinumab in nail psoriasis was evaluated in an open-label study (PHOENIX 1), in 766 patients with moderate-to-severe psoriasis, where 71% presented nail disease. At week 24 of therapy, the rate of improvement in NAPSI score was 46.5%. Ustekinumab showed excellent results in nail psoriasis and the improvement continued until after 1 year of treatment with the maintenance dose.Citation51
The debate is still open as to whether biologics, with their well-known side effects, are indicated for use in isolated nail psoriasis, where skin and joints have no symptoms.
Conclusion
Despite the pain and the functional and aesthetic discomfort, nail psoriasis is still a poorly studied disease. The evaluation of nail involvement is important for assessing the severity of psoriasis as it is an index of possible joint involvement, which may require a more substantial treatment. In cases of nail psoriasis, the clinical manifestations should first be observed in order to make a correct diagnosis and then to establish an appropriate treatment. Initially, local therapy may be useful, but in cases of cutaneous or joint involvement, systemic therapy is necessary with conventional or biological agents.
A 2013 Cochrane report on interventions in nail psoriasis assessed evidence for the efficacy and safety of treatments for the disease. They included 18 studies involving 1,226 patients and concluded that infliximab, golimumab, superficial radiotherapy, and electron beam brought about significant nail improvement compared to other treatments. However, the report also comments: “it was not possible to pool and compare the results because the studies were all so different”.Citation52
In conclusion, psoriasis is a chronic and relapsing disease that needs further investigation to choose the best treatment for each individual patient.
Disclosure
The authors report no conflicts of interest in this work.
References
- CassellSKavanaughAFTherapies for psoriatic nail disease. A systematic reviewJ Rheumatol20063371452145616724366
- TanESChongWSTeyHLNail psoriasis: a reviewAm J Clin Dermatol20121337538822784035
- BaranRThe Burden of nail psoriasis: an introductionDermatology2010221Suppl 115
- de JongEMSeegersBAGulinckMKBoezemanJBvan de KerkhofPCPsoriasis of the nails associated with disability in a large number of patients: results of a recent interview with 1728 patientsDermatology19961933003038993953
- de BerkerDNail anatomyClin Dermatol20133150951524079579
- JiaravuthisanMMSassevilleDVenderRBMurphyFMuhnCYPsoriasis of the nail: anatomy, pathology, clinical presentation, and a review of the literature on therapyJ Am Acad Dermatol200757112717572277
- EdwardsFde BerkerDNail psoriasis: clinical presentations and best practice recommendationsDrugs200969172351236119911853
- FariasDCTostiAChiacchioNDHirataSHDermoscopy in nail psoriasisAn Bras Dermatol20108510110320464097
- PiracciniBMBalestriRStaraceMRechGNail digital dermoscopy (onychoscopy) in the diagnosis of onychomycosisJ Eur Acad Dermatol Venereol20132750951322040510
- KlaassenKMGDulakMGvan de KerhofPCMPaschMCThe prevalence of onychomycosis in psoriatic patients: a systematic reviewJ Eur Acad Dermatol Venereol20142853354124033871
- IorizzoMDahdahMVincenziCVideodermoscopy of the hyponychium in nail bed psoriasisJ Am Acad Dermatol20085871471518342725
- RiberioCFSiqueiraEBHollerAPPeriungual capillaroscopy in psoriasisAn Bras Dermatol20128755055322892767
- HannoRMathesBMKrullEALongitudinal nail biopsy in evaluation of acquired nail dystrophyJ Am Acad Dermatol1986148038093711384
- GroverCReddyBSUma ChaturvediKDiagnosis of nail psoriasis: importance of biopsy and histopathologyBr J Dermatol20051531153115816307651
- GutierrezMWortsmanXFilippucciEDe AngelisRFilosaGGrassiWHigh-frequency sonography in the evaluation of psoriasis: nail and skin involvementJ Ultrasound Med2009281569157419854972
- AydinSZAshZDel GaldoFOptical coherence tomography: a new tool to assess nail disease in psoriasis?Dermatology201122231131321791896
- SattlerEKaestleRRothmundGWelzelJConfocal laser scanning microscopy, optical coherence tomography and transonychial water loss for in vivo investigation of nailsBr J Dermatol201216674074622059869
- RichPScherRKNail Psoriasis severity index: a useful tool for evaluation of nail psoriasisJ Am Acad Dermatol20034920621212894066
- OrtonneJPBaranRCorvestMSchmittCVoisardJJTaiebCDevelopment and validation of nail psoriasis quality of life scale (NPQ10)J Eur Acad Dermatol Venereol201024222720050290
- KlaassenKMGvan de KerkhofPCMPaschMCNail psoriasis, the unknown burden of diseaseJ Eur Acad Dermatol Venereol201428121690169524422908
- AugustinMBlomeCCostanzoAFor the NAPPA task force group: conception, development and validation of NAPPA, a novel questionnaire for the assessment of patient-reported outcomes in nail psoriasisBr J Dermatol201470591598
- RigopoulosDIoannidesDPrastitisNNail psoriasis: a combined treatment using calcipotriol cream and clobetasol propionate creamActa Derm Venereol200182140
