Abstract
Carotid artery stenting is an effective treatment for ischemic stroke patients with moderate-to-severe carotid artery stenosis. However, the midterm outcome for patients undergoing this procedure varies considerably with baseline characteristics. To determine the impact of baseline characteristics on outcomes following carotid artery stenting, data from 107 eligible patients with a first episode of ischemic stroke were collected by retrospective chart review. A modified Rankin Scale (mRS) was used to divide patients into two baseline groups, mRS ≤2 and mRS >2. A three-step decision-tree statistical analysis was conducted. After weighting the decision-tree parameters, the following impact hierarchy was obtained: admission low-density lipoprotein, gouty arthritis, chronic kidney disease, ipsilateral common carotid artery resistance index, contralateral ophthalmic artery resistance index, sex, and dyslipidemia. The finite-state machine model demonstrated that, in patients with baseline mRS ≤2, 46% had an improved mRS score at follow-up, whereas 54% had a stable mRS score. In patients with baseline mRS >2, a stable mRS score was observed in 75%, improved score in 23%, and a poorer score in 2%. Admission low-density lipoprotein was the strongest predictive factor influencing poststenting outcome. In addition, our study provides further evidence that carotid artery stenting can be of benefit in first-time ischemic stroke patients with baseline mRS scores >2.
Background
Stroke is a leading cause of morbidity and mortality in modern society.Citation1 On the basis of the TOAST (trial of ORG 10172 in acute stroke treatment) criteria,Citation1–Citation3 moderate-to-severe carotid stenosis is the most commonly reported cause of stroke,Citation1–Citation4 especially if the carotid lumen reduction is >50%.Citation2,Citation3,Citation5 This is in part because carotid stenosis can be screened by noninvasive carotid duplex examination and the stenosis can be treated effectively through carotid artery stenting.Citation6
Stroke can cause irreversible neurological deficits, and identification of the underlying mechanism is vital to reduce the likelihood of recurrence. In people >65 years, the incidence of extracranial carotid stenosis with >50% lumen reduction is over 5%. The risk of ipsilateral stroke increases with increasing degree of stenosis, and the rate is estimated at 1%–5% per year when stenosis is >50%.Citation6 There have also been reports that the incidence of stroke may be higher in Taiwanese and Chinese populations compared to European populations.Citation7,Citation8
Following initial ischemic stroke, there is a high risk of recurrence. Stroke severity, age, and degree of stenosis have all been shown to be predictive of recurrence.Citation9,Citation10 It is estimated that the risk of recurrence in the first month following initial stroke is 4% and in the first year is 12%.Citation9 One Taiwanese-based study with a 2.5-year follow-up duration found that the cumulative recurrence rate was 10.5%.Citation11 There are a number of treatment options available, including medical treatment, lifestyle interventions, and surgical interventions such as carotid artery stenting and carotid endarterectomy. A physician must weigh the risks and benefits based upon the degree of stenosis, severity of stroke, age of the patient, and other available baseline characteristics.Citation12
Carotid artery stenting can effectively prevent secondary stroke, ameliorate atherosclerosis, and restore blood supply to the brain parenchyma.Citation2,Citation3,Citation5 The current guidelineCitation13 recommends carotid stenting for carotid stenosis patients when the diameter of the lumen is reduced by >70% if assessed by noninvasive imaging or >50% if assessed by catheter-based imaging. Although the efficacy of carotid artery stenting is recognized in the literature, the outcomes for patients undergoing this procedure are heterogeneous, and it may be associated with significant morbidity.Citation14,Citation15 Appropriate guidance for first-line clinicians to assist in appropriate decision-making regarding stenting is unavailable in the literature, which prompted us to undertake this study.
Furthermore, the correlation between different baseline physical characteristics and midterm outcomes has not been established, resulting in a lack of objective clinical references. The primary aim of this study was, therefore, to develop a model to integrate patients’ baseline characteristics and carotid ultrasound data and determine their impact on outcomes following carotid artery stenting, as assessed by the modified Rankin Scale (mRS).
