Abstract
Purpose
Numerous studies have tried to combine transarterial chemoembolization (TACE) or hepatic arterial infusion chemotherapy (HAIC) with radiotherapy (RT) for the treatment of hepatocellular carcinoma (HCC) patients with portal vein tumor thrombus (PVTT). However, the efficacy of TACE or HAIC combined with RT versus TACE or HAIC alone remains controversial. Thus, we performed a meta-analysis to compare the efficacy and safety of intra-arterial chemoembolization combined with RT versus intra-arterial chemoembolization alone for the treatment of HCC patients with PVTT.
Methods
PubMed, Embase, and Cochrane Library databases were systematically searched for eligible studies. Two authors independently reviewed the abstracts, extracted relevant data and rated the quality of studies. The major end points were objective response rate (ORR), overall survival (OS), and adverse events.
Results
Eight studies with a total of 1,760 patients were included in this meta-analysis. The pooled results showed that intra-arterial chemoembolization combined with RT significantly improved ORR of PVTT (OR, 4.22; 95% CI, 3.07–5.80; P<0.001) and OS (HR, 0.69; 95% CI, 0.57–0.83; P=0.001), but did not affect ORR of primary liver tumor (OR, 1.37; 95% CI, 0.67–2.79; P=0.390). The incidence of grade 3 or 4 leukopenia (OR, 5.80; 95% CI, 2.478–13.56; P<0.001) and thrombocytopenia (OR, 3.77; 95% CI, 1.06–13.43; P=0.041) was higher in the intra-arterial chemoembolization plus RT group than in the intra-arterial chemoembolization group.
Conclusion
Combination therapy of intra-arterial chemoembolization and RT for HCC patients with PVTT could bring higher ORR of PVTT and better survival benefits. This combination therapy was also associated with a significantly increased risk of adverse events. However, they were mostly mild to moderate and successfully treated with conservative treatment.
Introduction
Portal vein tumor thrombus (PVTT) is an important biological behavior of advanced hepatocellular carcinoma (HCC). HCC patients complicated by the presence of PVTT are classified as Barcelona Clinic Liver Cancer (BCLC) stage C. Tumor invasion of the portal vein not only promotes wide dissemination of tumor throughout the liver but also increases the risk of liver failure.Citation1,Citation2 The prognosis of these patients is extremely poor with survival limited to only several months without any treatment.Citation3
Many modalities such as resection, transarterial chemoembolization (TACE), hepatic arterial infusion chemotherapy (HAIC), external radiotherapy (RT), immunotherapy, and sorafenib have been tried for the treatment of HCC with PVTT, but the optimal treatment strategy remains complicated and controversial. TACE was not recommended because it had a potential risk of liver failure.Citation4 Recently, however, some studies have shown its survival benefits for advanced HCC with PVTT, even with the main portal vein.Citation5 RT also has been reported to have some good responses and promising outcomes for the treatment of target PVTT in HCC patients.Citation6 There are numerous studies that report that the combination of TACE or HAIC and RT could be a reasonable treatment option for HCC patients with PVTT. Some studies showed that adding RT to TACE or HAIC does not improve survival and has an increased incidence of adverse events compared with TACE or HAIC alone,Citation7,Citation8 while some showed that survival was significantly higher in the TACE or HAIC plus RT group.Citation9,Citation10
Hence, we conducted this meta-analysis to evaluate the therapeutic effectiveness of TACE or HAIC plus RT to TACE or HAIC alone in terms of objective response rate (ORR), survival and adverse events in HCC patients with PVTT.
Methods
Literature search
This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement (http://prisma-statement.org).Citation11,Citation12 A comprehensive literature search through sources PubMed, Embase and Cochrane Library databases was performed. Search main terms were as follows: (“hepatocellular carcinoma” or “liver cancer” or “liver carcinoma” or “liver neoplasm” or “hepatic cancer” or “hepatic carcinoma” or “hepatic neoplasm” or “hepatoma” or “hepatocarcinoma”) and (“portal vein tumor thrombus” or “portal vein thrombus”) and (“hepatic arterial infusion chemotherapy” or “hepatic arterial infusion chemotherapy” or “HAIC” or “TACE” or “transarterial chemoembolization”) and (“radiotherapy”). A manual search of reference lists of relevant papers was also performed to identify other potentially relevant articles. There were no restrictions on study date and the language was restricted to English.
