Abstract
Background and Objectives
A wealth of research has identified adverse childhood experiences (ACEs; abuse, neglect, violence or disorder in the home) as a strong risk factor for substance misuse. Synthesis of the existing evidence is critical to shape policy and inform directions for future research. Existing reviews have focused on specific substances or substance use outcomes (eg, disorder), and do not include discussion of the mechanisms that operate between ACEs and substance misuse. The current umbrella review aims to synthesize reviews on the relationship between ACEs and substance misuse, review the evidence on the mechanisms linking these, identify existing gaps in our knowledge, and discuss critical directions for future research, practice, and public policy.
Methods
Two electronic databases (PsycINFO and Medline) were searched for reviews published between 1998 and 2022 on the link between ACEs and substance misuse. Twenty articles met eligibility criteria and were qualitatively synthesized.
Results
Results overwhelmingly demonstrated an elevated risk of substance misuse or disorder, among adolescents and adults exposed to ACEs. Research on the mechanisms that explain this link highlights a multitude of potential intervention targets, with childhood stress propelling a cascade of effects across neurobiological, endocrine, immune, metabolic, and nervous systems, impacting psychosocial and cognitive functioning. Nonetheless, the literature is subject to limitations surrounding potential unmeasured cofounders and causality, as well as decontextualizing childhood adversity from broader structural issues that influence the link between ACEs and substance misuse. Research, policy, and practice that seek to holistically understand and address the relationship between ACEs and substance misuse within the broader social determinants of health is crucial.
Introduction
Substance misuse refers to the use of alcohol and other drugs in ways that confer harm to the user or those around them.Citation1 Accordingly, substance misuse accounts for a substantial burden of disease globally, through substance use disorders as well as associated unintentional injuries, chronic diseases, and suicide.Citation2 Reducing this disease burden necessitates prevention approaches at both the universal level (ie, delivered to all), and critically, targeted to those most at risk of substance misuse. Moreover, treatment and rehabilitative approaches that recognize drivers of substance misuse and disorder are critical. In this respect, a life course approach that considers the upstream, social determinants of health is vital,Citation3 and has identified exposure to adverse childhood experiences (ACEs) as an important determinant to reduce the burden of substance misuse.Citation4
While the relationship between early-life stressors and subsequent risk for substance misuse has been recognized for decades, in 1998 the CDC-ACE study examined associations of a set of seven types of ACEs (emotional, physical, sexual abuse, domestic violence, living with a household member with a mental illness, substance use problems, or ever incarcerated) with health risk behaviors and disease in over 9500 adult members of the Kaiser Permanente Health Maintenance Organisation.Citation5 A graded association was found between the number of ACEs experienced and all studied health risk behaviors and diseases, including substance misuse, mental illness, sexually transmitted disease, obesity, heart disease and cancer.Citation5 This study spurred a wealth of research demonstrating associations between a specific set of childhood adversity types (which was expanded to include emotional and physical neglect, and parental divorceCitation6,Citation7) and physical and mental health outcomes, including substance misuse. This research has drawn attention to ACEs as a public health issue, highlighting the critical role of public policy, population health, and clinical practice in preventing ACE exposure and intervening on the pathways linking exposure to elevated risk for substance misuse and other poor health outcomes.Citation8 Encouragingly, policy and practice changes arising out of the ACEs literature indicate some success in reducing the prevalence of certain types of ACEsCitation9 and a growing recognition of the importance of applying a trauma-informed lens to research and clinical practice addressing substance misuse.Citation10,Citation11
Given the substantial and accumulating research available, synthesis of the existing evidence is critical to continue to shape policy and inform directions for future research. While some reviews of the literature have examined the association between ACEs and the misuse of specific substances or other substance use outcomes (eg, disorder), to our knowledge there exists no synthesis of the relationship between ACEs and substance misuse that synthesizes the evidence more broadly. Moreover, reviews considering the potential mechanisms that operate between ACEs and substance misuse, as well as critiquing existing limitations, are rarely conducted alongside the evidence synthesis. The current umbrella review aims to synthesize the last quarter century of reviews on the relationship between ACEs and substance misuse, the mechanisms linking these, identify existing gaps in our knowledge and critical directions for future research.
Defining Adverse Childhood Experiences (ACEs)
In this umbrella review, ACEs are conceptualized as experiences of severe threat or deprivation occurring in childhood, approximately aligned with the CDC definition of ACEs that includes physical, sexual, or emotional abuse, physical or emotional neglect, exposure to domestic violence, household mental illness or substance misuse, household incarceration, and parental separation.Citation5,Citation6 In recent years, researchers have called attention to some of the limitations of the ACEs framework: that it excludes other exposures that constitute childhood adverse experiences, such as bullying or community violence;Citation12 and that it removes childhood adversity from its broader structural context and thus oversimplifies the issue as rooted in individuals and families.Citation13,Citation14 Nonetheless, the current synthesis conceptualizes ACEs according to this framework given its predominance throughout the last quarter-century of research and its influence on public policy.Citation15 We acknowledge its limitations and do not exclude studies that include a broader conceptualization of ACEs, as long as they also include some of the traditional set of 10 ACEs. We employ an aggregative approach to ACEs, rather than reviewing evidence from specific types of ACEs (eg, solely sexual abuse), as this enables a synthesis of the complex and abundant existing evidence. This approach is supported by prevalence studies demonstrating the majority of children exposed to adversity will experience multiple types,Citation16,Citation17 rendering examination of the unique effects of one type of ACE on substance misuse as limiting ecologically validity. Further, there is robust evidence of a dose–response effect linking an increasing number of different types of ACEs with an elevated risk of substance use problems,Citation4 highlighting that the number of ACEs itself is an important risk factor. Finally, much of the evidence on the biological embedding of adversity stems from the concept of allostatic load, which incorporates all-cause stress in examining associations with pathology.Citation18 However, we also acknowledge that considering ACEs in the aggregate compared to distinct types of exposures may obscure nuances in the developmental mechanisms linking ACEs to substance misuse.Citation19 Our approach to review the available evidence on the conceptualization of ACEs arising from the landmark ACE study and ACEs in the aggregate is to reduce heterogeneity where possible and facilitate an overarching review on the existing evidence.
Methods
An umbrella review of the link between ACEs and substance misuse was conducted. An umbrella review is a review of existing reviews, to give a high-level overview of a given topic. Two electronic databases (PsycINFO and Medline) were searched on March 4, 2022, and review articles known to the authors were also assessed for eligibility. Eligible study designs were systematic reviews (both qualitative and quantitative) and meta-analyses that examined associations between ACEs and substance misuse. Studies were eligible if a peer-reviewed full text was available between January 1, 1998 to March 4, 2022 (1998 being the year of publication of the original ACE study), included human participants, and included associations between aggregative ACEs (at least two types of ACEs) measured between age 0 and 18 years and a substance misuse outcome. For the purposes of this review, substance misuse was the use of alcohol and/or other drugs in such a way that confers social, occupational, justice- or health-related harm to the individual or others. Alcohol and cannabis outcomes were included if studies indicated some form of harmful use (eg, heavy use, increased use, problem use, dependence, disorder) or any use under the age of 18 in line with guidelines for the safe consumption of alcohol.Citation20 For prescription drugs harm was defined as any use contrary to prescribed instructions; for illicit drugs and tobacco smoking this was defined as any use given the potential for social, occupational, justice- or health-related harm arising from any use. Studies assessing scale formation only, or dissertations were excluded. Search terms are presented in Supplementary Table 1. References were exported to systematic review software (Covidence) and duplicates removed automatically by the software. Titles and abstracts were screened to ascertain eligibility in a first step. For articles that were deemed potentially eligible after this first step, full-text articles were then reviewed against eligibility criteria. Data extracted from the eligible studies included first author, publication date, the ACEs included, the substance misuse outcome(s) measured, the sample characteristics, sample size, and main findings. Results from quantitative syntheses (eg, meta-analyses) are presented in the first section of the results; results from qualitative systematic reviews are summarized in the second section of the results. Given the substantial heterogeneity between samples of individual studies, most systematic reviews employed qualitative synthesis, and thus, the current umbrella review includes predominately qualitative synthesis. The current review synthesizes the overall findings of the included reviews, rather than the findings of individual primary studies included in these reviews.