Materials and methods
Patient identification
Patients with a first episode of ischemic stroke were identified retrospectively using data procedure codes for carotid artery stenting recorded by the angiography laboratory of the Department of Neuroimaging, Chunghua Christian Hospital, Taiwan. Patients who underwent carotid artery stenting at Chunghua Christian Hospital, Taiwan, between January 2010 and July 2014 and were aged >18 years were eligible for inclusion. Inclusion criteria were initial ischemic stroke, carotid stenosis with >50% lumen reduction by angiography, stroke primarily due to carotid stenosis (with minimal or no other etiologies that could be well explained in the index event), no evidence of recurrent stroke, minimal or no rehabilitation treatment after the stenting procedure, and follow-up available for at least 1 year after stenting. Exclusion criteria were patients with cerebral hemorrhage, cerebral arteriovenous malformations and aneurysms, and those lost to follow-up or for whom follow-up was not available for at least 1 year after stenting. Functional capability was evaluated by using the mRS. Assessment of functional capability was conducted by two physicians independently, and any discrepancies were resolved by a third physician. Functional capability was assessed at two time points; the first assessment was conducted before stenting and the second in an outpatient clinic, 1 year after stenting treatment.
Patients were divided into two groups based on patient functional capability, with mRS ≤2 points (ie, 0, 1, or 2) considered physically “good condition” and mRS >2 points (ie, 3, 4, 5, or 6) defined as “poor condition”. Medical records were reviewed and data recorded for a total of 107 patients.
Patients were transferred from outpatient clinics, emergency departments, or branch hospitals to Chunghua Christian Hospital where they were admitted for examination and treatment. All patients had comprehensive medical history recorded at admission along with carotid ultrasound and biochemistry investigations. Cranial diffusion-weighted sequence magnetic resonance imaging and angiography was conducted to confirm the ischemic lesion. The selected patients were stented, on average, 1 month after the index stroke episode. All patients underwent several neuroimaging examinations to confirm the degree of stenosis before the stenting treatment, and all stenting was conducted by one specialist. The study was approved by the Institutional Review Board of Chunghua Christian Hospital. The study was retrospective and the informed consent was not required by the Institutional Review Board of Chunghua Christian Hospital.
Baseline patient history
Patient demographics (eg, sex and age) and pertinent risk factors were obtained. Age, sex, body mass index, low-density lipoprotein (LDL), glycated hemoglobin, chronic kidney disease (CKD), chronic heart failure, atrial fibrillation, gouty arthritis, diabetes mellitus, hypertension, and dyslipidemia (defined as previous bloodstream LDL recording(s) ≥100 mg/dL and/or under lipid-lowering agent treatment) were extracted from the chart records to a standardized data extraction form.
Imaging
Carotid ultrasound and neuroradiological examinations were conducted according to standard protocols. Further information is included in the supplementary materials.
Statistical analyses
Statistical analyses were performed using the statistical package SPSS for Windows (Version 16.0, SPSS Inc, Chicago, IL, USA).
Data analysis was conducted in three steps
Step 1
Clinical baseline characteristics and carotid ultrasound data were classified into two groups according to the mRS score (mRS ≤2 and mRS >2). The Mann–Whitney U-test was used to determine differences in the means of continuous variables between the two groups. Categorical variables were compared using the χ2 test or Fisher’s exact test where appropriate. Multivariate logistic regression was employed to assess the significance of risk factors; P-values <0.050 were considered statistically significant.
Step 2
The data were processed in the Chi-squared Automatic Interaction Detection system (CHAID), and the most influential variables were selected and classified.Citation16–Citation19 CHAID, a decision tree widely used in fields such as business, marketing, and medical research, can be used for prediction and classification, and for detecting the interaction between variables. CHAID can reveal the most critical risk factors in both groups, thereby assisting clinicians to decide whether patients are suitable for stenting (ie, according to the predicted level of improvement after stenting). CHAID uses a prepruning strategy; a node is split only if a significant criterion is satisfied, thus preventing overfitting. CHAID was selected as our decision tree because of the criticality of interpretation and tree construction without overfitting.
Admission LDL was the root node of the tree, and LDL <100 mg/dL and ≥100 mg/dL were dichotomized as 0 and 1, respectively.Citation16,Citation17 The other internal nodes, such as resistance index (RI), were dichotomized using 0.75 as the cut-off, with 0 and 1 representing values below and above 0.75, respectively. Sex was denoted with the letters F and M representing female and male, respectively. The disease-related parameters (ie, CKD, dyslipidemia, and gouty arthritis) were dichotomized as 0 (without disease) and 1 (with disease).