Inclusion and exclusion criteria
This meta-analysis was focused on comparing the efficacy and safety of intra-arterial chemoembolization combined with RT versus intra-arterial chemoembolization alone in the treatment of HCC patients with PVTT. Therefore, only comparative analysis concerning clinical value of TACE or HAIC in combination with RT versus TACE or HAIC alone for HCC patients with PVTT was used. The inclusion criteria should be as follows: 1) the study subjects were HCC patients with PVTT without metastases; 2) sufficiently detailed data on methods, characteristics of patient population and survival; 3) the administration schedules of TACE or HAIC modalities should be similar in both groups. The exclusion criteria should be as follows: 1) abstracts, letters, case reports, reviews, meta-analyses, conference abstracts and proceedings and 2) impossible to extract the essential data needed for this meta-analysis from the published results. Only the most recent or highest quality report was included when the study results were based on overlapping cohorts from the same institution. Tumor response rates were evaluated based on the comparison of abdominal CT or magnetic resonance imaging (MRI) before and after treatment according to the modified Response Evaluation Criteria in Solid Tumours (RECIST) guidelines for HCC.Citation13 Complete response (CR): complete clearance of the lesion after treatment; partial response (PR): size of lesion decreased >30% after treatment; progressive disease (PD): size of lesion increased >20% after treatment; NR, no response; stable disease (SD), all other variations. shows the search strategy in detail.
Data extraction and quality assessment
Two authors (QZ and KZ) independently searched and screened all potentially eligible studies based on the inclusion and exclusion criteria detailed above. The following information was extracted: first author name, year of publication, sample size, use of TACE or HAIC, RT dose, follow-up time, and outcomes such as survival, tumor response, and adverse events. The survival data was collected after the propensity score matching analysis. The primary outcome was ORR, which was calculated for each study using the following formula: ORR = (CR + PR/total number of patients) ×100%. Secondary outcomes were OS and adverse events. OS was defined as the time from the commencement of treatment until death or last follow-up time. Any disagreement in the data extraction was resolved by consensus and discussion.
The methodological quality of the included literatures was evaluated and graded according to Newcastle Ottawa Scale (NOS). The NOS contains three parameters of quality: selection (0–4 points), comparability (0–2 points), and outcome assessment (0–3 points). The quality score ranged from 0 to 9 points, and article quality was classified into low (from 0 to 3 points), moderate (from 4 to 6 points), and high (>7 points) groups.
Statistical analysis
All statistical analyses were performed using STATA statistical software (Version 14; STATA Corp, College Station, TX, USA). Pooled odds ratios (ORs) with the corresponding 95% confidence intervals (CIs) were calculated to evaluate the efficacy of intra-arterial chemoembolization plus RT versus intra-arterial chemoembolization alone on tumor response as well as on the incidence of adverse events. Hazard ratios (HRs) with the corresponding 95% CIs were used to evaluate the survival advantage of the intra-arterial chemoembolization plus RT compared with RT alone. We estimated the HRs using the Kaplan–Meier methodology with log-rank test. If the HRs were not obtained directly by the original literature, we extracted these values from the available statistical information with the methods provided by Tierney et al.Citation14 ORs or HRs were assessed using the Mantel–Haenszel test. I2 statistics were used to measure statistical heterogeneity (I2>50% was considered indicative of significant heterogeneity). If significant heterogeneity existed, a fixed-effect statistical model was used; otherwise, a random-effect model was used.Citation15 We used Harbord’s test to evaluate a publication bias. All tests were two-sided (P=0.05 was considered statistically significant).
Results
Description of the studies
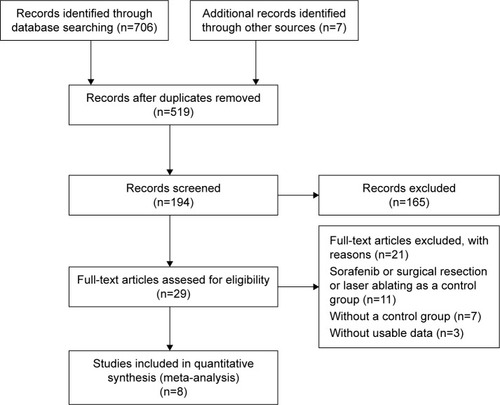
A total of 706 potentially relevant articles were identified through the systematic search. All titles or abstracts were screened, and 29 articles were retrieved for detailed evaluation. After reviewing and evaluating these studies, 21 articles were excluded because of the following reasons: 11 articles were related to other treatments such as sorafenib, surgical resection or laser abating; 7 articles did not employ a control group; and 3 articles lacked the outcome of interest. Finally, eight studiesCitation7–Citation10,Citation16–Citation19 qualified the inclusion criteria and were analyzed in our meta-analysis (). Baseline characteristics of the studies included in the meta-analysis, as well as the NOS scores, are summarized in . The included studies were all conducted in Asian populations: four were conducted in Japan, two in the People’s Republic of China, and two in Korea. In these eight comparative studies, which contained three prospective studies and five retrospective studies, two studies were analyzed using propensity score-matched method. A total of 1,760 patients were included in the meta-analysis, among which 490 patients were in intra-arterial chemoembolization plus RT group and 1,270 patients were in intra-arterial chemoembolization alone group.
