Abstract
Objective
In May 2022, an unprecedented Mpox outbreak was reported in several non-endemic countries with unknown epidemiological links. Since May 2022, more than 20,000 cases have been reported in Europe. Spain has been the most affected country in Europe. We aim to describe the Mpox epidemiological profile in Spain, identify its outbreak risks, and describe public health interventions implemented by the Spanish authorities.
Methods
A literature review was conducted, using specific selection criteria to obtain relevant publications describing Mpox clinical presentation and risk factors and the public health response in Spain to the ongoing outbreak.
Results
63.1% of the cases presented an anogenital rash, considered a specific and early symptom in this outbreak. Low case fatality rate is observed, mainly in risk groups, such as the immunocompromised population. Patients evolution was generally favorable, although 3–8% required hospitalization and two deaths occurred; 40% of patients were previously diagnosed with HIV infection. Most of the cases were seen among young population and concentrated in men who had sex with other men, mainly with multiple sexual partners, who did not practice safe sex such as using condoms, and those attending mass event parties.
Conclusion
To date, the Mpox outbreak is not considered a public health emergency of international concern. The epidemiological trend of the virus in Spain shows that public health response interventions (health education, contact tracing, vaccination, etc.) have adequately controlled the epidemic curve in high-risk populations and avoided spreading the virus to other groups within the community.
Introduction
Mpox virus is an orthopoxvirus with double-stranded DNA envelop, a member of the Poxviridae family, Chordopoxvirinae subfamily. It causes a viral zoonotic disease that can be transmitted from animal to human or human to human, characterized by a pustular rash. It is usually mild, and most people recover within a few weeks without specific treatment.Citation1 However, fatal cases have also been described.Citation2 It is important to highlight that the natural reservoir for the virus is still unidentified, even though rodents are suspected of playing a part in transmission.Citation3 In November 2023, WHO decided to change the name of the Monkeypox infection to Mpox to prevent any stigma or discrimination. This study will use the new synonym Mpox for this disease.Citation4
The virus was first discovered in a Danish laboratory in 1958 after an outbreak of skin rashes among captive monkeys.Citation3 In 1970, the first case in humans was detected in a child in the Democratic Republic of Congo.Citation5 Until May of 2022, the Mpox virus had historically caused outbreaks in remote populations in West and Central Africa, often in forested areas where wild animal hunting was common. In 2003, the first outbreak outside of Africa was recorded in the United States, with a total of 11 people infected, the cause of the outbreak was traced to three species of African rodents imported from Ghana into North America. These rodents were housed with prairie dogs, which subsequently became infected. The last outbreaks in Africa were reported in 2017 and 2018 in Nigeria and Cameroon, where the virus had not been reported for the previous 20 years. Following the announcement of these outbreaks, the WHO admitted that endemic Mpox had been reported from more countries in the last 10 years than during the previous 40 years. From September 2018 to May 2022, more cases were recorded outside of Africa: one in Israel, one in Singapore, five in the United Kingdom, and two in the United States, and all of them were travel-related. Therefore, there is an increasing concern about the virus’s new epidemiological behavior and its becoming an outbreak hazard for global health.Citation3
In May 2022, an unprecedented outbreak of Mpox infection with no known epidemiological links was reported in several non-endemic countries. The first case of Mpox was reported in Spain on the 18th of April 2022 in Madrid.Citation2 On the 23rd of July 2022 the General Director of the World Health Organization (WHO) declared the Mpox outbreak a public health emergency of international concern (ESPII). From May 2022 to January 2023, around 20,000 cases have been reported all around Europe; Spain has declared 7499 cases, becoming the most affected country in Europe.Citation2 Based on this new scenario, Mpox has been identified as an important hazard to global health. This literature review aims to describe the epidemiological profile of Mpox in Spain, identify the Mpox outbreak risk, and explore the public health interventions implemented by the Spanish authorities.
Methodology
Search Strategy and Selection Criteria
Initial searches were conducted on PubMed using the keywords “Mpox” or “Monkeypox” and “Spain” in articles published between May 2022 and November 2023. Articles were subjected to a preliminary screening based on title relevance, followed by a review of the abstract or full text to determine final inclusion. Additional sources were manually sourced through reference lists of relevant reports. Reports from the Spanish Epidemiological Surveillance Network (RENAVE) and Sistema para la Vigilancia en España (SiViEs) platform were given special attention. Inclusion criteria extended to articles addressing the epidemiological, clinical, or public health response characteristics of Mpox or Monkeypox in Spain.
Inclusion Criteria
Publication Source: Scientific articles published on PubMed containing the keywords ”Mpox” or ”Monkeypox” and ”Spain.”
Content Focus: Articles addressing the epidemiological, clinical, or public health response characteristics of Mpox in Spain.
Language: Articles in both English and Spanish.
