Abstract
Purpose
This research aims to investigate the role of management leadership in promoting a culture of patient safety within healthcare organizations. Through a comprehensive mediation analysis of the Chinese version of the safety attitudes questionnaire (CSAQ) and patient safety culture, the study examines the interplay between these critical factors and their combined influence on healthcare outcomes.
Patients and Methods
In a medical center located in Taiwan, a cross-sectional survey was carried out utilizing the CSAQ. Among the 1500 distributed surveys, 1037 were returned and deemed valid, resulting in a return rate of 69.13%. To investigate the main measures, Structural Equation Modeling with mediation analysis was employed to scrutinize the direct and indirect effects of factors including teamwork climate, job satisfaction, stress recognition, perceptions of management, working conditions, and emotional exhaustion on safety climate.
Results
The findings reveal that effective management leadership plays a pivotal role in shaping safety attitudes and fostering a robust patient safety culture. The study identifies three critical facets of patient safety that are entirely mediated by management perceptions: teamwork climate, working conditions, and stress recognition. The results highlight the importance of enhancing these dimensions to advance the patient safety culture within healthcare organizations. Moreover, stress recognition is identified as a critical factor influencing the organizational culture of patient safety.
Conclusion
This research offers valuable insights for healthcare organizations seeking to prioritize patient safety and improve overall quality of care. By enhancing our understanding of the critical factors that shape safety attitudes and patient safety culture, this study provides a roadmap for effective management leadership and a culture of patient safety within healthcare organizations. The study underscores the significance of management leadership in promoting patient safety culture and highlights the importance of enhancing teamwork climate, working conditions, and stress recognition to advance patient safety culture.
Introduction
In 2002, the issue of patient safety was initially deliberated during the World Health Assembly. As per the World Health Organization’s annual report, one in ten hospitalized patients faces medication-related harm stemming from adverse events. These events occur at rates ranging from 3.7% to 17% in different countries. In Australia, for instance, adverse events were associated with 10.1% of hospital admissions. In Portuguese acute care hospitals, 11.1% of adverse events occurred, with 53.2% being preventable.Citation1–4 Research indicates that many patients are subjected to harm during medical procedures, leading to permanent injury, death, or infections.Citation5–7 As a result, numerous initiatives have been undertaken on a global scale to prioritize safety considerations within healthcare organizations.
In 2006, the European Network for Patient Safety (EUNetPaS) defined the concept of patient safety culture as
An integrated pattern of individual and organizational behavior, based upon shared beliefs and values that continuously seeks to minimize patient harm, which may result from the processes of care delivery.Citation8
To put it another way, the patient safety culture within healthcare organizations serves as a barometer of hospital management’s dedication to patient safety and delivering high-quality medical care. As such, regularly evaluating the safety culture within these organizations is imperative for the continuous improvement of patient safety.Citation9,Citation10
The Safety Attitudes Questionnaire (SAQ) is a frequently employed tool for assessing medical staff’s perspectives on patient safety culture.Citation11–13 The original SAQ (refer to the Sexton et al’s SAQ), created by Sexton et al,Citation14 encompasses six dimensions of patient safety culture: teamwork climate, safety climate, perceptions of management, job satisfaction, stress recognition, and working conditions. In 2007, the Joint Commission of Taiwan (JCT) took the initiative to create a Chinese version of the Safety Attitudes Questionnaire (CSAQ) using forward and backward translation methods. This was done to more accurately evaluate the patient safety culture within Taiwan’s healthcare sector.Citation15 In 2014, building upon the original Chinese version of the SAQ (CSAQ) developed in 2007, the JCT introduced two additional dimensions - emotional exhaustion and work-life balance - with the aim of enhancing the comprehensiveness of the CSAQ assessment.Citation16–20 These new dimensions are specifically designed to capture medical staff’s viewpoints regarding fatigue and work-life conditions.
