Abstract
Objective
To validate a simple scoring system to classify dengue viral infection severity to patients in different settings.
Methods
The developed scoring system derived from 777 patients from three tertiary-care hospitals was applied to 400 patients in the validation data obtained from another three tertiary-care hospitals. Percentage of correct classification, underestimation, and overestimation was compared. The score discriminative performance in the two datasets was compared by analysis of areas under the receiver operating characteristic curves.
Results
Patients in the validation data were different from those in the development data in some aspects. In the validation data, classifying patients into three severity levels (dengue fever, dengue hemorrhagic fever, and dengue shock syndrome) yielded 50.8% correct prediction (versus 60.7% in the development data), with clinically acceptable underestimation (18.6% versus 25.7%) and overestimation (30.8% versus 13.5%). Despite the difference in predictive performances between the validation and the development data, the overall prediction of the scoring system is considered high.
Conclusion
The developed severity score may be applied to classify patients with dengue viral infection into three severity levels with clinically acceptable under- or overestimation. Its impact when used in routine clinical practice should be a topic for further study.
Introduction
Dengue viral infection is one of the most challenging tropical diseases internationally.Citation1 The infection may be complicated with hypotensionCitation2 and bleeding abnormality, leading to high mortality.Citation2,Citation3 The infection also has high economic impact due to high cost of care.Citation4,Citation5 Prognostication of disease severity may help clinicians decide which patients should be admitted to hospital, or which patients may safely be treated as outpatients.Citation6
A clinical decision rule is a clinical tool that quantifies the individual contributions that various components of the history, physical examination, and basic laboratory results make toward the diagnosis, prognosis, or likely response to treatment in a patient. Clinical decision rules attempt to formally test, simplify, and increase the accuracy of clinicians’ diagnostic and prognostic assessments.Citation7
A prediction rule for severe dengue infection based on clinical signs and simple laboratory results was successful in predicting dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS).Citation8 Decision tree algorithms,Citation9–Citation12 diagnostic decision algorithms,Citation13 the pediatric logistic organ dysfunction score,Citation14–Citation18 and the disseminated intravascular coagulation scoring systemCitation19,Citation20 were also developed. Other studies were also designed to differentiate dengue fever (DF),Citation9,Citation10 types of dengue infection (DF, DHF, or DSS),Citation10,Citation12,Citation13 fatal conditions,Citation12 development of DHF,Citation11 multiple organ dysfunctions,Citation14–Citation16 DSS mortality,Citation17,Citation18 and disseminated intravascular coagulation.Citation19,Citation20
Earlier, we developed a scoring system to help screen patient severityCitation21 based on clinical parameters and simple laboratory tests. The present study was conducted to externally validate this scoring system to patients in different settings.
Materials and methods
Patients
Medical files of patients with dengue viral infection aged 1–15 years were retrieved from hospital database, all cases were included in the study. The following International Classification of Diseases (ICD)-10 codes were used: A-90 (DF), A-91 (DHF), and A-910 (DHF with shock).
Definition of dengue severity
The severity of dengue infection was defined by the following criteria, as in the previous studyCitation21
Dengue infection – acute or abrupt onset of fever, accompanied by a positive tourniquet test, and white blood count ≤5,000/μLCitation22
DHF – all items of the following:Citation23
Acute or abrupt fever for 2–7 days
At least one of the following bleeding episodes:
– Positive tourniquet test
– Petechiae, ecchymoses, or purpura
– Bleeding from mucosa, gastrointestinal tract, injection sites, or other location
– Hematemesis or melena
Platelets ≤100,000/μL
At least one of the following plasma leakage evidences:
– Hemoconcentration assessed by an increase in hematocrit ≥20% from previous hematocrit
– Signs of plasma leakage, such as pleural effusion or ascites, or an evidence of hypoalbuminemia
DSS – all items for DHF above, accompanied with evidence of circulatory failure, such as:Citation23
Rapid and weak pulse; and
Pulse pressure ≤20 mmHg.
Or manifested by:
Hypotension; and
Cold body temperature or irritability.
Development data
The original data used to develop the score were obtained from three university-affiliated tertiary-care hospitals in Nakorn Sawan, Kampaeng Phet, and Uttaradit between 2007 and 2010 (n=777).
Validation data
The validation data were from similar patients as in the development data in another three university-affiliated tertiary-care hospitals in Phrae, Lamphun, and Chiang Mai during the same period (n=400).
Data analysis
The development data and the validation data were compared by exact probability tests or Student’s t-tests or Wilcoxon’s rank sum tests. The severity score was assigned to the patients based on the scoring system proposed from the earlier study, analyzed by multivariable ordinal logistic regression. Assigned item scores were derived by transformation of the coefficients of parameters ().Citation21 The proportions if correct prediction, underestimation, and overestimation in the development and the validation data were compared by areas under the receiver operating characteristic curves (AuROC). The predictive ability of the scoring system of both datasets was graphically compared by the probability or risk curves.