Publication Time Frame: Articles published between May 2022 and November 2023.
Exclusion Criteria
Content focus: Exclusion of Articles not addressing the epidemiological, clinical, or public health response characteristics of Mpox in Spain.
Language: Exclusion of articles not in English or Spanish.
Publication Time Frame: Exclusion of articles published outside the specified period (before May 2022)
Results
A total of 38 reports were included in the literature review: 30 articles and seven relevant international sources. Our PubMed search found nine reports, and all of them are included in our literature review. In addition, we decided to include our review with other reports and scientific articles manually sourced; also, the reference lists of all the studies were screened to identify other studies that could eventually fit our inclusion criteria. In total, 30 reports and 8 relevant national and international sources were included. shows the most relevant reports reviewed for this work, presented in the PICO format.
Table 1 Describe the PICO of the Most Relevant Published Articles Included in the Review
The review of reported cases of Mpox in Spain from May 2022 to November 2023 has yielded significant findings that can be summarized. These observations provide valuable insights into the current status and potential trends of Mpox in the region.
In 63.1% of the Spanish patients, a rash was in the anogenital area, the most frequent clinical sign observed after general/unspecific symptoms, such as fever and asthenia, to name a few.Citation2 Between sexes, this anogenital rash was present in 71.2% of the men but only in 51% of the women.Citation12 This anogenital rash is a specific and early sign of Mpox infection (the median number of days between the date of first symptom onset and the date rash of onset was 0 days).Citation2 The clinical presentation of current Mpox cases differs from the results of African patients before 2022. Historically, lesions have predominantly affected the face, palms and soles, mucous membranes, and, less commonly, genitals.Citation21 This outbreak is more associated with the anogenital rash.Citation2 A generally mild character of the infection with a very low case-fatality rate (concentrated only in risk groups) is confirmed;Citation2 a significant difference in mortality is observed between the affected patients before 2022 and the current outbreak, despite around 8% of the cases developing different complications.Citation2 40.3% of the Spanish reported cases were previously diagnosed with HIV infection, becoming the most frequent associated comorbidity.Citation2 The primary transmission mode for this infection is through close contact, typically through sexual intercourse, but not exclusively so.Citation22 Epidemiological surveillance conducted in Spain has revealed that the outbreak of Mpox is mainly under control.Citation2 However, the transmission of the virus appears to be concentrated within a specific group of individuals, namely men who have sex with other men. Among this group, those who engage in condomless sex with multiple partners and frequently attend sexual parties appear at increased risk of Mpox transmission.Citation6 The control strategy for the outbreak in Spain, limited to vaccination and contact tracing, was shown to be sufficient both to control the epidemic curve in men who have sex with other men and to avoid spreading the disease to other groups.Citation14
Discussion
Spain: Political, Administrative, and Socio-Demographic Features
Spain is one of the largest countries in Western Europe, with an extent of 505955km2 and a population of 47650000 in 2022. It is part of the Iberian Peninsula, together with Portugal. The Spanish territory is organized into 17 Autonomous Communities (including the Canary and the Balearic Islands and two Autonomous Cities, Ceuta, and Melilla, placed at the very north of the African continent) that conform to a quasi-federal state, where all the regions play a very active role in the provision of the welfare of state service, including health services.
The population tends to concentrate in big cities, such as Madrid (the capital) or Barcelona, and on the coastline. On the contrary, the rest of the country is mainly inhabited due to a depopulation process that occurred in the last century. The average life expectancy was 82.2 years (79.6 in men and 85.1 in women) in 2021.Citation23 The fertility rate is one of the lowest in the world, with 1.3 births per woman in 2021.Citation23 Subsequently, a constrictive population pyramid represents this aging population (around 20% of the population is over 65). In addition, the most prevalent diseases seen in Spain are chronic disease and its morbidity. However, since 2020, emerging diseases like Covid-19 have been game-changers. The ongoing outbreak of the Mpox virus, introduced in the country for the first time in April 2022, is a clear example of this present outbreak hazard.Citation23
The Spanish Public Health Actors on the National Health System
Spain’s National Health System is based on the principles of universality, free access, equity, and fairness of financing. Service delivery is organized at the regional level and supervised by the Ministry of Health.Citation24 Public health policy is also transferred to the regions, even though it is coordinated by an organization called Consejo Interterritorial de Salud with the advice of the National Epidemiology Center and its national surveillance system (RENAVE), a center for the coordination of the alerts and the public health emergencies (CAES) was also created in 2004. Despite being a strong system, it has been affected by different factors such as the Spanish financial crisis that occurred last decade (responsible for a contraction of the health budget), and more recently, the big effort made to fight against Covid-19 pandemic. In addition, Primary Care Attention, which used to be the center of the health system, struggles with the public health crisis due to a shortage of qualified professionals and inefficient health management. To reduce Spain's vulnerability against new epidemic hazards and prepare for future threats, a National Public Health Agency is expected to be founded in the following years.Citation25