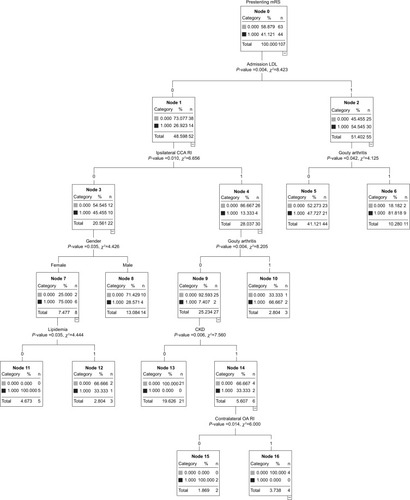
Although the objective was to obtain the risk factors and their interactions, the classification accuracy was also validated. We employed a leave-one-out cross-validation strategy to evaluate the misclassification rate of the decision tree and obtained an error rate of 23.3%. Most errors occurred in the right branch (; admission LDL = yes, gouty arthritis = no) because of missing clinical records or unclear documentation. Excluding these data, the error rate was 6.3%, thus validating the CHAID predictions.
Figure 1 Display of the CHAID.
Abbreviations: mRS, modified Rankin Scale; LDL, low-density lipoprotein; CCA, common carotid artery; RI, resistance index; CKD, chronic kidney disease; OA, ophthalmic artery; CHAID, Chi-squared Automatic Interaction Detection system.
Step 3
After obtaining the calculated contributing risk factors for stroke, we used the finite-state machine (FSM) to interpret the poststenting improvement.Citation18 FSM is a computational system model consisting of a set of states, inputs, and rules that map each state to another state or to itself. FSM is an effective graphical decision-making model and is widely applied in such fields as communication protocol design, biology, and artificial intelligence. The prestenting data were projected to the followed-up mRS states (dichotomized as subsequent worse or improved condition) by using FSM to correlate the two groups.
Results
Baseline characteristics for the two groups of patients, mRS ≤2 and mRS >2, are as listed in . Age at admission, LDL, and gouty arthritis differed significantly between the groups (P<0.05). The prestenting carotid duplex data were comparable between the two groups, except for ipsilateral common carotid artery (CCA) RI (P=0.01; ).
Table 1 Baseline clinical characteristics
Table 2 Prestenting carotid ultrasound data
The baseline data were correlated with follow-up mRS score using an FSM model. In those patients with favorable baseline characteristics (mRS ≤2), 46% exhibited improvements in the follow-up mRS, whereas 54% exhibited stable values. In the mRS >2 group, most patients exhibited stable values (75%), 23% exhibited an improvement, and 2% presented higher values in their follow-up mRS grading.
The risk factors of interest were further grouped and analyzed using multivariate logistic analysis (). Admission LDL (odds ratio [OR]: 5.00, 95% confidence interval [CI]: 1.86, 13.44), gouty arthritis (OR: 3.25, 95% CI: 1.03, 10.22), and ipsilateral CCA RI (OR: 0.30, 95% CI: 0.11, 0.83) were all significantly associated with mRS score at baseline.
Table 3 Multivariate logistic regression analyses
The results of the CHAID decision tree analysis are shown in . In the right branch of CHAID, internal node 2 is gouty arthritisCitation20–Citation22 (P=0.042); a baseline diagnosis of gouty arthritis is, therefore, likely to influence the diagnosis and outcome of stenting in stroke patients. However, medical records of patients with LDL exceeding 100 and without gouty arthritis may be missing or not well documented. In the mRS >2 group, node 6 (admission LDL =1 and gouty arthritis =1) has a large proportion, which classifies the two groups (baseline mRS ≤2 and mRS >2) well. In the left branch, internal node 1 is ipsilateral CCA RI (χ2=6.66; P=0.010). SexCitation23 and gouty arthritis are internal node 3 (χ2=4.43; P=0.035) and node 4 (χ2=8.21; P=0.004), respectively; gouty arthritis is considered as a chance node again. The branch starts at node 4 and terminates at the end nodes (nodes 10, 13, 15, and 16), confirming effective classification; in particular, node 13 has 21 patients with stroke of low severity. CKDCitation24,Citation25 is node 9 (χ2=4.43; P=0.035) and contralateral ophthalmic artery RI is node 14 (χ2=6.00; P=0.014); both these factors influence the clinical diagnosis and outcome. In the final branch, sex was internal node 3 (χ2=4.43; P=0.035) and dyslipidemia was internal node 7 (χ2=4.44; P=0.035). The three end nodes (nodes 8, 11, and 12) exhibit satisfactory classification.