Results
What is the Relationship Between ACEs and Substance Misuse?
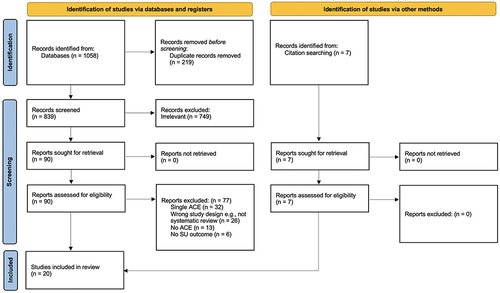
presents the PRISMA flow chartCitation21 of the study screening process. After duplicates were removed, 846 titles and abstracts were screened, and 97 full-text articles were assessed. Twenty articles met all eligibility criteria and were included in the evidence synthesis.Citation4,Citation22–40
Figure 1 PRISMA 2020 flow diagram. Study screening flow chart for studies identified in the umbrella review. Titles and abstracts were screened for 846 studies, resulting in 97 studies for full-text review. Of these, 20 studies were included in the current synthesis.
The evidence on associations between ACEs and substance misuse is robust and alarming. All reviews concluded that the majority of studies show an elevated risk of substance misuse or disorder, among adolescents and adults exposed to ACEs. Specific results are summarized below.
Umbrella Review of Systematic Reviews Employing Quantitative Synthesis
presents the study characteristics and estimates of the magnitude of the association between different levels of ACE exposure and alcohol, tobacco, and other drug use respectively, based on the six quantitative syntheses included in the current review.Citation4,Citation22,Citation25,Citation26,Citation34,Citation40 As shown, meta-analytic estimates demonstrate an increased pooled risk associated with just one ACE for harmful alcohol use, illicit drug use, and smoking.Citation22,Citation25,Citation26,Citation34 The strength of this association increases for those experiencing more than one ACE,Citation22,Citation25,Citation26,Citation34 which sadly represents the majority of children who experience any adversity.Citation17 For those experiencing four or more ACEs compared to no ACEs, the odds are markedly high for problematic alcohol use (OR=5.84), for illicit drug use (OR=5.62), and problematic drug use (OR=10.22).Citation25 Population attributable fractions (PAFs), that is, estimates of the proportion of an outcome that can be attributed to an exposure, indicate that in the US, approximately 13–29% of cases of drug use, 10–15% of harmful alcohol use, and 5–14% of cases of smoking can be attributed to ACEs.Citation4 At a population level, this corresponds to over 21 million people using illicit drugs, 10.5 million engaging in tobacco smoking, and 6.5 million engaging in harmful alcohol use.Citation4 In Europe, 15–45% of cases of drug use and 16–45% of harmful alcohol use were attributable to ACEs.Citation26
Table 1 Characteristics and Main Findings of Included Studies That Used Quantitative Synthesis to Examine the Relationship Between ACEs and Substance Misuse
Umbrella Review of Systematic Reviews Employing Qualitative Synthesis
Associations Between ACEs and Measures of Substance Misuse
presents the characteristics of included studies that examined the relationship between ACEs and substance misuse through qualitative synthesis. This relationship appears to hold across the spectrum of substance use behaviors, from age of initiation, consumption, and extending to harmful use, disorder, and dependence.Citation27,Citation29,Citation30 A recent review reported that all included studies found the development and severity of substance use disorder (SUD) to be positively associated with the number of ACEs,Citation29 and another review reported an average of those exposed to ACEs being 1.8 times more likely to have a SUD in adulthood.Citation33 Indeed, reviews report markedly higher prevalence rates of ACE exposure among those with a SUD compared to community estimates,Citation29 with between 85% and 100% of patients in treatment for SUD reporting at least one ACE compared to population estimates of between 46% and 62%.Citation29 Among adolescents in addiction treatment, a greater number of ACEs was associated with an earlier age of drug initiation.Citation29 ACEs were found to be associated with earlier onset of use and hazardous use of alcohol, and a shorter transition between the two.Citation30 Evidence is also consistent across substance types, although the bulk of research has been conducted on alcohol, tobacco, and cannabis. ACEs are associated with lifetime smoking, current smoking, heavy smoking, younger age of initiation, difficulty in smoking cessation.Citation27,Citation30 They show graded associations with alcohol and other drug outcomes, including early onset, heavy use, and disorder.Citation29,Citation30
Table 2 Characteristics and Main Findings of Included Studies That Used Qualitative Synthesis to Examine the Relationship Between ACEs and Substance Misuse
Associations Among Different Age Groups and Sex
While most studies have been conducted in adult samples, the existing evidence suggests a similar pattern among adolescent and young adult samples. Indeed, adolescence appears to be a critical developmental period during which the harmful effects of ACEs may manifest, due to biological and social changes as well as greater opportunity to use substances.Citation41–43 This burden appears to persist into adulthood, as evidenced by the large PAFs for childhood adversity and substance misuse among adults, highlighting the need for early intervention.Citation4,Citation26 Recent reviews have found that the positive associations between ACEs and substance misuse are evident by adolescence. Specifically, Hoffmann and Jones reviewed the literature on cumulative adversities and adolescent substance use, and found evidence of a positive association for initiation, frequency of use, disorder, and dependence.Citation24 Moreover, among young adults, Rogers et al found that greater ACEs predicted increased quantity and frequency of alcohol consumption, harmful alcohol use, and alcohol use disorder.Citation31 This was also confirmed for other drugs, with studies finding a positive association between ACEs and tobacco and e-cigarette use, cannabis dependence, other illicit drugs and non-medical prescription opioid use.Citation31
Sex differences are typically found in the prevalence of ACEs, with a higher prevalence and greater number of ACEs among females.Citation16,Citation34,Citation44 Evidence for sex-related differences in the link between ACEs and substance misuse is somewhat mixed, though tentatively suggests a stronger association between ACEs and substance misuse for females, compared to males. A review of longitudinal studies found that six out of 10 articles reported that the relationship between ACEs (specifically maltreatment) and substance misuse differed depending on sex.Citation28 Five of these found the relationship was stronger for women, compared to men; the remaining study found that sex moderated the relationship between sexual abuse only and drug use, with the association stronger for men compared to women.Citation28 A further study reported the test of sex differences was not significant, yet when models were run separately by sex only the relationship between maltreatment to drug use was significant for women, but not men.Citation28 Another included review found that several studies concluded stronger associations between cumulative adversity and substance use in adolescent females, compared to males.Citation24 Yet among young adults in a recent review, three of the five studies examining sex as a moderator of the ACE-substance misuse relationship found significant moderation, specifically, that the relationships between ACEs and alcohol use problems, illicit drug use, and e-cigarette use, were found to be stronger for males, compared to females.Citation31 Moreover, in a meta-analysis of the association between childhood maltreatment and SUD among bipolar disorder patients, meta-regression revealed the proportion of female participants in the sample did not change the effect size.Citation40
Associations Among Specific Populations and Social / Structural Factors Assessed
Six studies in the umbrella review examined the relationship between ACEs and substance misuse in specific populations: justice-involved youth; incarcerated adults; those with bipolar disorder; adults experiencing homelessness; and sexual minority populations. These reinforced the overall findings of this review. Among incarcerated adults, exposure to ACEs were associated with an increased likelihood of substance misuse, and earlier initiation of substance use.Citation35,Citation37 Similarly, among justice-involved youth a greater number of ACEs were associated with more substance use problems.Citation36 Childhood physical and sexual abuse were positively associated with alcohol dependence and other drug use among sexual minority youth.Citation39 Among patients with bipolar disorder, those with a history of childhood maltreatment had 1.84 times the odds of also experiencing a SUD and 1.44 times the odds of also experiencing an alcohol use disorder compared to bipolar disorder patients who did not experience childhood maltreatment.Citation40 Among adults experiencing homelessness, ACE exposure was associated with substance misuse.Citation38