Virological Characteristics of Mpox Virus
The Mpox virus is an enveloped double-stranded DNA virus of the orthopoxvirus genus in the Poxviridae family. Historically, two clades of Mpox have been described: Clade 1, also known as clade Congo-Basin, endemic to Central Africa with a high mortality rate (around 10%), and Clade 2 or West African Clade (now named Clade 2a), characterized by a 95% nucleotide sequence similarity with Clade 1 but presenting a considerably lower mortality rate (around 1–3%).Citation7 In addition, phylogenetic characteristics of the virus, which have been analyzed in different samples of patients during this current outbreak in Europe, describe a new subvariant of Clade 2, denominated 2b, which is genetically similar to Clade 2a but much less virulent.Citation20 Finally, it is worth noting that transmission of the virus was initially believed to be primarily zoonotic and only limited between humans in Clades 1 and 2a. However, the 2b Clade has been shown to have significant transmission between humans.Citation20 Initially, the belief was that monkeypox, classified as a DNA virus, with an assumed higher efficiency in detecting and correcting mutations compared to RNA viruses like SARS-CoV-2, would be less susceptible to rapid mutations. However, the virus had demonstrated a prolonged presence in Europe, exceeding the initially estimated timeframe. This observation indicates an ongoing acquisition of mutations, challenging the initial assumption of lower mutational dynamics.Citation26 Mpox virus exemplifies the delicate interplay between zoonotic spillover and anthropogenic factors, constituting a prime example of the global epidemic potential.Citation27
Mpox Outbreak in Spain
A comprehensive epidemiological surveillance work has been done by the National Epidemiology Surveillance Network (RENAVE) since the beginning of the outbreak. Between April 18, 2022, and November 6, 2023, the SiViEs platform has accurately documented a total of 7647 confirmed positive cases in the country. The majority of these cases occurred between May 2022 and December 2022, with approximately 1500 cases reported during that year. In contrast, during the current year of 2023, up to November 6, only 127 cases have been recorded. Therefore, the highest concentration of cases was observed during the epidemic outbreak in the second half of 2022, and the epidemiological situation has remained contained thus far.
In Spain, every reported case was confirmed by PCR or sequencing samples from skin lesions, vesicular fluids, oropharyngeal, genital, or recto-anal exudates. Despite the initial use of generic PCR for orthopoxviruses in some centers,Citation28 a real-time quantitative PCR was specifically designed and assessed across numerous patient samples within the majority of Spanish reference centres. Surveillance is passive, nationwide, and case-based; with laboratory information integrated, information flows from the regional to the national level. This system provides an invaluable amount of data for the analysis of the outbreak.
Demographic Features and Geographic Distribution
From April 2022 to January 2023, a total of 7499 cases were registered in Spain; 7333 corresponded to men, and 166 were women. The age range varies between 7 months and 88 years, with an average age of 37 years (interquartile range: 31–44 years). In 66.7% of the cases, patients were between 30 and 49 years old. Of the patients, 43.9% (3.295 cases) were born in Spain. Madrid (33.8%) and Catalonia (30.8%) declared more than 60% of the total cases in the country.Citation2
Clinical Features
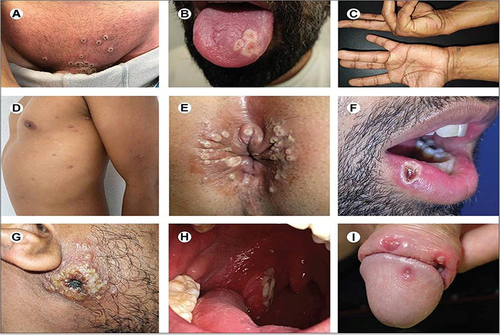
A total of 5386 cases (71.8%) presented some general symptomatology: fever, asthenia, sore throat, muscle pain, or headache, with fever being the most frequent general symptom (56.8%).Citation2 The specific symptomatology recorded was the rash located in the anogenital area, which was present in 63.1% of the cases, being the most frequent clinical sign observed in menCitation2,Citation6, as long as the anogenital rash was present in 71.2% of the men but only on the 51% of the women.Citation12 The median number of days between the first symptom onset and the rash of onset was 0 days.Citation2 Examples of the clinical presentation of anogenital rash and other rashes in Spanish patients are shown in .Citation8
Figure 1 Clinical presentation of confirmed human mpox virus cases in Spain, adapted from Tarin-Vicente et al, with permission of the authorCitation8 (A) Pustules in the genital and pubic area, initially umbilicated, now with necrotic crusts and a central dip. (B) Three merging pustular lesions with indented centers on the left side of the tongue’s top surface. (C) Small, hard vesicles on the thick skin of the palms. (D) Mixed group of bumps, pustules, and indented pustules with redness around them on the side of the chest and left arm. (E) Pustules arranged in a circle around the anus and nearby skin. (F) A pustular lesion with a crusted center on the inside part of the lower lip near the right corner of the mouth. (G) Initial infection site with a large, crusted sore on the right cheek. (H) The right tonsil at the back of the throat is red, swollen, and has a covered ulcer. (I) Various-sized lesions in different stages on the head and covering of the penis, with swelling around the larger sore.