Table 1 Score assignment scheme for classifying dengue severity
Results
Patients in the development and the validation data were similar in the presence of the following symptoms and signs: vomiting, cough, bleeding, systolic blood pressure, diastolic blood pressure, hematocrit, aspartate aminotransferase, prothrombin time, partial thromboplastin time, but were different in gender, age, hepatomegaly, headache, myalgia, abdominal pain, rash, pleural effusion, petechiae, pulse pressure, hemoglobin, white cell count, lymphocytes, neutrophils, platelets, and alanine aminotransferase ().
Table 2 Clinical characteristics of dengue patients in the development and the validation data
The severity score of patients in the development data was higher than in those in the validation data (5.6±4.1 versus 4.2±2.5, P<0.001), and the percentage of DSS was higher (6.4% versus 1.5%, P<0.001) ().
Table 3 Score-derived dengue severity levels in the development and the validation data
In the validation data, classification of patients into three severity levels (DF, DHF, and DSS) yielded the following results.
Patients scoring less than 2.5 predicted DF correctly in 21.5% (n=86 from 208), with 1-level underestimation in 11% (n=44) and 2-level underestimation in 0.8% (n=3), a total of 11.8% (n=47).
Scores 2.5–11.5 predicted DHF correctly in 28.0% (n=112 from 157), with an underestimation in 6.8% (n=27) and an overestimation in 30.5% (n=122).
Scores above 11.5 predicted DSS correctly in 1.3% (n=5 from 35), with only 1-level overestimation in 0.3% (n=1) ().
Table 4 Score-classified severity and criterion-classified dengue severity in the validation data
A total correct prediction was obtained in 50.8% (versus 60.7% in the development data), with an overall underestimation of 18.6% (versus 25.7%) and an overall overestimation in 30.8% (versus 13.5%).
The ability of the score to discriminate DF from DHF and DSS was different between the development and the validation data (AuROC =74.17% versus 70.76%, P=0.003). The ability to discriminate DSS from DF and DHF was also different (AuROC =88.77% versus 75.91%, P<0.001), as shown in and .
Figure 1 Score-predicted probability of severity in the development data (solid lines) and the validation data (dashed lines). Vertical dotted lines represent score-derived criteria for classifying patients into DF, DHF, and DSS.
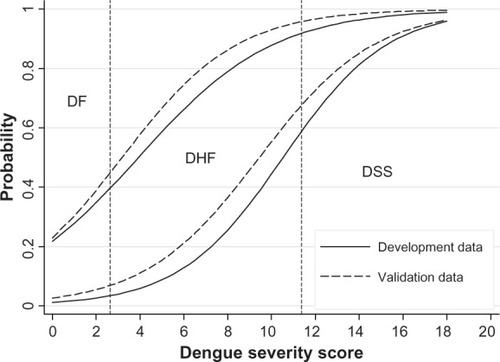
Table 5 Discriminative performance of the dengue severity score in the development data and the validation data
Discussion
The scoring systems for dengue infection in the past were reported to be successful when validated.Citation24 A simple decision tree using existing data was also successful as a guideline to admit DHF patients into hospitals, reducing unnecessary admission of mild D F.Citation25 A probability equation and a decision tree for DHF derived in 2004 and internally validated in 2007 was also successful in predicting DHF at first presentation, avoiding unnecessary hospital admission.Citation26
The scoring system proposed in the prior studyCitation21 was less accurate when validated to the new patients. This reduced accuracy may have occurred due to the fact that patients in the validation data were more severe or less severe than the development data, such as seen in this study.
However, from a clinical perspective, this scoring system would be useful in routine practice, as it requires only simple clinical data which can be obtained routinely and is usually available in all levels of patient care centers.
When applied to clinical practice, patients with a low score who are likely to have DF could be treated as outpatients, while those with a higher score who are likely to have DHF could be admitted, and those with the highest score who are likely to have DSS should be admitted for close monitoring, such as in an intensive care unit.
An impact of application of the score into routine clinical practice should be studied further to confirm its usefulness.
Conclusion
Despite some difference between patients in the validation and in the development data, the scoring system could still discriminate dengue infection severity with clinically acceptable over- or underestimation. The proposed scoring system is likely to be generalized and applied to routine practice in similar patients and settings.
Ethical approvals
The present study was approved by the Ethics Committee for Research in Patients, the Faculty of Medicine, Chiang Mai University, and the research ethical committees of the six hospitals.
Acknowledgments
The authors wish to thank the authorities of the six hospitals for their permission on data collection and wish to thank Chiang Mai University for their financial support.
Funding
The study was partially funded by the Faculty of Medicine, Chiang Mai University.
Disclosure
The authors report no conflicts of interest in this work.