- TostiAPiracciniBMCameliNCalcipotriol ointment in nail psoriasis: a controlled double-blind comparison with betamethasone dipropionate and salicylic acidBr J Dermatol19981396556599892909
- NakamuraRCAbreuLdDuque-EstradaBTamlerCLeveroneAPComparison of nail lacquer clobetasol efficacy at 0.05%, 1% and 8% in nail psoriasis treatment: prospective, controlled and randomized pilot studyAn Bras Dermatol201287220321122570023
- WolfRTurEBrennerSCorticosteroid-induced “disappearing digit”J Am Acad Dermatol1990237557562229508
- RequenaLZamoraEMartinLAcroatrophy secondary to longstanding applications of topical steroidsArch Dermatol1990126101310142383026
- RigopoulosDGregoriouSKatsambasATreatment of psoriatic nails with tazarotene 0.1% versus clobetasol propionate 0.05% cream: a double-blind studyActa Derm Venereol20078716716917340027
- SaricaogluHOzATuranHNail psoriasis successfully treated with intralesional methotrexate: case reportDermatology20112225721228554
- SternDKCreaseyAAQuijijeJLebwohlMGUVA and UVB penetration of normal human cadaveric fingernail plateArch Dermatol2011147443944121173303
- FinnertyEFSuccessful treatment of psoriasis of the nailsCutis1979234344759120
- YuRCHKingCMA double-blind study of superficial radiotherapy in psoriatic nail dystrophyActa Derm Venereol199272124136
- KwangTYNeeTSSengKTA therapeutic study of nail psoriasis using electron beamsActa Derm Venereol199575907747554
- Fernández-GuarinoMHartoASánchez-RoncoMGarcía-MoralesIJaénPPulsed dye laser vs photodynamic therapy in the treatment of refractory nail psoriasis: a comparative pilot studyJ Eur Acad Dermatol Venereol200923889189519470064
- OramYKarincaoğluYKoyuncuEKaharamanFPulsed dye laser in the treatment of nail psoriasisDermatol Surg20103637738120100261
- TreewittayapoomCSingvahanontPChanprapaphKHanekeEThe effect of different pulse durations in the treatment of nail psoriasis with 595-nm pulsed dye laser: a randomized, double-blind, intrapatient left-to-right studyJ Am Acad Dermatol20126680781222243768
- HuangYCChouCLChiangYYEfficacy of pulsed dye laser plus topical tazarotene versus topical tazarotene alone in psoriatic nail disease: a single-blind, intrapatient left-to-right controlled studyLasers Surg Med20134510210723423871
- Al-MutairiNNoorTAl-HaddadASingle blinded left-to-right comparison study of excimer laser versus pulsed dye laser for treatment of nail psoriasisDermatol Ther201442197205
- LeeJYSevere 20-nail psoriasis successfully treated by low dose methotrexateDermatol Online J20091511812
- GümüşelMÖzdemirMMevlitoğluIBodurSEvaluation of the efficacy of methotrexate and cyclosporine therapies on psoriatic nails: a one-blind, randomized studyJ Eur Acad Dermatol Venereol20112591080108421118309
- SyutoTAbeMIshibuchiHSuccessful treatment of psoriatic nail with low-dose cyclosporine administrationEur J Dermatol2007173248249
- FelicianiCZampettiAForleoPNail psoriasis: combined therapy with systemic cyclosporine and topical calcipotriolJ Cutan Med Surg2004812212515129317
- Sánchez-RegañaMSola-OrtigosaJAlsina-GibertMVidal-FernándezMUmbert-MilletPNail psoriasis: a retrospective study on the effectiveness of systemic treatments (classical and biological therapy)J Eur Acad Dermatol Venereol201125557958621198950
- TostiARicottiCRomanelliPCameliNPiracciniBMEvaluation of the efficacy of acitretin therapy for nail psoriasisArch Dermatol2009145326927119289755
- MukaiMMPoffoIFWernerBBrennerFMLima FilhoJHNAPSI utilization as an evaluation method of nail psoriasis in patients using acitretinAn Bras Dermatol201287225626222570030
- ReichKNestleFOPappKEXPRESS study investigatorsInfliximab induction and maintenance therapy for moderate-to-severe psoriasis: a phase III, multicenter, double-blind trialLancet200536694941367137416226614
- van den BoschFMangerBGoupillePEffectiveness of adalimumab in treating patients with active psoriatic arthritis and predictors of good clinical responses for arthritis, skin and nail lesionsAnn Rheum Dis201069239439919815494
- ThaciDUnnebrinkKSundaramMAdalimumab for the treatment of moderate to severe psoriasis: subanalysis of effects on scalp and nails in the BELIEVE studyJ Eur Acad Dermatol VenereolIn press
- LugerTABarkerJLambertJSustained improvement in joint pain and nail symptoms with etanercept therapy in patients with moderate-to-severe psoriasisJ Eur Acad Dermatol Venereol200923889690419453794
- KavanaughAMcInnesIMeasePGolimumab, a new human tumor necrosis factor alpha antibody, administered every four weeks as a subcutaneous injection in psoriatic arthritisArthritis Rheum20096097698619333944
- VitielloMTostiAAbucharAUstekinumab for the treatment of nail psoriasis in healthy treated psoriatic patientsInt J Dermatol20135235836223330782
- RichPBourcierMSofenHPHOENIX 1 investigatorsUstekinumab improves nail disease in patients with moderate-to-severe psoriasis: results from PHOENIX 1Br J Dermatol2014170239840724117389
- de VriesACBogaardsNAHooftLInterventions for nail psoriasisCochrane Database Syst Rev20131CD007633