Associated Complications and Comorbidities with Mpox Infection
A total of 510 (8.7%) had complications throughout their clinical process. The most common were the secondary bacterial infections of skin lesions and ulcers. Overall, 7% of the patients were hospitalized between the 5th of May and the 21st of November. The average age of hospitalized cases was 36 years, most were male (240 cases), and six were female. Six male cases were hospitalized in the ICU (in one of them, the ICU admission was not related to monkeypox). Among these cases, one case had a diagnosis of mild myocarditis with two days of observation in ICU, three cases with a diagnosis of meningoencephalitis, one case with various complications arising from disseminated Mpox infection, and one person with other pathologies and concomitant infection with Mpox. Of the diagnosed cases of meningoencephalitis, two patients, one with disseminated infection and another with concomitant infection of Mpox and other pathologies, have unfortunately passed away, resulting in a notably low casefatality rate of less than 0.5%. Interestingly, of the 6751 reported cases, 2721 individuals (40.3%) were diagnosed with HIV infection.Citation2 Coinfection with sexual transmission diseases (apart from HIV) was not registered on SIVIEs. However, other Spanish studies suggest that between 20%Citation19 and 25%Citation11 of the cases were coinfected by any other sexual transmission disease, often un-diagnosed, such as gonorrhoea, Chlamydia infection, and syphilis.Citation15
Features of Mpox Exposure
Of the 7499 cases, 5607 (74.8%) had information on the most likely transmission mechanism. Of these, in 4618 cases (82.4%), transmission was attributed to close contact in the context of sexual intercourse, in 350 cases (6.2%) to non-sexual close contact (including cases in children), 2 cases to occupational exposure in a health-care setting, in 31 cases not specified (0.6%), and in the remaining 606 (10.8%) this information is not described. In relation to attendance at mass events, of the 5846 cases with information on this variable, 1010 (17.3%) attended an event on the dates prior to the onset of symptoms.Citation2,Citation9
Out of the 6446 reported cases with information on a history of international travel in the 21 days before symptom onset, 963 (14.9%) had traveled. Travel destination was available for 60 of them (29 cases to Portugal, 12 cases to the United States, 12 cases to the Netherlands, 5 cases to Cuba, and 2 cases to Canada). One hundred and seventy-seven cases have been classified as imported cases. A total of 5607 cases of the 7499 cases analyzed (74.8%) were men who had had sex with men, 164 cases were heterosexual men (2.2%), 86 cases were heterosexual women (1.1%), 4 cases were bisexual women (0.1%), and 1638 cases (21.8%) had no information available. Excluding cases with no information, these percentages were 95.7%, 2.8%, 1.5%, and 0.1%, respectively.Citation2 These findings support sexual contact as the main route of transmission of the disease.Citation29
Laboratory Tests
The detection of Mpox can be achieved through various diagnostic methods, including cell culture, polymerase chain reaction (PCR), enzyme-linked immunosorbent assay (ELISA), immunohistochemistry, electron microscope, Western blot analysis and sequencing.Citation30 However, PCR has been recommended for a confirmatory and definitive test.Citation31 Samples can be taken for any lesion skin lesion material or alternative specimens like oral or nasopharyngeal swabs. Importantly, it is emphasized that PCR conducted on blood samples is not diagnostically sufficient and should not serve as a standalone first-line diagnostic tool.