Many applications of the CSAQ have also proposed important dimensions related to enhancing patient safety culture. For example, Huang et alCitation16 stated that teamwork climate, perceptions of management, and emotional exhaustion were important components contributing to better patient safety. Additionally, nurses reported higher levels of stress and challenges compared to physicians, likely due to the multitasking work conditions in hospitals. Lee et alCitation18 indicated that different demographic variables, such as gender, age, and job experience, influenced patient safety culture. Male employees showed higher satisfaction in safety climate, job satisfaction, and working conditions, while female employees demonstrated higher stress recognition. Employees in managerial positions perceived better teamwork climate, safety climate, and job satisfaction. Lee et alCitation20 argued that nurses with different demographic variables have different perceptions of patient safety. It is imperative for hospital management to prioritize factors like supervisor/manager roles and organizational experience, as these exert significant influence on nurses’ perspectives regarding patient safety culture. Huang et alCitation21 explored the perceptions of pediatric nurses in Taiwan on teamwork climate, job satisfaction, and safety attitudes, and their impact on patient safety. The results showed that teamwork climate, job satisfaction, and safety climate have a significant impact on patient safety. Additionally, the organizational characteristics of the work environment also affect the safety attitudes and job satisfaction of pediatric nurses. Wu et alCitation19 explored the factors influencing overall satisfaction with patient safety culture among hospital staff using the CSAQ. They found that perceptions of management significantly influence overall satisfaction for physicians, nurses, and technicians, while safety climate is a crucial factor for administrative staff. Moreover, by reevaluating the psychometric properties of the Chinese version of the SAQ among medical staff in Taiwan, Tang et alCitation22 found that the emotional state of medical staff significantly impacts patient safety, suggesting the inclusion of assessments for emotional exhaustion and work-life balance in the questionnaire for a more comprehensive evaluation.
Research within healthcare management has delved into the multitude of factors that impact patient safety culture. Notably, LiCitation23 and Lee et alCitation15 independently concluded that the teamwork climate stands out as the foremost factor influencing the attitudes of medical staff toward patient safety. Kim & WengCitation24 incorporated the work experience of physicians and nurses into various patient safety constructs and observed that effective management could enhance the safety climate. For experienced staff, this improvement was linked to increased focus on job satisfaction and teamwork climate, while for less experienced staff, attention to working conditions was crucial. Lee et alCitation10 stated that enhancing the positive psychological well-being of medical staff could lead to a more favorable practice environment for nurses and foster a stronger safety attitude. Lee et al,Citation18 in their examination of the perspectives of physicians and nurses, stressed the paramount importance of addressing cooperation among hospital units, addressing staffing shortages, and managing shift changes to enhance patient safety culture within hospitals. Nevertheless, there remains a limited number of studies that have specifically investigated the influence of management leadership on patient safety culture within healthcare organizations.Citation25,Citation26 In reality, the maintenance of medical staff’s positive attitudes toward patient safety relies heavily on leadership’s commitment to and prioritization of patient safety.Citation27 Management leadership within hospitals plays a vital role in aiding medical staff in comprehending the organizational culture and leadership style, facilitating their ability to handle patient safety issues effectively in their daily practices.Citation25,Citation28,Citation29
While the realm of healthcare management has experienced growing research focus on the elements that impact patient safety culture, there has been limited consideration given to the role of management leadership in shaping this culture within healthcare establishments. This study aims to illuminate how management leadership influences the perception of safety climate among physicians and nurses. It intends to achieve this by exploring the impact of the CSAQ instrument. This study makes two significant contributions. Firstly, it underscores the influence of management leadership on patient safety culture within healthcare organizations by utilizing the CSAQ instrument. Secondly, it delves into the mediating role of the CSAQ instrument to offer a more profound insight into the interplay between management leadership and patient safety culture.
Patients and Method
Hospital Setting
This research was conducted at a medical center situated in Taichung City, Taiwan, recognized as one of the foremost medical establishments among the 19 Medical Centers and First-Class Teaching Hospitals in Taiwan.Citation30 This hospital boasts a substantial staff population exceeding 2300 employees and provides a diverse array of services, including 1005 hospital beds and clinical education for healthcare professionals. It encompasses more than 40 specialized divisions.
Data Collection
In December 2020, an internal survey using the CSAQ was carried out to evaluate the patient safety culture within a medical center located in Taichung City, Taiwan. Medical professionals were invited to electronically complete the questionnaire via an email-delivered hyperlink. For individuals without email addresses, a separate account and password were provided in hard copy format, granting access to the online questionnaire. Some personnel chose the paper-based option, submitting completed questionnaires to a designated collection box. To ensure anonymity, all questionnaires were anonymized and devoid of any personally identifiable information. Prior to the survey’s implementation, pre-testing and cognitive testing were conducted on a subset of 50 hospital employees to ensure the accurate understanding of survey items and response options. During the pre-testing phase, we observed strong reliability across all dimensions (Cronbach’s alpha exceeded 0.8), indicating robust internal consistency in our questionnaire. This bolstered the credibility of the survey instrument utilized in our research. Moreover, in the cognitive testing phase, it was evident that employees effectively grasped the questionnaire content. This success underscores our efforts in ensuring its comprehensibility and effectiveness.