While most of these studies acknowledged a greater prevalence of ACEs among socially disadvantaged or minority groups,Citation35,Citation36,Citation38,Citation39 there was little assessment of whether this affected the strength or manner of the association between ACEs and substance misuse. One systematic review examined social factors as mediating or moderating the relationship between ACEs and substance misuse.Citation23 ACE exposure was found to be associated with increased substance misuse through lower educational opportunity and achievement and involvement with the justice system.Citation23 Moreover, living in a neighborhood characterized by greater trust and social cohesion reduced the association between ACEs and alcohol misuse.Citation23
Systematic Reviews Examining Mechanisms in the Link Between ACEs and Substance Misuse
All studies included in a meta-synthesis of qualitative reviews examining the link between ACEs and addiction found that substance use served as a coping mechanism in an attempt to avoid feelings of low self-worth, depression, shame, and inadequacy arising from childhood adversity.Citation32 Another review focused on evidence from longitudinal studies identified a multitude of psychosocial mediators of the relationship between ACEs and substance misuse in adolescence and early adulthood.Citation23 This review reinforced the importance of coping motives, finding individuals exposed to ACEs more likely to endorse coping motives for substance use compared to non-exposed peers, in turn increasing substance misuse.Citation23 Internalizing symptoms (ie, of major depression, anxiety, post-traumatic stress) were commonly found to mediate the relationship between ACEs and substance misuse, including age of initiation and problem use,Citation23 and were also found to predict increased coping motives for drinking, further exacerbating substance misuse.Citation23 Externalizing symptoms (eg, behavioral disinhibition) were also found to mediate the relationship between ACEs and substance misuse, with ACEs predicting increased externalizing symptoms, which in turn predicted worse substance use outcomes, including age of initiation and disorder.Citation23 Moreover, interpersonal factors, such as parent and peer relationships, were commonly found to mediate the relationship between ACEs and substance misuse, highlighting that links between ACEs and substance misuse are dependent on social factors.Citation23
Limitations of Existing Research
Some important caveats arise when reviewing the existing literature. Firstly, while there is consistent evidence reporting positive associations between ACEs and substance misuse, there remain a number of studies reporting null or mixed findings on this relationship. Moreover, due to biases such as the file drawer problem, it is likely that some null associations have gone unpublished and are thus not reflected in the existing literature. While differences in methodology may go some way to accounting for null findings, it is also evident that certain factors confound the relationship between ACEs and substance misuse. These could both inflate and reduce the magnitude of associations between ACEs and substance misuse, with protective factors such as degree of social support reducing this association, and other factors associated with greater disadvantage, or social contributors to substance misuse such as peers or parental factors, strengthening the relationship between ACEs and substance misuse. Despite the inconsistency with some studies reporting null findings, there is an extraordinary number of rigorous studies that report positive associations between ACEs and substance misuse, highlighting the improbability that the association is an artefact of publication bias or unmeasured confounders. However, this issue highlights the importance of including the context in which ACEs occur to better understand the nuance in this relationship.
A second caveat is that of causality. The relationship between ACEs and substance misuse reviewed above is based on associations, yet it is often implied as causal. In addition, many of these associations are based on cross-sectional data, which cannot provide evidence on the hypothesized direction of association between ACEs and substance misuse, and which often finds a stronger association between ACEs and substance misuse compared to longitudinal studies.Citation24 Importantly, ACEs often co-occur in environments where the presence of other confounding factors can limit the ability to infer causality in the absence of rigorous study design. For example, parental alcohol use disorder can confer risk for offspring alcohol use problems through both genetic and environmental pathways, but living with a parent suffering an alcohol use disorder may also increase the risk of accumulating ACEs through reduced capacity of the parent to provide physical and emotional needs, as well as supervision.Citation45 However, it is also evident that many of the current methods used in quantitative causal inference, advanced from fieldssuch as biomedical research, do not adequately assess the upstream causal effects pertinent to the social determinants of health.Citation46 Rigid adherence to these methods typically engenders moving downstream toward proximal causes of disorder without appropriately taking into account the upstream social determinants causes that lead to the downstream factors.Citation46 Incorporating methodology advanced in the field of social epidemiology is an important future direction to strengthen causal claims in the relationship between ACEs and substance misuse. Meanwhile, diverging lines of evidence tentatively support the causal effects of ACEs on substance misuse. Firstly, prospective studies confirm the hypothesized temporal pathway with ACEs preceding substance misuse and mental illness.Citation47–50 Secondly, many studies adjusting for known and strongly associated covariates (parental mental illness, substance use, family conflict, divorce, sociodemographic factors, parental discipline) find that these relationships holdCitation45,Citation51 (although some do not, seeCitation52 for review). Third, studies on twins discordant for sexual abuse exposure demonstrate that the risk of alcohol use problems following sexual abuse holds above family background confounders, with a ratio of 2.8 for the exposed twin developing AUD to the non-exposed twin.Citation45 Finally, animal models support causal associations between early-life adversity and addiction.Citation51,Citation53
Discussion
The literature reviewed above suggests a robust link between ACEs and substance misuse, based on almost a quarter century of research. All articles identified by this umbrella review concluded that the majority of studies show an elevated risk of substance misuse, dependence or disorder, among adolescents and adults exposed to ACEs. Reviews confirmed a graded response between the number of ACEs experienced and the risk of substance misuse. A link between ACEs and substance misuse was supported for a range of outcomes, from age of initiation, harmful use, disorder, and dependence; as well as across adolescent, adult, male, and female populations. These findings highlight that clinical practice addressing substance use disorder must reflect trauma-informed care; that is, recognize the impact, signs, and symptoms of trauma, resist re-traumatizing those seeking treatment, and integrate understanding of trauma into practice and policies.Citation54
Why are ACEs Associated with Substance Misuse?
Only two studies included in the current review investigated the mechanisms that might explain the link between ACEs and substance misuse, finding support for the self-medication hypothesis and other psychological factors. There is also a vast literature examining neurobiological mechanisms linking experiences of early-life stress to substance misuse. In addition, genetic factors, including genes related to glucocorticoid functioning, serotonin transporting, and risk of alcohol dependence have been found to moderate the association between ACEs and substance misuse,Citation24,Citation52 and interact with environmental factors in the pathway from ACEs to substance misuse and disorder.Citation43,Citation51 Mechanisms linking ACEs and substance misuse appear to unfold on a continuum whereby severe and chronic stress caused by ACEs propels a cascade of effects across neurobiological, endocrine, immune, metabolic, and nervous systems, which impact psychosocial and cognitive functioning throughout childhood and adolescence, that in turn increase vulnerability to substance misuse and disorder. Such latent vulnerability to substance misuse may be triggered by subsequent stressors along the life course, with theoretical and empirical support for stress sensitization among those experiencing early life stress.Citation55–57 Importantly, the resilience demonstrated by many individuals exposed to ACEs highlights that the pathway from ACEs to substance misuse is undoubtedly complex and influenced by individual, social, and environmental factors.Citation43 This is critically important, as it highlights the multitude of potential intervention targets to prevent substance use problems following ACEs. Commonly proposed mechanisms linking ACEs and substance misuse are briefly reviewed below.