When the outbreak began, timely and accurate diagnosis became imperative, posing a significant challenge for microbiology services. In Spain, despite the initial use of generic PCR for Orthopoxviruses in some hospitals,Citation28 a real-time quantitative PCR was specifically designed and assessed across numerous patient samples within the majority of Spanish reference centres. The results underwent meticulous comparison with isolation outcomes, and these diagnostic tests were made accessible from June 2022.Citation32
Treatment
For most patients with an active infection of Mpox with an intact immune system, no specific treatment is needed. However, supportive care (including specific skin care information) and pain control should be implemented early on the first contact with health care. Complications must be treated individually, assessing each case. Some patients are at risk of developing severe diseases, such as those who are immunocompromised due to conditions such as advanced or poorly controlled human immunodeficiency virus (HIV), leukemia, lymphoma, generalized malignancy, or solid organ transplantation. Also, infants (younger than one year old), pregnant women, and patients with chronic conditions that affect skin integrity are at risk.Citation30
No specific treatment has been shown to be completely effective for severe Mpox disease.Citation10 However, Tecovirimat has documented efficacy in a small series of cases, becoming the only antiviral approved by the European Medicines Agency for the treatment of severe Mpox.Citation13
Control Strategies
Vaccination
The cessation of smallpox vaccination after the eradication of the disease in 1980 may be a contributing factor to the current outbreak, particularly in conjunction with the rising trend of global mobility. This historical perspective highlights the potential impact of halting vaccination efforts on disease control.Citation13 In Spain, the available vaccines, including both MVA-BN (Modified Vaccinia Ankara) vaccines, represent a significant advancement in immunization. However, it's noteworthy that the field of vaccine development has seen a transformative shift with the emergence of mRNA technology. This innovative platform has become a driving force in the rapid creation of vaccines, particularly in response to newly identified pathogens.Citation33 We anticipate promising outcomes in the near future based on ongoing developments.
Vaccination against Mpox in Spain was authorized by the National Commission for Public Health on the 9th of June of 2022.Citation34 Two brands of the same vaccine are available in the country: Jynneos and Imvanex. Both are Modified Vaccinia Ankara (MVA-BN). Their efficacy in preventing the disease is well demonstrated.Citation35 However, the duration of the protection is still unknown.Citation36
On the first recommendation in June 2022, the National Commission only authorized the use of post-exposure prophylaxis (recommended after close contact with a confirmed case). In July and August of 2022, this organization approved the use of the vaccine under two circumstances: pre- and post-exposure prophylaxis. However, pre-exposure use was restricted to young men (under 45) with risky sexual behavior.Citation34 Also, due to the limited stock and the peak demand, the European Medicines Agency (EMA) authorized the injection of fractionated vaccine doses.Citation35
Until December 2022, around 25,000 doses of vaccines had been administered in Spain, both fractionated and full doses.Citation2 Many doses were administered to risk groups in terms of pre-exposition prophylaxis. From the overall positive cases of Mpox in the country, 55 cases had been vaccinated in the context of the outbreak, with an average of 5 days elapsing between the date of vaccination and the onset of symptoms. Also, 471 positive cases had received smallpox vaccination at least once, most of these patients were Spanish and Latin American.Citation2
On the 7th of December 2022, the latest recommendation to date was given by the National Commission of Public Health,Citation15 two different criteria for receiving the vaccine are described:Citation34
Pre-Exposure Prophylaxis
Vaccination is recommended for people with risky sexual behavior, including but not only gays, bisexuals, and men who have sex with other men. Health workers exposed to the virus are also included. A recent Spanish cohort study has demonstrated the efficacy of MVA-BN vaccination for Mpox in a high-risk population. A single dose of the MVA-BN vaccine is shown to reduce the risk of Mpox infection by 65% starting from 7 days post-vaccination, and this risk reduction increases to 79% from 14 days post-vaccinationCitation17. These findings confirm that MVA-BN vaccination functions as an effective preventive measure in a high-risk population for Mpox infection, particularly in the early period following vaccine administration. Due to the pre-exposure vaccination campaign aligning with the decline in monkeypox incidence in Spain and the subsequent low incidence, the effectiveness over extended periods post-vaccination could not be assessed.Citation17
Post-Exposure Prophylaxis
Post-exposure prophylaxis is a well-established strategy for preventing infectious diseases. Prophylaxis using smallpox vaccines continues to be accessible from the strategic national stockpile for eligible individuals who have been exposed.Citation37 The vaccine is now recommended for anyone in close contact with a confirmed case who has not had the disease or previous vaccination. It must be administered within the first 4 days after close contact, with a maximum window of 14 days after contact. Vaccination must be prioritized in risk groups: immunocompromised patients (including HIV-positive patients with less than 200 CD4), pregnant women, children, and health workers. A prospective cohort study of close contacts of Mpox cases had proved that the post-exposure vaccine effectiveness was 93.6% (95% CI: 72.1–98.5) for non-cohabitants and 88.6% (95% CI: 66.1–96.2) for cohabitants. These findings suggest a significant level of protection provided by the vaccine, particularly in preventing illness among close contacts in both general and intimate living arrangements during the observed outbreak in Spain.Citation16