This study was undertaken with permission from the Institutional Review Board of Cheng Ching General Hospital in Taichung City, Taiwan (approval number: HP190028) and conformed to the principles outlined in the Declaration of Helsinki. The participants were informed about the study’s purpose, and their consent to use the data is implied through their participation in the study. Following this, medical staff, including physicians and nurses, were invited to complete the official CSAQ questionnaire (refer to the JCT website, https://psc.jct.org.tw/), with a total of 1500 questionnaires distributed. Among these, 1037 questionnaires were deemed valid, yielding a response rate of 69.13%. The demographic profile of the participants is detailed in . The data revealed that a significant majority of the respondents were female nurses (77.5%) holding bachelor’s degrees (83.9%) and falling within the age range of 31 to 40 years (32.4%). Additionally, more than half of the sampled respondents had been employed at the hospital for over five years. It’s important to note that participation in the study was considered as implied consent for data utilization.
Table 1 Demographic of Participants (n = 1037)
Measures
In our study, we assessed the primary components of patient safety culture by employing the dimensions and scales derived from the CSAQ developed by the JCT. The questionnaire, comprising 46 questions,Citation16,Citation19,Citation31,Citation32 has been validated as an accurate tool for assessing medical staff’s attitudes toward patient safety within healthcare organizations. These questions are categorized into eight distinct areas: Teamwork Climate (focusing on relationships and cooperation among staff), Safety Climate (assessing organizational commitment to safety), Job Satisfaction (evaluating job-related experiences), Stress Recognition (examining stress factors), Perceptions of Management (gauging managerial actions), Working Conditions (evaluating the work environment and support), Emotional Exhaustion (assessing burnout), and Work-Life Balance (considering the balance between work and personal life).
In this research, perceptions of management encompass how hospital staff perceive the hospital management’s commitment to patient safety, serving as an indicator of management leadership. On the other hand, safety climate characterizes the overall organizational atmosphere regarding the dedication to patient safety, providing an expression of patient safety culture. Furthermore, we decided to exclude work-life balance due to its utilization of a four-point frequency scale, which differs from an interval scale. Notably, studies by Sexton et alCitation33 and Sexton et alCitation34 have demonstrated a typically low correlation between work-life balance and safety climate. In response to this concern, the remaining five dimensions of the CSAQ were examined to explore the presence of mediators, also referred to as intervening variables, in the causal relationships between perceptions of management and safety climate.
Participants were asked with rating each question using a five-point Likert scale, where 1 signified “Strong Disagree” and 5 represented “Strong Agree”. To ensure precise measurement of the intended outcomes, 15 questions were reverse-scored, implying that a response of “Strong Agree” actually indicated unfavorable perceptions, and vice versa.
The Hypothesized Model
Management leadership plays a pivotal role in enhancing the quality of care and service within healthcare organizations. A recent literature review in the field of healthcare management underscores the significance of positive staff perceptions of management and leadership, revealing their association with crucial outcomes such as safety climate, teamwork climate, working conditions, job satisfaction, and emotional exhaustion.Citation14,Citation16,Citation25 For instance, Weng et alCitation25 investigated the impact of perceptions of management leadership on medical staff regarding patient safety and emphasized the potential role of management leadership in fostering a safety culture by elevating job satisfaction, teamwork climate, and working conditions. In the context of job satisfaction, Wang, Chontawan, and NantsupawatCitation35 argued that physicians and nurses are more likely to find satisfaction in their roles when hospital leaders demonstrate a strong commitment to patient safety. Concerning stress recognition, there is evidence to suggest that when medical staff receive substantial support from management, they perceive less pressure.Citation20 Similarly, research indicates that the reduced efficiency and exhaustion experienced by medical staff, who may struggle to meet the demands of patient-centered care, are closely linked to unsupported or unnoticed safety initiatives by management.Citation16,Citation36 Regarding working conditions, studies on transformational leadership propose that leaders can create an environment characterized by openness, transparency, and flexibility within the hospital, which can significantly influence the perceptions of hospital staff regarding their working conditions.Citation29,Citation37,Citation38
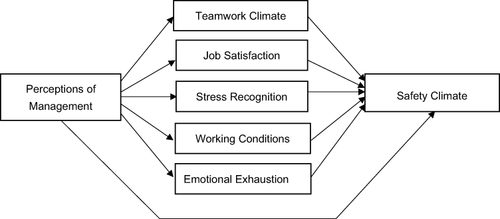
Drawing from the aforementioned studies, we posit that perceptions of management have direct effects on teamwork climate, job satisfaction, stress recognition, emotional exhaustion, and working conditions, respectively. In addition to these direct relationships, we also explore the indirect connection between perceptions of management and safety climate, which is mediated by other variables. The hypothesized model is presented in .