The parameters of the CHAID tree were weighted in descending order of influence as follows: admission LDL (OR: 0.323), gouty arthritis (OR: 0.262), CKD (OR: 0.143), ipsilateral CCA RI (OR: 0.108), contralateral ophthalmic artery RI (OR: 0.072), sex (OR: 0.051), and dyslipidemia (OR: 0.042).
Similarities were observed in the variables selected using CHAID and multivariate analysis ( and ). Most significant variables, especially the critical factors, were the same: admission LDL, ipsilateral CCA RI, and gouty arthritis.
Discussion
The mRS scale is primarily a reflection of a patient’s mobility and degree of daily life independence. In our study, we observed significant improvement in motor function, but not high cortical function, following stenting treatment. It was observed that approximately 46% of the patients with favorable baseline characteristics (mRS score ≤2) exhibited improved mRS following stenting, and no patients with deterioration in mRS were observed in this group. In the group with unfavorable baseline mRS scores (mRS score >2), approximately 75% of the patients had stable follow-up mRS scores, with approximately 23% exhibiting an improvement. The physical harm derived from carotid artery stenting in the unfavorable group was near zero. These findings demonstrate that carotid artery stenting can improve most ischemic stroke patients’ functional outcomes, regardless of baseline characteristics, or at least stabilize previous functionalities.
A recent systematic review of guidelines for treatment of carotid stenosis found 33 guidelines relating to symptomatic carotid stenosis, of which CAS was endorsed by 27 of these guidelines (82%) for use in those patients at high Carotid endarterectomy risk due to comorbidities, vascular anatomy, or other reasons.Citation12 Carotid stenting is recommendedCitation13 for carotid stenosis patients when the diameter of the lumen is reduced by >70% by noninvasive imaging or >50% by catheter-based imaging. In addition, for elderly patients with carotid stenosis, carotid endarterectomy is preferred over carotid stenting treatment as it is associated with better outcomes. In our study, patients selected for carotid artery stenting were in the >70% or >50% category in accordance with the guideline. Furthermore, the mean age of our study population was about 70 years, because carotid endarterectomy is not a procedure conducted at our institution. The midterm functionality of our study population, in contrast to the findings reported in the guideline, revealed either stationary or improved outcome.
Admission LDL is significantly associated with the outcome of carotid stenting, as measured by mRS, in first-time ischemic stroke patients, implying that it may be a useful factor in predicting outcomes. The level of LDL should be evaluated at patient admission. Interestingly, high LDL levels have been implicated as being associated with poor outcomes in the coronary stenting setting.Citation26,Citation27
The most influential risk factors yielded by CHAID were consistent with the significant variables in the multivariate logistic regression analysis. Admission LDL, gouty arthritis, and ipsilateral CCA RI were the first decision and chance nodes in CHAID and were also significant in the multivariate analysis, thus affirming the reliability of the decision tree. High lipid profile patients might be comparatively asymptomatic compared with other risk factors or unaware that they are at risk. This finding underlies the significant value of blood lipid profile work-up at admission.
The fact that gouty arthritis is associated with poor outcome may underlie the proinflammatory nature of the condition. Interestingly, high serum uric acid concentration is a known risk factor for gout, and one study has shown that in patients with acute ischemic stroke, the chance of a good clinical outcome increases significantly with increasing serum uric acid concentration.Citation28
RI, a clinical parameter generated from carotid ultrasound, represents the general downstream blood vascular bed resistance level.Citation29 Values of RI greater than 0.75 denote increased downstream vascular bed resistance level and can arise as a result of a number of factors, including obstructions. Because CCA and internal carotid artery are the major vessels supplying blood to the intracranial hemispheres, their RI values are lower than that of external carotid artery under normal circumstances (CCA and internal carotid artery <0.75, external carotid artery >0.75).