Isolation
In individuals with mild monkeypox disease with a competent immune system, an assessment based solely on PCR data might recommend a contact isolation period of 3 to 6 weeks. However, in cases of mild monkeypox in immunocompetent patients, the duration of isolation and the need for specific post-recovery precautions can be adjusted based on the understanding of viral dynamics and patient’s clinical improvement. Understanding this knowledge gap could lead to more targeted and efficient public health future recommendations for individuals recovering from mild mpox.Citation18
Public Health Surveillance
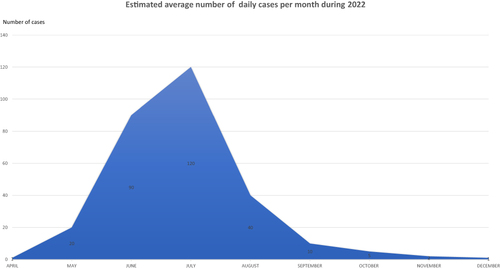
On the 20th of October 2022, the World Health Organization recognized that notable achievements had been made against halting the spread of Mpox disease. To date, the Mpox outbreak is no longer considered a public health emergency of international concern. In Spain, comprehensive epidemiological surveillance work was done by the National Epidemiology Surveillance Network (RENAVE) since the beginning of the outbreak. Between April 18, 2022, and November 6, 2023, the SiViEs platform has accurately documented a total of 7647 confirmed positive cases in the country. The majority of these cases occurred between May 2022 and December 2022, with approximately 1500 cases reported during that year. In contrast, during the current year of 2023, up to November, only 127 cases have been recorded. Therefore, the highest concentration of cases was observed during the epidemic outbreak in the second half of the year 2022, and the epidemiological situation has remained contained thus far. In , we can observe how the epidemic curve peaked July 2022, when more than 100 cases were detected daily. After this peak, a progressive and sustained reduction is observed. During December 2022, less than 20 cases were notified in Spain, concentrated only in six regions.Citation2
Figure 2 Estimation of the daily cases per month of Mpox in Spain during 2022.
Environmental Surveillance
Mpox DNA virus has been identified in wastewater samples from various regions of Spain, even during the early stages of reported clinical cases in those areas. Notably, the detection of viral DNA in wastewater showed a rapid increase, providing an early indication of the subsequent rise in officially reported cases. This underscores the effectiveness of Wastewater-Based Epidemiology (WBE) as a sensitive and cost-effective strategy for monitoring emerging viral threats, particularly in scenarios where issues such as stigma and blame could undermine the ability to respond effectively during outbreaks.Citation38
Recommendations
Based on our literature review, we would like to suggest some recommendations that could be useful to respond against Mpox:
In the context of the outbreak, any anogenital rash after sexual intercourse should be tested for the Mpox virus. PCR samples from recto-anal exudates should be sequenced, especially in men.
Tests for HIV must be offered to all suspected and confirmed cases; screening for other STDs is also highly recommended.
Active epidemiological surveillance must be undertaken in the group of men who have sex with other men and those who attend sexual parties, promoting health education, early testing, contact tracing, and a strong vaccination campaign to reach the highest possible percentage of at-risk individuals fully vaccinated as soon as possible. Furthermore, Wastewater-Based Epidemiology should be considered as a sensitive and cost-effective strategy for monitoring emerging viral threats.
Although our data show that Mpox cases are more prevalent among the MSM community, this finding should not be utilized to discriminate or stigmatize this community. Instead, focus should be placed on prevention, sexual education, and vaccination.
Research in Context
Evidence Before This Study
The epidemiological trends of human monkeypox infection are swiftly shifting from endemic regions to non-endemic countries, becoming a re-emerging public health threat. The outbreak is concentrated among men who have sex with other men. An anogenital rash was present in many cases, and although monkeypox has not been proven to be a sexually transmitted disease, many cases showed a connection with sexually transmitted diseases, such as HIV.
Added Value of This Study
Effective preventive and control strategies rely on a good understanding of disease burden, transmission, and management, which are the objectives of this study.
Implications of All the Available Evidence
Following this study, our aim is to maintain active epidemiological surveillance among men who have sex with other men and those who attend sexual parties. This includes promoting health education, early testing, and contact tracing and implementing a strong vaccination campaign to ensure a high percentage of at-risk individuals are fully vaccinated as soon as possible. Additionally, considering the characteristics of the outbreak, the risk of general transmission among the entire population seems to be low.
Conclusion
On May 11, 2023, the Emergency Committee on Mpox met and advised that the multi-country outbreak is no longer a Public Health Emergency of International Concern (PHEIC) due to the sustained decline in cases. The Committee’s advice was accepted by the WHO Director-General.
The epidemiological trend of the virus in Spain and the rest of the world indicates that the public health response, which included health education, contact tracing, and vaccination, has effectively controlled the epidemic curve among high-risk populations and prevented the spread of the virus to other groups within the community. This success should be showcased as an example of effective intervention in outbreak control.
Disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Funding
References
- Homepage/Website. WHO Mpox (monkeypox) outbreak; 2022. Avalaible from: https://www.who.int/emergencies/situations/monkeypox-oubreak-2022. Accessed January 25, 2024.