Analysis Methods
The subsequent section delineates the methodologies applied to elucidate the mechanism by which staff perceptions of management leadership impact the safety climate within the healthcare organization. To begin with, Confirmatory Factor Analysis (CFA) was utilized as an initial step to validate the items retained in the model. A model re-specification process was then undertaken by scrutinizing the measurement items. Within this stage, items exhibiting a low factor loading (<0.50) were excluded from the original scale to mitigate potential measurement inaccuracies.Citation39
Mediation analysis was subsequently conducted to assess three main research concepts, namely, the direct effect of perceptions of management on safety climate, the perceptions of management affect safety climate by going through the other five dimensions of the CSAQ, and both two proposed paths are confirmed simultaneously. In other words, a case of no mediation exists if the direct effect is significant and full mediation is obtained if all the effects from the perceptions of management on safety culture are directed through five dimensions of the CSAQ. Partial mediation occurs when part of the influence from the perceptions of management is directed through five dimensions of the CSAQ to safety climate. To do this, we analyze proposed paths using structural equation modeling (SEM) on AMOS 22.0. SEM allows for multiple mediated relationships, particularly when a model with more than one mediator and dependent variable to be considered in one model simultaneously.Citation40
Results
The results of the CFA revealed that six items with weak factor loadings (<0.50) were excluded from the model re-specification process. These items were tc2, sc5, pm3, ee4, ee8, and ee9. As displayed in , a total of 33 questions were utilized to assess seven categories. Teamwork climate exhibited the highest average value, while stress recognition and Emotional Exhaustion had the lowest average values.
Table 2 Results of Confirmatory Factor Analysis
Subsequently, the re-specified model was tested, and the reliability and validity of the measures were assessed. The results indicated that the reliability of all dimensions, as assessed by Cronbach’s alpha, exceeded 0.7, ranging from 0.844 to 0.948. This signifies that the measurement scales demonstrated high internal consistency and reliability.Citation41 Furthermore, the reliability-validity tests demonstrated that the Composite Reliability (CR) of the items exceeded the recommended threshold of 0.70, and the Average Variance Extracted (AVE) estimates were all above 0.50, indicating strong convergent validity of the measurement model. In terms of model fit statistics, the measurement model displayed reasonable fit characteristics. For instance, it exhibited acceptable absolute fit indices (χ2/df = 5.337, Goodness-of-Fit (GFI) = 0.858, Root Mean Squared Residual (RMR) = 0.043, and Root Mean Square Error of Approximation (RMSEA) = 0.065), as well as favorable incremental fit indices (Tucker-Lewis Index (TLI) = 0.927, Comparative Fit Index (CFI) = 0.934), and parsimonious fit indices (Parsimonious Normed Fit Index (PNFI) = 0.827 and Parsimony Goodness-of-Fit Index (PGFI) = 0.725).Citation39,Citation42
A maximum likelihood estimation method was employed in a structural equation analysis to assess the data’s normality. The results indicated that the absolute values of skewness were below 2, and the absolute values of kurtosis were less than 7, providing evidence of data normality. The overall goodness of fit for the structural model depicted in is deemed satisfactory. This includes acceptable absolute fit indices (χ2/df = 4.065, GFI = 0.888, RMR = 0.051, and RMSEA = 0.054), favorable incremental fit indices (TLI = 0.948, CFI = 0.954), and adequate parsimonious fit indices (PNFI = 0.828 and PGFI = 0.736).
Figure 2 Resulting model from the analysis.