The Stress Response
One of the most commonly reviewed mechanisms as to how ACEs become biologically embedded centers on the hypothalamic–pituitary–adrenal (HPA) axis. The HPA axis coordinates release of the stress-response hormone, cortisol. In typical functioning of the HPA axis, cortisol is released in response to stress, and exerts a range of effects across immune, metabolic, and cardiovascular systems, which helps humans enact a fight or flight response.Citation53 After the threat has passed, cortisol levels return to normal, maintaining homeostasis in the HPA axis.Citation53 However, in cases of ongoing stress, such as adverse experiences in childhood, the downregulation of the HPA axis may be prevented, leading to hypersecretion of cortisol. This can result in what has been termed “allostatic load”, which, over the long-term may wear out this and other biological systems.Citation58
Dysregulation of the HPA axis may lead to either hypo- (ie, reduced) or hyper-secretion of cortisol. It is currently unclear why different studies find either hypo- or hyper-secretion of cortisol, though hypotheses and empirical investigations have pursued differences in the type, severity, timing, or recency of ACE exposure, the age of measurement of cortisol, the cortisol indicator measured, sex effects, and the presence of psychopathology such as depression.Citation59,Citation60 One prevailing view aligns with the Protection Hypothesis, which posits that HPA axis hyperactivity is observed in children but may subsequently transform into hypoactivity during later adolescence and adulthood in an attempt to protect brain regions from the damage from chronically elevated cortisol levels.Citation61–63 However, findings remain inconsistent across studies. The functioning of the HPA axis is undoubtedly complex, and rigorous attention to procedural and sample details will be required if we are to understand with greater precision how ACEs impact HPA axis functioning.
Despite these uncertainties, dysregulation of the HPA axis (both hypo- and hyper-activity) is implicated in substance misuse and disorder.Citation63,Citation64 It is possible these reflect multiple pathways to substance misuse, with researchers hypothesizing that those with a hyper-reactive HPA axis may be more likely to engage in substance use to dampen the resulting negative affect.Citation65,Citation66 The HPA axis interacts with brain regions and systems, such as the hippocampus, amygdala, pre-frontal cortex, and mesocorticolimbic dopaminergic pathway, involved in cognition, memory, impulse control, emotional regulation, threat, and reward processing. These structures and systems have a high density of cortisol receptors and even brief periods of exposure to stress appear sufficient to cause significant structural and functional alterations, including decreased neurogenesis in adulthood and atrophy caused by repeated stress.Citation58,Citation67 It is these structural and functional alterations that appear to confer vulnerability to substance misuse via a blunted response to natural reward coupled with a sensitized reward response to substances, as well as attention biases to threat processing at the expense of successful emotion regulation and cognitive functioning (explored in the following paragraphs). Heavy use of psychoactive substances can further alter the HPA axis, and these changes are associated with increased motivations to use substances and do so a higher levels.Citation64
The Reward System
It is recognized that differences in both behavioral and biological sensitivity to reward is a hallmark feature of substance-related problems. Both animal and human studies have demonstrated disruption to the reward system following early stress, typically finding reduced neural and behavioral sensitivity to natural (eg food) and monetary reward.Citation68 This is consistent with the blunted response to natural reward observed in humans with substance use disorder.Citation68 In humans, maltreated children showed greater impulsivity in reward tasks, insensitive to changing values of reward.Citation68 In humans, those exposed to ACEs show a stronger dopamine response to drugs, report greater pleasurable effects (eg euphoria), greater desire for more, and fewer negative effects of opioids compared to those non-exposed to ACEs, as well as a positive association between the number of adverse events in adulthood and dopamine response.Citation68,Citation69 These alterations may potentially enhance the rewarding effects of substances, increasing the risk of transitioning from controlled to compulsive use of substances, and help to explain severity of those presenting with substance use disorder with a history of ACEs.Citation63,Citation68 Indeed, differences in function and structure of these brain regions have been shown to mediate the relationship between ACEs and subsequent alcohol dependence.Citation63,Citation68 Animal models support a causal role of early-life stress on reward sensitivity, demonstrating enduring changes in the dopamine response to drugs following maternal separation or handling in rats.Citation43
Neurocognitive Pathways
Imaging evidence shows reduced grey matter volume in the pre-frontal cortex of children and adults who experienced ACEs, with corresponding deficits in emotion regulation, executive control, and memory.Citation68 These difficulties are strongly implicated in the development and maintenance of substance misuse and disorder.Citation70–72 Moreover, accumulating evidence suggests that altered threat processing may link ACEs and substance misuse. Children exposed to violence appear to be particularly wired to identify and respond to threat. They show an over-generalization of threat to non-threatening stimuli, biases in information processing toward prioritizing threat, greater amygdala reactivity to aversive stimuli, heightened emotional reactivity to potentially threatening cues, and altered emotion regulation in responding to threat.Citation73,Citation74 Adolescents exposed to ACEs displayed greater recruitment of effortful control from pre-frontal regions in response to negative stimuli compared to non-maltreated adolescents, yet it is postulated that the aforementioned deficits in pre-frontal control over amygdala reactivity may limit successful emotion regulation.Citation68 Together, these findings suggest ACEs result in neurological changes that facilitate rapid identification of threat at the expense of effective emotion regulation and adaptive emotional reactivity. Increasingly, studies are showing similar responses to threat and emotion processing among humans with substance use disorders.Citation68 Moreover, alcohol use acutely reduces amygdala reactivity to emotional cues and dampens connectivity between the amygdala and pre-frontal cortex, possibly contributing to motivations to use alcohol.Citation63,Citation68 Several studies have demonstrated an association between elevated amygdala reactivity and drug craving among those with substance use disorder, suggesting this may play an important role in conditioned stimulus associations and stress-related relapse.Citation68
Psychological Pathways
The self-medication hypothesis views substance use as an attempt to cope with or reduce negative affect.Citation75 However, the use of substances to cope may only temporarily alleviate negative emotions, and in fact can lead to greater negative affect and a cycle of comorbid mental health and substance use disorder.Citation76 ACEs are undoubtedly a significant source of distress and negative affect; therefore, self-medication is a pertinent theoretical mechanism linking ACEs to substance misuse and disorder. This was empirically supported by two systematic reviews in the current umbrella review.Citation23,Citation32 Relatedly, overarching coping styles, that is, the tendency toward certain cognitive and behavioral coping strategies when faced with stressors, may increase susceptibility to substance misuse. Coping styles develop early in life, through modelling and communication from interpersonal relationships, and are built and refined through a dynamic interplay between the person’s beliefs, values, genes, personality, and their social environment.Citation77,Citation78 This interplay between factors unique to an individual explain why the same event may be perceived and reacted to differently by two individuals.Citation77 Coping strategies characterized by avoidance (eg, denial, distraction) have been hypothesized as linking ACE exposure to substance misuse. Children exposed to ACEs may lack effective models of coping, or may employ avoidant styles of coping to facilitate survival and reduce the potential for harm in a traumatic environment that is beyond their ability to control.Citation78,Citation79 Evidence has found a greater tendency for maltreated adolescents to use avoidant coping strategies compared to non-exposed peers.Citation78,Citation80–82 Yet in the long-term, the use of avoidance to cope with stressors appears to confer risk for psychiatric symptoms, including substance misuse.Citation83 For example, children exposed to abuse are more likely to attempt to flee from stressors.Citation84 However, if the stressor is unavoidable, faced with threat these individuals display greater stress reactivity, as measured by amygdala response, and struggle to recruit the pre-frontal cortex to successfully regulate emotional response.Citation84 This stress reactivity is itself aversive, and coupled with the anxiolytic effects of some substances, may reinforce drug-related cravings and substance misuse. Indeed, avoidant coping has been found to mediate the association between ACEs and substance use in varying samples.Citation33,Citation85 Importantly, stress-process models postulate that ACEs lead to substance misuse to reduce negative affect when other coping resources are absent. Indeed, evidence suggests that the degree to which individuals use substances to cope depends on the availability of other resources that can be recruited to help individuals cope (eg, social support, self-control, emotion regulation).Citation24 Importantly, this advances the concept of resiliency as dependent on both individual and social-environmental resources and highlights a substantial opportunity for early intervention.Citation13