- Homepage/Website. Situacion Epidemiologica De Los Casos De Viruela Del Mono-03012023.pdf. Avalaible from: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/archivos%20A-Z/MPOX/SITUACION%20EPIDEMIOLOGICA%20DE%20LOS%20CASOS%20DE%20VIRUELA%20DEL%20MONO-03012023.pdf. Accessed January 25, 2024.
- Ihekweazu C, Yinka-Ogunleye A, Lule S, Ibrahim A. Importance of epidemiological research of monkeypox: is incidence increasing? Expert Rev Anti Infect Ther. 2020;18(5):389–392. doi:10.1080/14787210.2020.1735361
- Homepage/Website. WHO recommends new name for monkeypox disease. Avalaible from: https://www.who.int/news/item/28-11-2022-who-recommends-new-name-for-monkeypox-disease. Accessed January 25, 2024.
- Meo SA, Jawaid SA. Human monkeypox: fifty-two years based analysis and updates. Pak J Med Sci. 2022;38(6):1416–1419. doi:10.12669/pjms.38.6.6775
- Iñigo Martínez J, Gil Montalbán E, Jiménez Bueno S, et al. Monkeypox outbreak predominantly affecting men who have sex with men, Madrid, Spain, 26 April to 16 June 2022. Eurosurveillance. 2022;27:27. doi:10.2807/1560-7917.ES.2022.27.27.2200471
- Ferdous J, Barek M, Hossen M, Bhowmik KK, Islam MS. A review on monkeypox virus outbreak: new challenge for world. Health Sci Rep. 2022;6(1):e1007. doi:10.1002/hsr2.1007
- Tarín-Vicente EJ, Alemany A, Agud-Dios M, et al. Clinical presentation and virological assessment of confirmed human monkeypox virus cases in Spain: a prospective observational cohort study. Lancet Lond Engl. 2022;400(10353):661–669. doi:10.1016/S0140-6736(22)01436-2
- Girometti N, Byrne R, Bracchi M, et al. Demographic and clinical characteristics of confirmed human monkeypox virus cases in individuals attending a sexual health centre in London, UK: an observational analysis. Lancet Infect Dis. 2022;22(9):1321–1328. doi:10.1016/S1473-3099(22)00411-X
- Patauner F, Gallo R, Durante-Mangoni E. Monkeypox infection: an update for the practicing physician. Eur J Intern Med. 2022;104:1–6. doi:10.1016/j.ejim.2022.08.022
- Núñez-Cortés R, Calatayud J, López-Gil JF, Koyanagi A, Casaña J, López-Bueno R. Risk profile and mode of transmission of Mpox: a rapid review and individual patient data meta-analysis of case studies. Rev Med Virol. 2023;33(2):e2410. doi:10.1002/rmv.2410
- Vallejo-Plaza A, Rodríguez-Cabrera F, Hernando Sebastián V, et al. Mpox (formerly monkeypox) in women: epidemiological features and clinical characteristics of mpox cases in Spain, April to November 2022. Eurosurveillance. 2022;27(48):2200867. doi:10.2807/1560-7917.ES.2022.27.48.2200867
- Ena J, Wenzel RP. The rise and fall of mpox. Rev Clínica Esp Engl Ed. 2023;223(1):60–61.
- Guarducci G, Porchia BR, Lorenzini C, Nante N. Overview of case definitions and contact tracing indications in the 2022 monkeypox outbreak. Infez Med. 2022;31(1):13–19. doi:10.53854/liim-3101-3
- Cobos A, Valerio M, Palomo M, et al. Demographic, clinical and microbiological characteristics of the first 30 human monkeypox confirmed cases attended in a tertiary hospital in Madrid (Spain), during the May-June 2022 international outbreak. Rev Esp Quimioter. 2023;36(2):194. doi:10.37201/req/112.2022
- Montero Morales L, Barbas Del Buey JF, Alonso García M, et al. Post-exposure vaccine effectiveness and contact management in the mpox outbreak, Madrid, Spain, May to August 2022. Eurosurveillance. 2023;28(24):2200883. doi:10.2807/1560-7917.ES.2023.28.24.2200883
- Fontán-Vela M, Hernando V, Olmedo C, et al. Effectiveness of MVA-BN vaccination in a population at high-risk of mpox: a Spanish cohort study. Clin Infect Dis;2023. ciad645. doi:10.1093/cid/ciad645
- Suñer C, Ubals M, Tarín-Vicente EJ, et al. Viral dynamics in patients with monkeypox infection: a prospective cohort study in Spain. Lancet Infect Dis. 2023;23(4):445–453. doi:10.1016/S1473-3099(22)00794-0
- Maldonado-Barrueco A, Sanz-González C, Gutiérrez-Arroyo A, et al. Sexually transmitted infections and clinical features in monkeypox (mpox) patients in Madrid, Spain. Travel Med Infect Dis. 2023;52:102544. doi:10.1016/j.tmaid.2023.102544
- Americo JL, Earl PL, Moss B. Virulence differences of mpox (monkeypox) virus clades I, IIa, and IIb.1 in a small animal model. Proc Natl Acad Sci U S A. 2023;120(8):e2220415120. doi:10.1073/pnas.2220415120
- Yinka-Ogunleye A, Aruna O, Dalhat M, et al. Outbreak of human monkeypox in Nigeria in 2017–18: a clinical and epidemiological report. Lancet Infect Dis. 2019;19(8):872–879. doi:10.1016/S1473-3099(19)30294-4
- Thornhill JP, Barkati S, Walmsley S, et al. Monkeypox Virus Infection in Humans across 16 Countries — April–June 2022. N Engl J Med. 2022;387(8):679–691. doi:10.1056/NEJMoa2207323
- Homepage/Website. INEbase / Demography and population /Demographic phenomena /Basic Demographic Indicators / Latest data INE. Avalaible from: https://www.ine.es/dyngs/INEbase/en/operacion.htm?c=Estadistica_C&cid=1254736177003&menu=ultiDatos&idp=1254735573002. Accessed January 25, 2024.