In this study, it was observed that ipsilateral CCA RI was a critical factor among patients included in the analysis. The analysis of the baseline mRS ≤2 and >2 groups revealed that patients with RI >0.75 were more commonly found in the mRS ≤2 group. This interesting observation may be explained by the flow velocity pattern formula ([peak systolic velocity {PSV} – end diastolic velocity {EDV}]/PSV; normal value: ≤0.75).Citation30 When the stenosis increases, PSV increases correspondingly. As the stenosis nears the threshold, the PSV stops increasing; subsequently, the EDV increases. The low RI indicates that EDV has reached a critical threshold. This indication can lead to a poor clinical outcome.
This study has several limitations. First, because this was a retrospective, single medical center study, the sample size was small and the case selection was prone to biases and confounding factors; the results must be carefully interpreted. Second, all patients were of Asian origin, and therefore the results may be applicable only to Asian populations. Third, most patients in this study were elderly, and so caution should be used before extrapolation to other age groups. Fourth, medical treatment during the poststenting phase could have been viewed on the medical chart by the clinician (eg, antigouty arthritis and antihyperlipidemic drugs). This might have led to bias at the time of assessment of follow-up mRS score, resulting in interpretation bias. Finally, the follow-up duration was short (at around 1 year). Studies of a longer duration are warranted.
Conclusion
Among commonly measured baseline characteristics, admission LDL is associated with midterm functional outcomes. This study supports the effectiveness of carotid stenting, even in those patients with poor baseline physical function.
Acknowledgments
Our special thanks to Ping-Yi Lin, PhD, of Chunghua Christian Hospital for her literature review. This project is partially supported by Ministry of Science and Technology and Big Data Research Center of National Chiao Tung University, Taiwan.
Supplementary materials
Carotid ultrasound examination
Cervical carotid artery examination was performed using a Philips iE33 7 mHz linear transducer. Patients slightly tilted their head to the contralateral side, and the transducer was placed on their necks. Cross-sectional B mode scanning was performed to detect intraluminal plaque, and longitudinal screening was adopted for validation. The plaque was classified as subtype 1–4 independently by two physicians according to the international classification system.Citation1 In case of classification discrepancy, reassessment was conducted by a third physician. The common carotid intima–media thickness at the midportion on the ipsilateral side (symptomatic side of the index stroke event) was measured. Peak systolic velocity (PSV), end diastolic velocity (EDV), and resistance index (flow velocity pattern formula, defined as PSV − EDV)/PSV) of the common carotid artery (CCA), internal carotid artery, external carotid artery, and ophthalmic artery bilaterally were assessed. Reversal of blood flow in the ophthalmic artery was also measured. Forward and reverse flow was defined as blood flow away from the stenotic ipsilateral carotid artery and blood flow into the carotid artery, respectively. The degree of carotid stenosis was calculated according to the European Carotid Surgery Trial methodCitation2 along with parameter classification at various sites of the extracranial carotid system.Citation3
Neuroradiological examinations
Magnetic resonance imaging/angiography
Structural and functional magnetic resonance images and angiographic examinations were performed using a 3T-(Magnetom Verio, Siemens Healthcare, Malvern, PA, USA) or 1.5 T imager (Magnetom Aera, Siemens Healthcare) with a cervical coil. A standard protocol was followed to evaluate stroke, including axial diffusion-weighted imaging, apparent diffusion coefficient, and fluid-attenuated inversion-recovery sequences. Three-dimensional time-of-flight magnetic resonance angiography without contrast enhancement was performed in the transverse plane by using a sliding interleaved kY acquisition sequence comprising six overlapping slabs of eleven sections by employing the following parameters: section thickness, 1.2 mm; repetition time (ms)/echo time (ms), 242/7; flip angle, 20°; field of view, 200×200 mm2; matrix, 205×320. The final pixel size was 0.975×0.625 mm. The entire imaging time was approximately 7 minutes.