Within the current umbrella review, one systematic review was found that points to a multitude of intervention targets that can be addressed early in the life course. These include coping motives, internalizing symptoms, externalizing symptoms, and parent and peer relationships. Early intervention will be critical in reducing the burden of substance use problems, with evidence that childhood stress may increase vulnerability to early use of substances, which in itself shapes the susceptibility of the brain to substances, thereby further increasing the risk for addiction and disorder.Citation43,Citation51 This is supported by many studies finding that ACEs increase risk for early onset substance use, even after controlling for parental and peer confounding factors.Citation51 In turn, literature supports early initiation of substance use as a risk factor for disorder.Citation51
It is also important to note the potential for differential associations between ACEs and substance misuse depending on the specific ACE or type of ACE studied. While the current review focuses on cumulative trauma, there is growing theoretical and empirical support for a dimensional model of adversity, that separates experiences of threat (eg, abuse) and deprivation (eg, neglect) to understand more nuanced pathways linking ACEs to psychiatric outcomes.Citation19 For example, empirical evidence suggests that altered threat processing may arise from abuse, rather than neglect, and that pathways from neglect to psychopathology are more consistently characterized by alterations in executive function, cognition, and processing of social information.Citation73 There is also empirical support for different patterns of activation in reward learning for children exposed to threat, versus deprivation.Citation73 These findings suggest that despite similar presentations, effective interventions to prevent or treat substance misuse might be different depending on the type of adversity experienced. Accumulating research is examining these nuances to improve our understanding of how best to intervene. Other research has examined the synergistic effects of certain pairs of ACEs, finding the strongest increases in the probability of internalizing and externalizing disorders for women when sexual abuse was experienced in tandem with domestic violence or household mental illness, or household substance misuse was experienced with physical abuse.Citation86 For men, experiencing household mental illness and household substance misuse or sexual abuse increased the probability of disorder, as did the combination of physical abuse and domestic violence.Citation86 Further research has examined associations between each specific ACE and substance misuse, finding the strongest predictors for adult substance misuse to be emotional abuse, household substance misuse, and household mental illness,Citation87 and deprivation less robustly associated with substance misuse among young adults.Citation88 However, here it is important to consider ACEs cumulatively and independently, rather than relying on one method, given the inter-relationship and co-occurrence of multiple adversity types.Citation87 Findings of the current umbrella review should be interpreted with the context that the ACEs assessed are skewed towards experiences of threat, particularly physical and sexual abuse. This reflects a long-term bias in the existing literature, which may mean that our understanding of the link between ACEs and substance misuse is predominantly reflective of the link between abuse and substance misuse. Conclusions arising from the current review may be less generalizable to experiences of deprivation or other ACEs. Future research must examine the mechanisms linking ACEs and substance misuse with more attention to the type of exposure, with the hope to harness these more nuanced findings in order to develop tailored interventions to prevent and treat ACE-related substance misuse.
Where Do We Go from Here?
The ACEs literature has been critiqued as oversimplistic and reductionist in decontextualizing childhood adversity from broader structural issues and focusing solely on individuals or families.Citation13 Given the wealth of evidence reporting associations between ACEs and substance misuse as summarized by the current umbrella review, future research must seriously address the limitations of the current evidence base or examine the mechanisms that explain this link to advance the field, rather than continuing to identify associations between ACEs and substance use outcomes. In this way, research can inform the development of effective interventions to prevent substance use problems among those exposed to ACEs, at both policy and practice levels.
Addressing limitations in the ACEs literature will most notably require thorough recognition that the link between ACEs and substance misuse is influenced by the socio-cultural context in which this relationship occurs. There was virtually no assessment of this in the included reviews, highlighting that this issue has been severely neglected compared to the wealth of literature demonstrating overall associations between ACEs and substance misuse. Critiques of the ACEs and health outcomes literature have identified that ACE exposure is commonly decontextualized from broader social, economic, and structural conditions,Citation13 and that ACEs may be better conceptualized as manifestations of poverty, deprivation, and social and gender inequality which have long been shown to affect health and opportunity across the life course.Citation89 Critics argue that the narrative that ACEs lead to poor health and disadvantage, rather than being manifestations of it, has contributed to focusing on individuals and families as the required target for intervention.Citation89 Broader social and structural determinants of health influence both the occurrence of ACEs and the risk of substance misuse arising from exposure, and must be addressed to improve the outcomes of those who have experienced ACEs. This growing recognition is an important shift toward attributing responsibility to structures and systems rather than on individuals and families, which has implicitly dominated the intervention landscape over the last 25 years. For example, evidence indicates that children of Indigenous parents with alcohol use problems show 2–3 times greater odds of alcohol use and problem drinking compared to children of non-Indigenous parents with alcohol use problems.Citation90
Structural barriers that account for these disparities in the health impacts of ACEs should form targets for intervention. This will critically require policy-driven approaches fueled by recognition that both the social distribution of ACEs and means to mitigate their impacts are products of social inequality. Ensuring health care is accessible to all, reducing barriers to accessing care associated with stigma, language, and cultural sensitivity, and incorporating cultural assets into prevention and treatment approaches may be critical in addressing the link between ACEs and substance misuse.Citation31 However, even when receiving equal access to care, recent research has found poorer treatment outcomes for depression among more disadvantaged groups.Citation91 The differential exposure hypothesis posits that these observed social inequalities in health arise from variation in levels of exposure to stressors, and highlights that the efficacy of treating an individual in clinical practice may be limited until broader structural changes are meaningfully addressed through policy and public health. While ACEs are experienced by all creeds, they are not randomly distributed across the population. The prevalence of ACEs is concentrated among marginalized groups, such as low-income earners, those with no or limited access to health insurance, minority sexual orientation, racial/ethnic minority groups,Citation92,Citation93 and in counties of greater deprivation.Citation94 This greater prevalence of ACEs reflects structural inequalities, such as disproportionate rates of incarceration among Black and Indigenous populations or greater financial strain among low-income earners and marginalized groups.Citation95,Citation96 The disproportionate contact of the justice system with minority race/ethnicities may compound the deleterious effect of ACEs on a range of health, legal, and economic outcomes, including substance misuse. Moreover, ACEs occur in addition to stressors related to discrimination, poverty, and racism. Thus, addressing the compounding syndemics of ACEs and other social determinants of health, and the systems that underlie the inequities in these exposures will undoubtedly be critical in the prevention and treatment of substance misuse and disorder as well as public health more broadly.
Future research should interrogate how the mechanisms linking ACEs and substance misuse differ depending on the socio-economic context, or demographic factors, such as sex differences. Mechanisms operating between ACEs and substance misuse are the key to developing interventions to prevent and treat substance misuse among those exposed to ACEs, as such, understanding moderating factors would help to maximize the efficacy of these approaches. For example, safe and supportive interpersonal relationships in both childhood and adulthood can buffer the impact of ACEs on mental health and substance misuse.Citation97–99 There is evidence that these positive relationships may model effective coping strategies and help to undo dysregulation in the stress system.Citation63 There may also be sex differences in the mechanisms linking ACEs to substance misuse. Research has found that externalizing symptoms and enhancement motives for substance use are mechanisms for males, whereas internalizing symptoms and coping motivates, as well as externalizing symptoms, may be mechanisms for females.Citation63 Moreover, female internalizing symptoms in response to a stressor predicted subsequent drug use, whereas for males it was a blunted autonomic nervous system measure that predicted drug use in response to the same stressor.Citation64 Better understanding of these nuances will be critical in the development of prevention and treatment approaches to address the link between ACEs and substance misuse. Effective substance misuse prevention programs exist,Citation100,Citation101 but it is critical these adopt a trauma-informed approach and establish efficacy among those exposed to ACEs. Encouragingly, previously independent approaches to treating substance use disorder and traumatic stress are just beginning to be integrated,Citation102–104 reflecting increased awareness of the critical importance of trauma-informed prevention and treatment of substance use disorders.Citation11 More rigorous research in developing, evaluating, and implementing effective interventions for young people that take into account the findings from this umbrella review is needed.