- Bernal-Delgado E, Garcia-Armesto S, Oliva J, et al. Spain: health system review. Health Syst Transit. 2018;20(2):1–179.
- Homepage/Website. EstrategiaVigilanciaSaludPublica. Avalaible from: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/vigilanSP/doc/estrategiaVigilanciaSaludPublica.pdf. Accessed January 25, 2024.
- Sharma A, Fahrni ML, Choudhary OP, Choudhary OP. Monkeypox outbreak: new zoonotic alert after the COVID-19 pandemic. Int J Surg Lond Engl. 2022;104:106812. doi:10.1016/j.ijsu.2022.106812
- Saied AA, Metwally AA, Choudhary OP, Choudhary OP. Monkeypox: an extra burden on global health. Int J Surg Lond Engl. 2022;104:106745. doi:10.1016/j.ijsu.2022.106745
- Panag DS, Jain N, Katagi D, et al. Variations in national surveillance reporting for Mpox virus: a comparative analysis in 32 countries. Front Public Health. 2023;11:1178654. doi:10.3389/fpubh.2023.1178654
- Grau Echevarría A, Peñuelas Leal R, Martínez Domenech Á, et al. Clinical and demographic features of 49 patients with human monkeypox virus–confirmed infection in a tertiary care center in Valencia, Spain: a descriptive study. Sex Transm Dis. 2023;50(2):66. doi:10.1097/OLQ.0000000000001734
- Homepage/Website. Clinical management and infection prevention and control for monkeypox: interim rapid response guidance; 2022: Avalaible from https://www.who.int/publications-detail-redirect/WHO-MPX-Clinical-and-IPC-2022.1. Accessed January 25, 2024.
- Li Y, Olson VA, Laue T, Laker MT, Damon IK. Detection of monkeypox virus with real-time PCR assays. J Clin Virol off Publ Pan Am Soc Clin Viro. 2006;36(3):194–203. doi:10.1016/j.jcv.2006.03.012
- Álvarez Argüelles ME, Martínez ZP, Alba SR, et al. Detecting, quantifying, and isolating monkeypox virus in suspected cases, Spain. Emerg Infect Dis. 2023;29(7):1465–1469. doi:10.3201/eid2907.221229
- Chopra H, Choudhary OP, Choudhary OP. mRNA vaccines as an armor to combat the infectious diseases. Travel Med Infect Dis. 2023;52:102550. doi:10.1016/j.tmaid.2023.102550
- Homepage/Website. Estrategia_vacunacion_Monkeypox_07122022. Avalaible from: https://www.sanidad.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/MonkeyPox/docs/Estrategia_vacunacion_Monkeypox_07122022.pdf. Accessed January 25, 2024.
- Wilck MB, Seaman MS, Baden LR, et al. Safety and immunogenicity of modified vaccinia ankara (ACAM3000): effect of dose and route of administration. J Infect Dis. 2010;201(9):1361–1370. doi:10.1086/651561
- Homepage/Website. CDC. Mpox in the U.S. Centers for Disease Control and Prevention; 2022. Avalaible from: https://www.cdc.gov/poxvirus/mpox/interim-considerations/jynneos-vaccine.html. Accessed January 25, 2024.
- Fahrni ML, Sharma A, Choudhary OP, Choudhary OP. Monkeypox: prioritizing public health through early intervention and treatment. Int J Surg Lond Engl. 2022;104:106774. doi:10.1016/j.ijsu.2022.106774
- Girón-Guzmán I, Díaz-Reolid A, Truchado P, et al. Spanish wastewater reveals the current spread of Monkeypox virus. Water Res. 2023;231:119621. doi:10.1016/j.watres.2023.119621