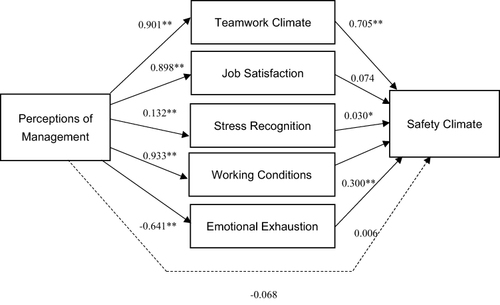
In the model, all standardized regression weights, except for perceptions of management (weight of −0.068 with p = 0.596), job satisfaction to safety climate (weight of 0.074 with p = 0.100), and emotional exhaustion (weight of −0.641 with p = 0.779) on safety climate, are statistically significant.
The standardized effects of the seven patient safety-related dimensions are presented in . All of these effects are statistically significant, except for the direct impact of perceptions of management on safety climate, job satisfaction on safety climate, and emotional exhaustion on safety climate.
Table 3 Direct and Indirect Effects Among Safety-Related Dimensions
Based on the path coefficients derived from the model, it was observed that perceptions of management exerted the most significant total effect on safety climate. Notably, teamwork climate had the highest direct influence on safety climate (weight of 0.705 with p < 0.01). A substantial indirect effect of perceptions of management on safety climate was also evident (weight of 0.914 with p < 0.01), underscoring the strong mediating effects between perceptions of management and safety climate.
Furthermore, the results of the Chi-square difference test indicated no statistically significant difference between the partial and full mediation models.Citation43 In other words, teamwork climate, stress recognition, and working conditions fully mediate the relationship between perceptions of management and safety climate. Specifically, 63.5% (0.901*0.705) of this mediation is attributed to teamwork climate, 27.9% (0.933*0.300) to working conditions, and 0.3% (0.132*0.030) to stress recognition.
Discussion
Our aim is to assess the influence of management leadership on patient safety culture using the CSAQ framework. The following is a discussion of the results of our investigation.
First, the measurement of questions across dimensions was observed to differ from that in the Chinese version of the SAQ developed by the JCT. We re-evaluated thirty-three items, measuring seven dimensions, by considering their psychometric properties in relation to patient safety culture as perceived by physicians and nurses within their work environment. As a result, one question was removed from each of the dimensions: teamwork climate (item tc2), safety climate (item sc5), and perceptions of management (item pm3). Additionally, three questions from the emotional exhaustion dimension (items ee4, ee8, and ee9) were excluded. However, no questions were eliminated from the job satisfaction, stress recognition, and working conditions dimensions.
Second, prior studies have stated that positive safety culture in healthcare organizations can result from management leadership policies and management styles that strengthen medical staff professional fulfillment and engagement.Citation29,Citation38 However, consistent with the findings of Weng et al,Citation25 our study suggests that hospital management should be cognizant of the fact that solely focusing on enhancing staff perceptions of management leadership may not be an effective way to enhance patient safety culture. Instead, the hospital management should put more effort into investing resources to heighten other mediated factors such as teamwork climate, working conditions, and stress recognition. In our study, the effect of the perceptions of management on safety climate is mostly mediated by teamwork climate (63.5%). Studies agree on the fact that staff’s attitude toward patient safety may change positivity if hospital management dedicated to creating a supportive, cooperative, and enjoyable environment for medical staff within the unit or hospital.Citation44–46 Therefore, implementations for improving patient safety culture should begin with teamwork climate improvement.
Next, our study highlights the mediating role of working conditions in the relationship between perceptions of management and safety climate, accounting for 27.9% of the mediation effect. Based on these findings, we recommend the implementation of psychological and physical interventions aimed at improving working conditions for medical staff. In practical terms, addressing issues such as manpower shortages and high workloads among physicians and nurses is crucial,Citation47 as these factors contribute to psychological and physical stress that can erode medical staff’s commitment to a culture of safety in healthcare. Various management practices can play a role in regulating working conditions, including the implementation of effective handoffs and transitions, providing job control to staff, and establishing transparent incentive schemes.
Furthermore, it is essential for leaders in healthcare organizations to adopt a transformational leadership style. This leadership approach serves as a model for inspiring and motivating medical staff to think creatively and perform beyond expectations.Citation29,Citation38,Citation46 Given that hospitals are labor-intensive entities, human resource management becomes paramount not only for reshaping leadership styles but also for ensuring the health and well-being of medical staff in the workplace.