Conclusions
Evidence from almost 25 years of ACEs research converges on ACEs as strong and consistent risk factors for subsequent substance misuse and disorder. ACEs account for 13–29% of cases of drug use, 10–15% of harmful alcohol use, and 5–14% of cases of smoking in the US, and 15–45% of cases of drug use and 16–45% of harmful alcohol use in Europe.Citation4,Citation26 However, this link is undoubtedly complex, and shaped by a multitude of individual, social, and structural factors, that interact with each other in the risk for substance use problems. Importantly, many children exposed to ACEs show remarkable resilience in the face of adversity, highlighting the multifaceted nature of risk and the multitude of potential intermediary factors that can be harnessed to prevent substance misuse and disorder. Research that seeks to holistically understand and address the relationship between ACEs and substance misuse within the broader social determinants of health, incorporating a broad range of risk and protective factors, is a crucial future direction.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- McLellan AT. Substance misuse and substance use disorders: why do they matter in healthcare? Trans Am Clin Climatol Assoc. 2017;128:112–130.
- Degenhardt L, Charlson F, Ferrari A, et al. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5(12):987–1012. doi:10.1016/S2215-0366(18)30337-7
- Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(1_suppl2):19–31. doi:10.1177/00333549141291S206
- Grummitt LR, Kreski NT, Kim SG, Platt J, Keyes KM, McLaughlin KA. Association of Childhood adversity with morbidity and mortality in US adults: a systematic review. JAMA Pediatr. 2021. doi:10.1001/jamapediatrics.2021.2320
- Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi:10.1016/s0749-3797(98)00017-8
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics. 2003;111(3):564. doi:10.1542/peds.111.3.564
- Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282(17):1652–1658. doi:10.1001/jama.282.17.1652
- Magruder KM, McLaughlin KA, Elmore Borbon DL. Trauma is a public health issue. Eur J Psychotraumatol. 2017;8(1):1375338. doi:10.1080/20008198.2017.1375338
- Finkelhor D, Shattuck A, Turner HA, Hamby SL. Trends in children’s exposure to violence, 2003 to 2011. JAMA Pediatr. 2014;168(6):540–546. doi:10.1001/jamapediatrics.2013.5296
- Hanson RF, Lang J, Critical Look A. At trauma-informed care among agencies and systems serving maltreated youth and their families. Child Maltreat. 2016;21(2):95–100. doi:10.1177/1077559516635274
- Purkey E, Patel R, Phillips SP. Trauma-informed care: better care for everyone. Can Fam Physician. 2018;64(3):170–172.
- Grummitt L, Keyes K, Rajan S, Kelly EV, Barrett EL, Newton NC. Clusters of adversity types among U.S. youth: associations with mental health. Am J Prev Med. 2022;63(3):331–340. doi:10.1016/j.amepre.2022.03.016
- McEwen CA, Gregerson SF. A critical assessment of the adverse childhood experiences study at 20 years. Am J Prev Med. 2019;56(6):790–794. doi:10.1016/j.amepre.2018.10.016
- Asmussen K, Fischer F, Drayton E, McBride T. Adverse childhood experiences: what we know, what we don’t know, and what should happen next; 2020. Available from: https://www.eif.org.uk/report/adverse-childhood-experiences-what-we-know-what-we-dont-know-and-what-should-happen-next. Accessed November 9, 2022.
- Struck S, Stewart-Tufescu A, Asmundson AJN, Asmundson GGJ, Afifi TO. Adverse childhood experiences (ACEs) research: a bibliometric analysis of publication trends over the first 20 years. Child Abuse Negl. 2021;112:104895. doi:10.1016/j.chiabu.2020.104895
- Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of adverse childhood experiences from the 2011–2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatr. 2018;172(11):1038–1044. doi:10.1001/jamapediatrics.2018.2537
- McLaughlin KA, Greif Green J, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Arch Gen Psychiatry. 2012;69(11):1151–1160. doi:10.1001/archgenpsychiatry.2011.2277
- McEwen BS, Gianaros PJ. Stress- and allostasis-induced brain plasticity. Annu Rev Med. 2011;62:431–445. doi:10.1146/annurev-med-052209-100430
- McLaughlin KA, Sheridan MA. Beyond cumulative risk: a dimensional approach to childhood adversity. Curr Dir Psychol Sci. 2016;25(4):239–245. doi:10.1177/0963721416655883
- Lewis P. Australian Guidelines to Reduce Health Risks from Drinking Alcohol. National Health and Medical Research Council; 2020.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
- Bellis MA, Hughes K, Ford K, Ramos Rodriguez G, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health. 2019;4(10):e517–e528. doi:10.1016/S2468-2667(19)30145-8
- Grummitt L, Kelly E, Barrett E, Keyes K, Newton N. Targets for intervention to prevent substance use in young people exposed to childhood adversity: a systematic review. PLoS One. 2021;16(6):e0252815. doi:10.1371/journal.pone.0252815
- Hoffmann JP, Jones MS. Cumulative stressors and adolescent substance use: a review of 21st-century literature. Trauma Violence Abuse. 2020;1524838020979674. doi:10.1177/1524838020979674
- Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e356–e366. doi:10.1016/S2468-2667(17)30118-4
- Hughes K, Ford K, Bellis MA, Glendinning F, Harrison E, Passmore J. Health and financial costs of adverse childhood experiences in 28 European countries: a systematic review and meta-analysis. Lancet Public Health. 2021;6(11):e848–e857. doi:10.1016/S2468-2667(21)00232-2
- Kalmakis KA, Chandler GE. Health consequences of adverse childhood experiences: a systematic review. J Am Assoc Nurse Pract. 2015;27(8):457–465. doi:10.1002/2327-6924.12215
- Kristman-Valente A, Wells EA. The role of gender in the association between child maltreatment and substance use behavior: a systematic review of longitudinal research from 1995 to 2011. Subst Use Misuse. 2013;48(8):645–660. doi:10.3109/10826084.2013.800115
- Leza L, Siria S, López-Goñi JJ, Fernández-Montalvo J. Adverse childhood experiences (ACEs) and substance use disorder (SUD): a scoping review. Drug Alcohol Depend. 2021;221:108563. doi:10.1016/j.drugalcdep.2021.108563
- Ports KA, Holman DM, Guinn AS, et al. Adverse childhood experiences and the presence of cancer risk factors in adulthood: a scoping review of the literature from 2005 to 2015. J Pediatr Nurs Jan-Feb. 2019;44:81–96. doi:10.1016/j.pedn.2018.10.009
- Rogers CJ, Pakdaman S, Forster M, et al. Effects of multiple adverse childhood experiences on substance use in young adults: a review of the literature. Drug Alcohol Depend. 2022;234:109407. doi:10.1016/j.drugalcdep.2022.109407
- Teixeira CAB, Lasiuk G, Barton S, Fernandes M, Gherardi-Donato E. An exploration of addiction in adults experiencing early-life stress: a metasynthesis. Rev Lat Am Enfermagem. 2017;25:e2939–e2939. doi:10.1590/1518-8345.2026.2939
- De Venter M, Demyttenaere K, Bruffaerts R. Het verband tussen traumatische gebeurtenissen in de kindertijd en angst, depressie en middelenmisbruik in de volwassenheid; een systematisch literatuuroverzicht [The relationship between adverse childhood experiences and mental health in adulthood. A systematic literature review]. Tijdschr Psychiatr. 2013;55(4):259–268.