Digital subtraction angiography and stenting
Biplanar intra-arterial digital subtraction angiography was performed using a biplanar flap panel rotational angiography unit (Axiom Artis Zee, Siemens Healthcare) with an image intensifier matrix of 1,024×1,024 pixels and a final pixel size of 0.37 mm. Immediately after approaching the femoral artery, a 7-F catheter (Mach 1, Boston Scientific, Marlborough, MA, USA) was inserted into the right or left CCA near the carotid bifurcation. Posteroanterior and lateral projections were acquired at the level of carotid bifurcation. A third projection at an oblique angle was acquired if overlapping vessels were noted in the original two projections. For each projection, 11 mL of nonionic iodinated contrast material (Omnipaque 350, GE Healthcare, Carrigtwohill, Co. Cork, Ireland) was intra-arterially injected at a flow rate of 7 mL/s by using an automatic injector (Mark V ProVis, Medrad, Whippany, NJ, USA). Subsequently, stenting was performed. A guidewire was inserted into the carotid artery on either side of the stenotic region. An EZ filter wire (Boston Scientific, Marlborough, MA, USA) was used predilation to prevent most of the major strokes caused by distal embolic migration. Overall, 5,000 units of prophylactic heparin were administered. A self-expandable ×30 mm carotid wall stent was delivered coaxially through the guiding catheter into the stenotic area (Figure S1).
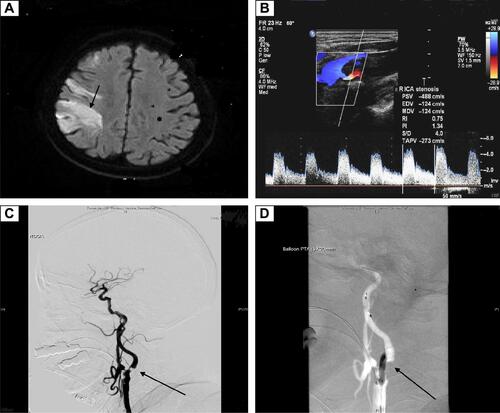
Figure S1 An example of first-time ischemic stroke with critical carotid artery stenosis.
Notes: The patient was brought to our stroke services due to acute onset of left-sided weakness and slurred speech 1 day prior to ward admission. (A) The diffusion-weighted sequence of MRI showed right middle cerebral artery territory high signal intensity, suggestive of ischemic lesion (black arrow). (B) Extracranial carotid duplex showed increased resistance flow profile with turbulent flow, high PSV, and spectral broadening of right proximal ICA. (C) Digital subtraction angiography revealed critical stenosis (>90%) of the right distal CCA and the proximal part of ICA (black arrow). (D) The stent was delivered subsequently through a guiding catheter into the right ICA (black arrow).
Abbreviations: ICA, internal carotid artery; PSV, peak systolic velocity; EDV, end diastolic velocity; MDV, mean diastolic velocity; RI, resistance index; PI, pulsatility index; S/D, ratio of systolic to diastolic blood pressure; TAPV, time-averaged peak velocity; MRI, magnetic resonance imaging; CCA, common carotid artery.
References
- Gray-WealeACGrahamJCBurnettJRByrneKLusbyRJCarotid artery atheroma: comparison of preoperative B-mode ultrasound appearance with carotid endarterectomy specimen pathologyJ Cardiovasc Surg19882966766813062007
- MRC European Carotid Surgery Trial: interim results for symptomatic patients with severe (70%–99%) or with mild (0%–29%) carotid stenosis. European Carotid Surgery Trialists’ Collaborative GroupLancet (London, England)1991337875212351243
- GrantEGBensonCBMonetaGLCarotid artery stenosis: grayscale and Doppler ultrasound diagnosis – society of radiologists in ultrasound consensus conferenceUltrasound Q200319419019814730262
Disclosure
The authors report no conflicts of interest in this work.