References
- HalsteadSBDengueLancet2007370101644165217993365
- ChaudharyRKhetanDSinhaSTransfusion support to dengue patients in a hospital based blood transfusion service in north IndiaTransfus Apher Sci200635323924417097349
- ChhinaDKGoyalOGoyalPKumarRPuriSChhinaRSHaemorrhagic manifestations of dengue fever and their management in a tertiary care hospital in north IndiaIndian J Med Res2009129671872019692757
- KongsinSJiamtonSSuayaJAVasanawathanaSSirisuvanPShepardDSCost of dengue in ThailandDengue Bull2010347788
- SuayaJAShepardDSSiqueiraJBCost of dengue cases in eight countries in the Americas and Asia: a prospective studyAm J Trop Med Hyg200980584685519407136
- LeeLKEarnestACarrascoLRSafety and cost savings of reducing adult dengue hospitalization in a tertiary care hospital in SingaporeTrans R Soc Trop Med Hyg2013107374223296696
- McGinnTGGuyattGHWyerPCUsers’ guides to the medical literature. XXII: how to use articles about clinical decision rulesJAMA20062841798410872017
- PongpanSWisitwongATawichasriCPatumanondJPrognostic indicators for dengue infection severityInt J Clin Pediatr2013211218
- LaiWPChienTWLinHJSuSBChangCHA screening tool for dengue fever in childrenPediatr Infect Dis J201332432032423249912
- TannerLSchreiberMLowJGHDecision tree algorithms predict the diagnosis and outcome of dengue fever in the early phase of illnessPLoS Negl Trop Dis200823e19618335069
- BrasierARJuHGarciaJA three-component biomarker panel for prediction of dengue hemorrhagic feverAm J Trop Med Hyg201286234134822302872
- ThitiprayoonwongseDSuriyapkolPSoonthornphisajNData mining of dengue infection using decision tree. Proceeding of the 12th WSEAS International Conference on Applied Computer Science; 2012 May 11–13; SingaporeLatest Advances in Information Science and Applications2012154159
- PottsJAGibbonsRVRothmanALPrediction of dengue disease severity among pediatric Thai patients using early clinical laboratory indicatorsPLoS Negl Trop Dis201048e76920689812
- LeteurtreSDuhamelAGrandbastienBLacroixJLeclercFPaediatric logistic organ dysfunction (PELOD) scoreLancet2006367951489716546531
- LeteurtreSMartinotADuhamelAValidation of the paediatric logistic organ dysfunction (PELOD) score: prospective, observational, multicentre studyLancet2003362937919219712885479
- HonnaLTriratnaSTriwaniTheodorusUse of pediatric logistic organ dysfunction (PELOD) in determining prognostic among pediatric intensive care unit patientsPaediatr Indones2010506347350
- DewiLPNurfitriEPediatric logistic organ dysfunction score as a predictive tool of dengue shock syndrome outcomesPaediatr Indones20125227277
- IskandarHRMulyoDAgnesPSuryatinYComparison of pediatric logistic organ dysfunction (PELOD) score and pediatric risk of mortality (PRISM) III as a mortality predictor in patients with dengue shock a mortality predictor in patients with dengue shock syndromePediatrics2008121Suppl 2S129
- CarlosCCOishiKCincoMTDDComparison of clinical features and hematologic abnormalities between dengue fever and dengue hemorrhagic fever among children in the PhilippinesAm J Trop Med Hyg200573543544016103617
- OishiaKMapuaeCACarlosdCCDengue and other febrile illnesses among children in the PhilippinesDengue Bull2006302634
- PongpanSWisitwongATawichasriCPatumanondJNamwongpromSDevelopment of dengue infection severity scoreISRN Pediatr2013201384587624324896
- SawasdivornSVibulvattanakitSSasavatpakdeeMIamsirithavornSEfficacy of clinical diagnosis of dengue fever in paediatric age groups as determined by WHO case definition 1997 in ThailandDengue Bull2001255664
- World Health Organization [homepage on the Internet]Dengue hemorrhagic fever: diagnosis, treatment, prevention and controlGenevaWorld Health Organization1997 Available from: http://www.who.int/csr/resources/publications/dengue/Denguepublication/enAccessed December 29, 2013
- ChangKLuP-LKoW-CDengue fever scoring system: new strategy for the early detection of acute dengue virus infection in TaiwanJ Formos Med Assoc20091081187988519933032
- LeeVJLyeDCSunYLeoYSDecision tree algorithm in deciding hospitalization for adult patients with dengue haemorrhagic fever in SingaporeTrop Med Int Health20091491154115919624479
- TheinTLLeoY-SLeeVJSunYLyeDCValidation of probability equation and decision tree in predicting subsequent dengue hemorrhagic fever in adult dengue inpatients in SingaporeAm J Trop Med Hyg201185594294522049054