- Petruccelli K, Davis J, Berman T. Adverse childhood experiences and associated health outcomes: a systematic review and meta-analysis. Child Abuse Negl. 2019;97:104127. doi:10.1016/j.chiabu.2019.104127
- Bowen K, Jarrett M, Stahl D, Forrester A, Valmaggia L. The relationship between exposure to adverse life events in childhood and adolescent years and subsequent adult psychopathology in 49,163 adult prisoners: a systematic review. Pers Individ Dif. 2018;131:74–92. doi:10.1016/j.paid.2018.04.023
- Folk JB, Kemp K, Yurasek A, Barr-Walker J, Tolou-Shams M. Adverse childhood experiences among justice-involved youth: data-driven recommendations for action using the sequential intercept model. Am Psychologist. 2021;76:268–283. doi:10.1037/amp0000769
- Goddard T, Pooley JA. The impact of childhood abuse on adult male prisoners: a systematic review. J Police Crim Psychol. 2019;34(2):215–230. doi:10.1007/s11896-018-9260-6
- Liu M, Luong L, Lachaud J, Edalati H, Reeves A, Hwang SW. Adverse childhood experiences and related outcomes among adults experiencing homelessness: a systematic review and meta-analysis. Lancet Public Health. 2021;6(11):e836–e847. doi:10.1016/S2468-2667(21)00189-4
- McGeough BL, Sterzing PR. A systematic review of family victimization experiences among sexual minority youth. J Prim Prev. 2018;39(5):491–528. doi:10.1007/s10935-018-0523-x
- Agnew-Blais J, Danese A. Childhood maltreatment and unfavourable clinical outcomes in bipolar disorder: a systematic review and meta-analysis. Lancet Psychiatry. 2016;3(4):342–349. doi:10.1016/s2215-0366(15)00544-1
- Blakemore S-J, Mills KL. Is adolescence a sensitive period for sociocultural processing? Ann Rev Psychol. 2014;65(1):187–207. doi:10.1146/annurev-psych-010213-115202
- Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10(6):434–445. doi:10.1038/nrn2639
- Enoch M-A. The influence of gene-environment interactions on the development of alcoholism and drug dependence. Curr Psychiatry Rep. 2012;14(2):150–158. doi:10.1007/s11920-011-0252-9
- Cole AB, Armstrong CM, Giano ZD, Hubach RD. An update on ACEs domain frequencies across race/ethnicity and sex in a nationally representative sample. Child Abuse Negl. 2022;129:105686. doi:10.1016/j.chiabu.2022.105686
- Sartor CE, Agrawal A, McCutcheon VV, Duncan AE, Lynskey MT. Disentangling the complex association between childhood sexual abuse and alcohol-related problems: a review of methodological issues and approaches. J Stud Alcohol Drugs. 2008;69(5):718–727. doi:10.15288/jsad.2008.69.718
- Robinson WR, Bailey ZD. Invited commentary: what social epidemiology brings to the table-reconciling social epidemiology and causal inference. Am J Epidemiol. 2020;189(3):171–174. doi:10.1093/aje/kwz197
- Abajobir AA, Najman JM, Williams G, Strathearn L, Clavarino A, Kisely S. Substantiated childhood maltreatment and young adulthood cannabis use disorders: a pre-birth cohort study. Psychiatry Res. 2017;256:21–31. doi:10.1016/j.psychres.2017.06.017
- Clark C, Caldwell T, Power C, Stansfeld SA. Does the influence of childhood adversity on psychopathology persist across the lifecourse? A 45-year prospective epidemiologic study. Ann Epidemiol. 2010;20(5):385–394. doi:10.1016/j.annepidem.2010.02.008
- Gondek D, Patalay P, Lacey RE. Adverse childhood experiences and multiple mental health outcomes through adulthood: a prospective birth cohort study. SSM Mental Health. 2021;1:100013. doi:10.1016/j.ssmmh.2021.100013
- Kisely S, Strathearn L, Najman J. The influence of child maltreatment on substance or alcohol use in 30-year-old adults: a birth cohort study. Drug Alcohol Rev. 2020. doi:10.1111/dar.13192
- Enoch MA. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology. 2011;214(1):17–31. doi:10.1007/s00213-010-1916-6
- Keyes KM, Hatzenbuehler ML, Hasin DS. Stressful life experiences, alcohol consumption, and alcohol use disorders: the epidemiologic evidence for four main types of stressors. Psychopharmacology. 2011;218(1):1–17. doi:10.1007/s00213-011-2236-1
- Hertzman C, Boyce T. How experience gets under the skin to create gradients in developmental health. Annu Rev Public Health. 2010;31:329–473pfollowing 347. doi:10.1146/annurev.publhealth.012809.103538
- Huang LN, Flatow R, Biggs T, et al. SAMHSA’s concept of trauma and guidance for a trauma-informed approach; 2014.
- McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol Med. 2010;40(10):1647–1658. doi:10.1017/S0033291709992121
- Hammen C, Henry R, Daley SE. Depression and sensitization to stressors among young women as a function of childhood adversity. J Consult Clin Psychol. 2000;68(5):782–787.
- Glaser JP, van Os J, Portegijs PJ, Myin-Germeys I. Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. J Psychosom Res. 2006;61(2):229–236. doi:10.1016/j.jpsychores.2006.04.014
- McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179. doi:10.1056/NEJM199801153380307
- Raymond C, Marin M-F, Wolosianski V, et al. Early childhood adversity and HPA axis activity in adulthood: the importance of considering minimal age at exposure. Psychoneuroendocrinology. 2021;124:105042. doi:10.1016/j.psyneuen.2020.105042
- Bernard K, Frost A, Bennett CB, Lindhiem O. Maltreatment and diurnal cortisol regulation: a meta-analysis. Psychoneuroendocrinology. 2017;78:57–67. doi:10.1016/j.psyneuen.2017.01.005
- Fries E, Hesse J, Hellhammer J, Hellhammer DH. A new view on hypocortisolism. Psychoneuroendocrinology. 2005;30(10):1010–1016. doi:10.1016/j.psyneuen.2005.04.006
- Koss KJ, Gunnar MR. Annual research review: early adversity, the hypothalamic–pituitary–adrenocortical axis, and child psychopathology. J Child Psychol Psychiatry. 2018;59(4):327–346. doi:10.1111/jcpp.12784
- Kirsch DE, Lippard ETC. Early life stress and substance use disorders: the critical role of adolescent substance use. Pharmacol Biochem Behav. 2022;215:173360. doi:10.1016/j.pbb.2022.173360
- Milivojevic V, Sinha R. Central and peripheral biomarkers of stress response for addiction risk and relapse vulnerability. Trends Mol Med. 2018;24(2):173–186. doi:10.1016/j.molmed.2017.12.010
- Andersen SL, Teicher MH. Stress, sensitive periods and maturational events in adolescent depression. Trends Neurosci. 2008;31(4):183–191. doi:10.1016/j.tins.2008.01.004
- Andersen SL, Teicher MH. Desperately driven and no brakes: developmental stress exposure and subsequent risk for substance abuse. Neurosci Biobehav Rev. 2009;33(4):516–524. doi:10.1016/j.neubiorev.2008.09.009
- Berens AE, Jensen SKG, Nelson CA. Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC Med. 2017;15(1):135. doi:10.1186/s12916-017-0895-4
- Puetz VB, McCrory E. Exploring the relationship between childhood maltreatment and addiction: a review of the neurocognitive evidence. Curr Addict Rep. 2015;2(4):318–325. doi:10.1007/s40429-015-0073-8
- Carlyle M, Broomby R, Simpson G, et al. A randomised, double-blind study investigating the relationship between early childhood trauma and the rewarding effects of morphine. Addict Biol. 2021;26(6):e13047. doi:10.1111/adb.13047
- Lovallo WR. Early life adversity reduces stress reactivity and enhances impulsive behavior: implications for health behaviors. Int J Psychophysiol. 2013;90(1):8–16. doi:10.1016/j.ijpsycho.2012.10.006
- Cheetham A, Allen NB, Yücel M, Lubman DI. The role of affective dysregulation in drug addiction. Clin Psychol Rev. 2010;30(6):621–634. doi:10.1016/j.cpr.2010.04.005
- Boness CL, Watts AL, Moeller KN, Sher KJ. The etiologic, theory-based, ontogenetic hierarchical framework of alcohol use disorder: a translational systematic review of reviews. Psychol Bull. 2021;147(10):1075–1123. doi:10.1037/bul0000333
- McLaughlin KA, Weissman D, Bitrán D. Childhood adversity and neural development: a systematic review. Annual Rev Dev Psychol. 2019;1(1):277–312. doi:10.1146/annurev-devpsych-121318-084950
- McLaughlin KA, Sheridan MA, Gold AL, et al. Maltreatment exposure, brain structure, and fear conditioning in children and adolescents. Neuropsychopharmacology. 2016;41(8):1956–1964. doi:10.1038/npp.2015.365
- Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry. 1997;4(5):231–244. doi:10.3109/10673229709030550
- Blume AW, Schmaling KB, Marlatt GA. Revisiting the self-medication hypothesis from a behavioral perspective. Cogn Behav Pract. 2000;7(4):379–384. doi:10.1016/S1077-7229(00)80048-6
- Lazarus RS, Folkman S. Stress, Appraisal, and Coping. Springer publishing company; 1984.