References
- AdamsHPJrBendixenBHKappelleLJClassification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke TreatmentStroke199324135417678184
- MeyerSAGandhiCDJohnsonDMWinnHRPatelABOutcomes of carotid artery stenting in high-risk patients with carotid artery stenosis: a single neurovascular center retrospective review of 101 consecutive patientsNeurosurgery2010663448453 discussion 53–5420124935
- SpenceJDManagement of asymptomatic carotid stenosisNeurol Clin201533244345725907915
- MaddenKPKaranjiaPNAdamsHPJrClarkeWRAccuracy of initial stroke subtype diagnosis in the TOAST study. Trial of ORG 10172 in Acute Stroke TreatmentNeurology19954511197519797501144
- ChaturvediSSaccoRLHow recent data have impacted the treatment of internal carotid artery stenosisJ Am Coll Cardiol201565111134114325790886
- EcksteinHHKuhnlADorflerAKoppIBLawallHRinglebPAThe diagnosis, treatment and follow-up of extracranial carotid stenosisDtsch Arztebl Int201311027–2846847623964303
- HuHShengWChuFLanCChiangBIncidence of stroke in TaiwanStroke199223912371519277
- TsaiCFThomasBSudlowCLEpidemiology of stroke and its subtypes in Chinese vs white populations: a systematic reviewNeurology201381326427223858408
- HankeyGJLong-term outcome after ischaemic stroke/transient ischaemic attackCerebrovasc Dis (Basel, Switzerland)200316Suppl 11419
- LiLYiinGSGeraghtyOCIncidence, outcome, risk factors, and long-term prognosis of cryptogenic transient ischaemic attack and ischaemic stroke: a population-based studyLancet Neurol201514990391326227434
- WuTHChenHHLeeTKFactors affecting the first recurrence of noncardioembolic ischemic strokeThromb Res20009739510310680640
- AbbottALParaskevasKIKakkosSKSystematic review of guidelines for the management of asymptomatic and symptomatic carotid stenosisStroke201546113288330126451020
- KernanWNOvbiageleBKittnerSJResponse to letter regarding article, “Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association”Stroke2015464e87e8925744519
- VogelTRDombrovskiyVYHaserPBScheirerJCGrahamAMOutcomes of carotid artery stenting and endarterectomy in the United StatesJ Vasc Surg2009492325330 discussion 3019058948
- ZhangLZhaoZOuyangYSystematic review and meta-analysis of carotid artery stenting versus endarterectomy for carotid stenosis: a chronological and worldwide studyMedicine20159426e106026131824
- Ben-HaimYTom-TovEA streaming parallel decision tree algorithmJ Mach Learn Res201011849872
- LohWYClassification and regression treesData Min Knowl Disc201111423
- QuinlanJInduction of decision treesMach Learn1986181106
- UtgoffPIncremental induction of decision treesMach Learn19894161186
- ChamorroAAmaroSCastellanosMSafety and efficacy of uric acid in patients with acute stroke (URICO-ICTUS): a randomised, double-blind phase 2b/3 trialLancet Neurol201413545346024703208
- LiuKLLeeHFChouSHAcute gouty arthritis complicated with acute ST elevation myocardial infarction is independently associated with short- and long-term adverse non-fatal cardiac eventsClin Rheumatol2014331919823990026
- VinikOWechalekarMDFalzonLBuchbinderRvan der HeijdeDMBombardierCTreatment of asymptomatic hyperuricemia for the prevention of gouty arthritis, renal disease, and cardiovascular events: a systematic literature reviewJ Rheumatol Suppl201492707425180131
- IkawaFKatoYKobayashiSGender difference in cerebrovascular diseaseNihon Rinsho201573461762425936150
- MassonPWebsterACHongMTurnerRLindleyRICraigJCChronic kidney disease and the risk of stroke: a systematic review and meta-analysisNephrol Dial Transplant20153071162116925681099
- ToyodaKCerebral small vessel disease and chronic kidney diseaseJ Stroke2015171313725692105
- CaiALiLZhangYBaseline LDL-C and Lp(a) elevations portend a high risk of coronary revascularization in patients after stent placementDis Markers201335685786224367139
- LerakisSEl-ChamiMFPatelADEffect of lipid levels and lipid-lowering therapy on restenosis after coronary artery stentingAm J Med Sci2006331527027316702797
- ChamorroAObachVCerveraARevillaMDeulofeuRAponteJHprognostic significance of uric acid serum concentration in patients with acute ischemic strokeStroke20023341048105211935059
- PourcelotLApplications cliniques de l’Examen Doppler TranscutanePeronneauPSymposium: Velocimetric Ultrasonnor Doppler34Paris, FranceINSERM1974213240
- TouboulPHennericiMMeairsSMannheim carotid intima-media thickness consensus (2004–2006). An update on behalf of the Advisory Board of the 3rd and 4th Watching the Risk Symposium, 13th and 15th European Stroke Conferences, Mannheim, Germany, 2004, and Brussels, Belgium, 2006Cerebrovasc Dis (Basel, Switzerland)2007237580