Finally, while it is true that stress recognition demonstrates a relatively weak mediating effect (0.3%) on the relationship between perceptions of management and safety climate, it is imperative not to disregard any stress-related issues among medical staff in the healthcare industry. Our findings align with those of Park & Kim,Citation48 highlighting that stress recognition stands as a critical factor influencing the organizational culture of patient safety. Park and KimCitation48 have identified heightened stressors and challenges as risk factors that can contribute to patient safety incidents. To address this concern, it is recommended to implement initiatives such as Mindfulness-Based Stress Reduction (MBSR) programs or Appreciative Inquiry groups. These programs can help alleviate anxiety and irritability among medical staff during medical encounters.Citation49
Conclusion
Understanding the pivotal role of management leadership within a hospital is of utmost importance in fostering an environment where medical staff actively engage in patient safety-oriented initiatives. Our study’s findings underscore that the influence of management perceptions on safety climate is entirely mediated through three critical facets of patient safety: teamwork climate, working conditions, and stress recognition. Consequently, it is incumbent upon hospital management to concentrate their efforts on enhancing these three dimensions to advance the patient safety culture.
Furthermore, it’s worth noting that the generalizability of our research results may be limited since all respondents were drawn from a private medical center in Taiwan. Therefore, the applicability of our model to other hospitals or regions may vary. A promising avenue for future research could involve comparing management leadership’s impact on patient safety culture between public and private hospitals. Additionally, the research framework we employed may have limitations regarding the scope of the SAQ. It may be valuable to explore other organizational culture factors that influence the development of safety climate. For instance, factors such as cohesiveness, role significance, orientation to power, and communication could serve as potential mediators to promote a high-quality patient safety culture within healthcare organizations.
Data Sharing Statement
According to the hospital’s regulations, individual de-identified data should pass both the Research and Development Committee and Institutional Review Board (IRB). Researchers should write a research proposal and apply it in a clinical trial to the IRB of the hospital. All data listed in the present manuscript can be obtained through e-mail if both committees agree to the application.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Vincent C. The Essentials of Patient Safety. London: Blackwell Publishing; 2011.
- Australian Institute of Health and Welfare (AIHW). Australia’s health 2018. Available from: https://www.aihw.gov.au/getmedia/7c42913d-295f-4bc9-9c24-4e44eff4a04a/aihw-aus-221.pdf.aspx?inline=true. Accessed January 14, 2023.
- Sousa P, Uva AS, Serranheira F, Nunes C, Leite ES. Estimating the incidence of adverse events in Portuguese hospitals: a contribution to improving quality and patient safety. BMC Health Serv Res. 2014;14(1):311. doi:10.1186/1472-6963-14-311
- World Health Organization (WHO). Patient safety: making health care safer (No. WHO/HIS/SDS/2017.11). World Health Organization; 2017.
- Zúñiga F, Schwappach D, De Geest S, Schwendimann R. Psychometric properties of the Swiss version of the nursing home survey on patient safety culture. Saf Sci. 2013;55:88–118. doi:10.1016/j.ssci.2012.12.010
- Gonzalez JFZ, Wolf G, Dudjak L, Jordan B. Impact of magnet culture in maintaining quality outcomes during periods of organizational transition. J Nurs Care Qual. 2015;30(4):323–330. doi:10.1097/NCQ.0000000000000118
- Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016;353:i2139. doi:10.1136/bmj.i2139
- European Union Network for Quality in Health Care. Use of Patient Safety Culture Instrument and Recommendations. European Network for Quality in Health Care, Office for Quality Indicators; 2006.