- Gruhn MA, Compas BE. Effects of maltreatment on coping and emotion regulation in childhood and adolescence: a meta-analytic review. Child Abuse Negl. 2020;103:104446. doi:10.1016/j.chiabu.2020.104446
- Wadsworth ME. Development of maladaptive coping: a functional adaptation to chronic, uncontrollable stress. Child Dev Perspect. 2015;9(2):96–100. doi:10.1111/cdep.12112
- Fortier MA, DiLillo D, Messman-Moore TL, Peugh J, DeNardi KA, Gaffey KJ. Severity of child sexual abuse and revictimization: the mediating role of coping and trauma symptoms. Psychol Women Q. 2009;33(3):308–320. doi:10.1111/j.1471-6402.2009.01503.x
- Milojevich HM, Levine LJ, Cathcart EJ, Quas JA. The role of maltreatment in the development of coping strategies. J Appl Dev Psychol. 2018;54:23–32. doi:10.1016/j.appdev.2017.10.005
- Hébert M, Smith K, Caouette J, et al. Prevalence and associated mental health outcomes of child sexual abuse in youth in France: observations from a convenience sample. J Affect Disord. 2021;282:820–828. doi:10.1016/j.jad.2020.12.100
- Compas BE, Jaser SS, Bettis AH, et al. Coping, emotion regulation, and psychopathology in childhood and adolescence: a meta-analysis and narrative review. Psychol Bull. 2017;143(9):939–991. doi:10.1037/bul0000110
- Taylor SE. Mechanisms linking early life stress to adult health outcomes. Proc Natl Acad Sci. 2010;107(19):8507. doi:10.1073/pnas.1003890107
- Min M, Farkas K, Minnes S, Singer LT. Impact of childhood abuse and neglect on substance abuse and psychological distress in adulthood. J Trauma Stress. 2007;20(5):833–844. doi:10.1002/jts.20250
- Putnam KT, Harris WW, Putnam FW. Synergistic childhood adversities and complex adult psychopathology. J Trauma Stress. 2013;26(4):435–442. doi:10.1002/jts.21833
- Merrick MT, Ports KA, Ford DC, Afifi TO, Gershoff ET, Grogan-Kaylor A. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse Negl. 2017;69:10–19. doi:10.1016/j.chiabu.2017.03.016
- Grummitt LR, Kelly EV, Barrett EL, et al. Associations of childhood emotional and physical neglect with mental health and substance use in young adults. Aust N Z J Psychiatry. 2021;56(4):365–375. doi:10.1177/00048674211025691
- Hartas D. Assessing the foundational studies on adverse childhood experiences. Socl Policy Soc. 2019;18(3):435–443. doi:10.1017/S1474746419000034
- Owais S, Faltyn M, Zou H, et al. Psychopathology in the Offspring of Indigenous Parents with Mental Health Challenges: a Systematic Review: psychopathologie des descendants de parents autochtones ayant des problèmes de santé mentale: une revue systématique. Can J Psychiatry. 2021;66(6):517–536. doi:10.1177/0706743720966447
- Mills JA, Suresh V, Chang L, et al. Socioeconomic predictors of treatment outcomes among adults with major depressive disorder. Psychiatr Serv. 2022:appips202100559. doi:10.1176/appi.ps.202100559
- Strompolis M, Tucker W, Crouch E, Radcliff E. The intersectionality of adverse childhood experiences, race/ ethnicity, and income: implications for policy. J Prev Interv Community. 2019;47(4):310–324. doi:10.1080/10852352.2019.1617387
- Nurius PS, Green S, Logan-Greene P, Longhi D, Song C. Stress pathways to health inequalities: embedding ACEs within social and behavioral contexts. Int Public Health J. 2016;8(2):241–256.
- Kurani S, Webb L, Cadet K, et al. Area-level deprivation and adverse childhood experiences among high school students in Maryland. BMC Public Health. 2022;22(1):811. doi:10.1186/s12889-022-13205-w
- Mauer M. Addressing racial disparities in incarceration. Prison J. 2011;91(3_suppl):87S–101S. doi:10.1177/0032885511415227
- Conrad-Hiebner A, Byram E. The temporal impact of economic insecurity on child maltreatment: a systematic review. Trauma Violence Abuse. 2018;21(1):157–178. doi:10.1177/1524838018756122
- Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. Positive childhood experiences and adult mental and relational health in a statewide sample: associations across adverse childhood experiences levels. JAMA Pediatr. 2019;173(11):e193007–e193007. doi:10.1001/jamapediatrics.2019.3007
- Jaffee SR, Takizawa R, Arseneault L. Buffering effects of safe, supportive, and nurturing relationships among women with childhood histories of maltreatment. Psychol Med. 2017;47(15):2628–2639. doi:10.1017/S0033291717001027
- Bellis MA, Hardcastle K, Ford K, et al. Does continuous trusted adult support in childhood impart life-course resilience against adverse childhood experiences - a retrospective study on adult health-harming behaviours and mental well-being. BMC Psychiatry. 2017;17(1):110. doi:10.1186/s12888-017-1260-z
- Edalati H, Conrod PJ. A review to identify gaps in research and service delivery for substance use prevention among at-risk adolescents involved in child welfare system: the promises of targeted interventions. Int J Child Adolesc Resilience. 2017;5(1):20–39.
- Teesson M, Newton NC, Slade T, et al. Combined universal and selective prevention for adolescent alcohol use: a cluster randomized controlled trial. Psychol Med. 2017;47(10):1761–1770. doi:10.1017/S0033291717000198
- Danielson CK, Adams Z, McCart MR, et al. Safety and efficacy of exposure-based risk reduction through family therapy for co-occurring substance use problems and posttraumatic stress disorder symptoms among adolescents: a randomized clinical trial. JAMA Psychiatry. 2020;77(6):574–586. doi:10.1001/jamapsychiatry.2019.4803
- Fortuna LR, Porche MV, Padilla A. A treatment development study of a cognitive and mindfulness-based therapy for adolescents with co-occurring post-traumatic stress and substance use disorder. Psychol Psychother. 2018;91(1):42–62. doi:10.1111/papt.12143
- Schollar-Root O, Cassar J, Peach N, et al. Integrated trauma-focused psychotherapy for traumatic stress and substance use: two adolescent case studies. Clin Case Stud. 2021;21(3):192–208. doi:10.1177/15346501211046054