- Allen S, Chiarella M, Homer CS. Lessons learned from measuring safety culture: an Australian case study. Midwifery. 2010;26(5):497–503. doi:10.1016/j.midw.2010.07.002
- Lee TSH, Tzeng WC, Chiang HH. Impact of coping strategies on nurses’ well‐being and practice. J Nurs Scholarsh. 2019;51(2):195–204. doi:10.1111/jnu.12467
- Watts BV, Percarpio K, West P, Mills PD. Use of the Safety Attitudes Questionnaire as a measure in patient safety improvement. J Patient Saf. 2010;6(4):206–209. doi:10.1097/PTS.0b013e3181fbbe86
- Patel S, Wu AW. Safety culture in Indian hospitals: a cultural adaptation of the safety attitudes questionnaire. J Patient Saf. 2016;12(2):75–81. doi:10.1097/PTS.0000000000000085
- Soh SE, Barker A, Morello R, Dalton M, Brand C. Measuring safety climate in acute hospitals: rasch analysis of the safety attitudes questionnaire. BMC Health Serv Res. 2016;1(1):497. doi:10.1186/s12913-016-1744-4
- Sexton JB, Helmreich RL, Neilands TB, et al. The safety attitudes questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res. 2006;6(1):44. doi:10.1186/1472-6963-6-44
- Lee YC, Weng SJ, Stanworth JO, Hsieh LP, Wu HH. Identifying critical dimensions and causal relationships of patient safety culture in Taiwan. J Med Imaging Health Inform. 2015;5(5):995–1000. doi:10.1166/jmihi.2015.1482
- Huang CH, Wu HH, Lee YC. The perceptions of patient safety culture: a difference between physicians and nurses in Taiwan. Appl Nursg Res. 2018;40:39–44. doi:10.1016/j.apnr.2017.12.010
- Huang CH, Wu HH, Chou CY, Dai H, Lee YC. The perceptions of physicians and nurses regarding the establishment of patient safety in a regional teaching hospital in Taiwan. Iran J Public Health. 2018;47(6):852–860.
- Lee YC, Shieh JI, Huang CH, Wang CY, Wu HH. Analyzing patient safety culture from viewpoints of physicians and nurses—a case of a regional teaching hospital in Taiwan. J Healthc Qual. 2017;39(5):294–306. doi:10.1097/JHQ.0000000000000065
- Wu CF, Wu HH, Lee YC, Huang CH. What attributes determine overall satisfaction in patient safety culture? An empirical study of the perceptions of hospital staff in Taiwan. J Test Eval. 2021;49(1):629–639. doi:10.1520/JTE20180713
- Lee YC, Huang CH, Wu CF, Hsueh HW, Wu HH. A Longitudinal study of identifying critical variables influencing patient safety culture from nurses’ viewpoints in Taiwan. J Test Eval. 2019;47(5):3387–3398. doi:10.1520/JTE20180060
- Huang CH, Wu HH, Lee YC, Van Nieuwenhuyse I, Lin MC, Wu CF. Patient safety in work environments: perceptions of pediatric healthcare providers in Taiwan. J Pediatr Nurs. 2020;53:6–13. doi:10.1016/j.pedn.2020.03.005
- Tang YT, Wu HH, Lee YC, Huang CHH. Evaluating the psychometric properties of the Chinese version of the Safety Attitudes Questionnaire among medical staff in Taiwan. J Health Organ Manag. 2023;37(1):84–95. doi:10.1108/JHOM-03-2022-0084
- Li AT. Teamwork climate and patient safety attitudes: associations among nurses and comparison with physicians in Taiwan. J Nurs Care Qual. 2013;28(1):60–67. doi:10.1097/NCQ.0b013e318262ac45
- Kim SH, Weng SJ. Incorporating work experience of medical staff into patient safety climate management: a multi-group analysis. BMC Health Serv Res. 2018;18(1):919. doi:10.1186/s12913-018-3747-9
- Weng SJ, Kim SH, Wu CL. Underlying influence of perception of management leadership on patient safety climate in healthcare organizations–A mediation analysis approach. Int J Qual Health C. 2017;29:111–116. doi:10.1093/intqhc/mzw145
- Sammer CE, Lykens K, Singh KP, Mains DA, Lackan NA. What is patient safety culture? A review of the literature. J Nurs Scholarsh. 2010;42(2):156–165. doi:10.1111/j.1547-5069.2009.01330.x
- Frankel A, Grillo SP, Baker EG, Huber CN, Abookire S, Grenham M. Patient safety leadership walkrounds? At partners healthcare: learning from implementation. Jt Comm J Qual Saf. 2005;31:423–437. doi:10.1016/S1553-7250(05)31056-7
- Frankel A, Grillo SP, Pittman M, et al. Revealing and resolving patient safety defects: the impact of leadership WalkRounds on frontline caregiver assessments of patient safety. Health Serv Res. 2008;43(6):2050–2066. doi:10.1111/j.1475-6773.2008.00878.x
- Boamah SA, Laschinger HKS, Wong C, Clarke S. Effect of transformational leadership on job satisfaction and patient safety outcomes. Nurs Outlook. 2018;66(2):180–189. doi:10.1016/j.outlook.2017.10.004
- Joint Commission of Taiwan (JCT). The Lists of Evaluation for Hospitals in 2015–2018 in Taiwan. Available from: https://www.jct.org.tw/cp-49-2584-efab2-1.html. Accessed March 3, 2023.
- Chi CY, Huang CH, Lee YC, Wu HH. Critical demographic variables on affecting patient safety culture from medical staffs’ viewpoints. Eng Lett. 2019;27:EL_27_2_09.
- Cheng CY, Lee YC, Huang CH, Wu HH. Assessing the medical staff’s overall satisfaction of patient safety culture from a regional teaching hospital in Taiwan. J Test Eval. 2020;48(6):4153–4162. doi:10.1520/JTE20180116
- Sexton JB, Schwartz SP, Chadwick WA, et al. The associations between work–life balance behaviours, teamwork climate and safety climate: cross-sectional survey introducing the work–life climate scale, psychometric properties, benchmarking data and future directions. BMJ Qual Saf. 2017;26(8):632–640. doi:10.1136/bmjqs-2016-006032
- Sexton JB, Adair KC, Leonard MW, et al. Providing feedback following leadership walkrounds is associated with better patient safety culture, higher employee engagement and lower burnout. BMJ Qual Saf. 2018;27(4):261–270. doi:10.1136/bmjqs-2016-006399
- Wang X, Chontawan R, Nantsupawat R. Transformational leadership: effect on the job satisfaction of Registered Nurses in a hospital in China. J Adv Nurs. 2012;68(2):444–451. doi:10.1111/j.1365-2648.2011.05762.x
- O’Mahony N. Nurse burnout and the working environment. Emerg Nurs. 2011;19(5):30–37. doi:10.7748/en2011.09.19.5.30.c8704
- Mahmoud A. A study of nurses’ job satisfaction: the relationship to organizational commitment, perceived organizational support, transactional leadership, transformational leadership, and level of education. Eur J Sci Res. 2008;22:286–295.
- Westerberg K, Tafvelin S. The importance of leadership style and psychosocial work environment to staff‐assessed quality of care: implications for home help services. Health Soc Care Community. 2014;22(5):461–468. doi:10.1111/hsc.12084
- Bagozzi RP, Yi Y. On the evaluation of structural equation models. Acad Mark Sci Rev. 1988;16(1):74–94. doi:10.1177/009207038801600107
- Lowry PB, Gaskin J. Partial least squares (PLS) structural equation modeling (SEM) for building and testing behavioral causal theory: when to choose it and how to use it. IEEE Trans Prof Commun. 2014;57(2):123–146. doi:10.1109/TPC.2014.2312452
- Nunnally JC. Psychometric Theory. 2nd ed. New York: McGraw-Hill; 1978.
- Hair J, Black W, Babin B, Anderson R, Tatham R. Multivariate Data Analysis. 6th ed. N.J: Pearson Prentice Hall; 2006.
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88(3):588–606. doi:10.1037/0033-2909.88.3.588
- Goh SC, Chan C, Kuziemsky C. Teamwork, organizational learning, patient safety and job outcomes. Int J Health Care Qual Assur. 2013;26(5):420–432. doi:10.1108/IJHCQA-05-2011-0032
- Joy A, Dittmar PC. Interprofessional collaboration. In: Hospital Medicine. Cham: Springer; 2017:95–103.
- Huang CH, Wu HH, Lv R, Wang S, Ding X, Guo Z. The role of perceptions of management plays in promoting the development of patient safety culture in the healthcare organizations. In: Proceedings of International Conference on Application of Information and Communication Technology and Statistics in Economy and Education (ICAICTSEE). 2019:62–68.
- Afework A, Tamene A, Tesfaye A, Tafa A, Gemede S. Status and factors affecting patient safety culture at Dilla University teaching hospital: a mixed-method cross-sectional study. Risk Manag Healthc Policy. 2023;16:1157–1169. doi:10.2147/RMHP.S419990
- Park YM, Kim SY. Impacts of job stress and cognitive failure on patient safety incidents among hospital nurses. Saf Health Work. 2013;4(4):210–215. doi:10.1016/j.shaw.2013.10.003
- Lee YC, Huang SC, Huang CH, Wu HH. A new approach to identify high burnout medical staffs by kernel k-means cluster analysis in a regional teaching hospital in Taiwan. Inquiry J Health Care. 2016;53:1–6. doi:10.1177/0046958016679306