Table 1 Characteristics of the trials included in the meta-analysis
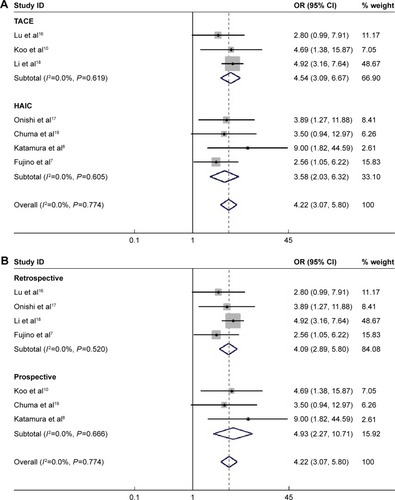
Objective response of PVTT and primary tumor to treatment
The ORR of PVTT to treatment was reported in seven studies which included 1,203 patients. In these studies, ORR of PVTT ranged from 42.86% to 75% in the intra-arterial chemoembolization plus RT group and from 13.79% to 45.45% in the intra-arterial chemoembolization-alone group. About 182 (61.90%) of 294 patients received CR or PR in the intra-arterial chemoembolization combined with RT group, whereas 304 (33.44%) of 909 patients achieved CR or PR in intra-arterial chemoembolization-alone group. The value of I2 was <50% (P=0.774), applying the fixed-effect model in this pooled analysis. As shown in , the pooled results demonstrated that intra-arterial chemoembolization plus RT significantly improved ORR of PVTT compared with intra-arterial chemoembolization alone (OR =4.22; 95% CI, 3.07–5.80; P<0.001). The pooled OR was found to be 4.54 in TACE plus RT group (95% CI, 3.09–6.67; P<0.001; ) and 3.58 in HAIC plus group (95% CI, 2.03–6.32; P<0.001; ). By performing subgroup analyses with regard to study design, we noticed that there was significantly improved ORR of PVTT in intra-arterial chemoembolization plus RT group in both retrospective studies (HR, 4.09; 95% CI, 2.89–5.80; P<0.001; ) and prospective studies (HR, 4.93; 95% CI, 2.77–10.71; P<0.001; ).
Figure 2 Odds ratios and 95% confidence intervals for objective response rate of portal vein tumor thrombus.
Abbreviations: CI, confidence interval; HAIC, hepatic arterial infusion chemotherapy; OR, odds ratio; TACE, transarterial chemoembolization.
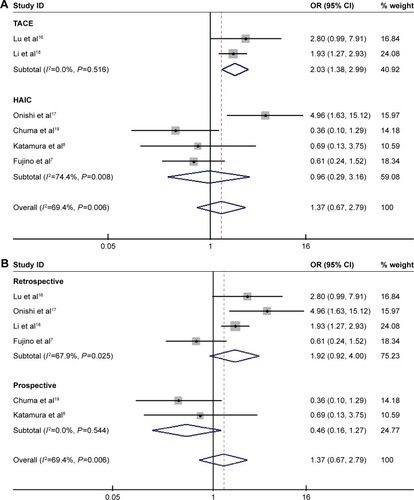
Six studies which included 1,132 patients presented data of ORR of primary liver tumor. ORR of primary liver tumor in these studies ranged from 18.75% to 70% in the intra-arterial chemoembolization plus RT group and from 17.65% to 50.2% in the intra-arterial chemoembolization-alone group. About 134 (53.17%) of 252 patients received CR or PR in intra-arterial chemoembolization combined with RT group, whereas 423 of 880 (48.07%) patients achieved CR or PR in intra-arterial chemoembolization-alone group. The random-effect model was used due to heterogeneity (I2=69.4%; P=0.006). As illustrated in , there were no significant differences with regard to ORR of primary liver tumor between the two modalities (OR, 1.37; 95% CI, 0.67–2.79; P=0.390). The pooled OR was found to be 2.03 in TACE plus RT group (95% CI, 1.38–2.99; P<0.001; ) and 0.96 in HAIC plus RT group (95% CI, 0.29–3.16; P=0.940; ). In other words, the TACE plus RT would significantly improve the ORR of primary liver tumor to treatment while the HAIC plus RT did not. By performing subgroup analyses with regard to study design, we noticed that there were no significant differences in either retrospective studies (HR, 1.92; 95% CI, 0.92–4.00; P=0.081; ) or prospective studies (HR, 0.46; 95% CI, 0.16–1.27; P=0.132; ).
Figure 3 Odds ratios and 95% confidence intervals for objective response rate of primary liver tumor.
Abbreviations: CI, confidence interval; HAIC, hepatic arterial infusion chemotherapy; OR, odds ratio; TACE, transarterial chemoembolization.
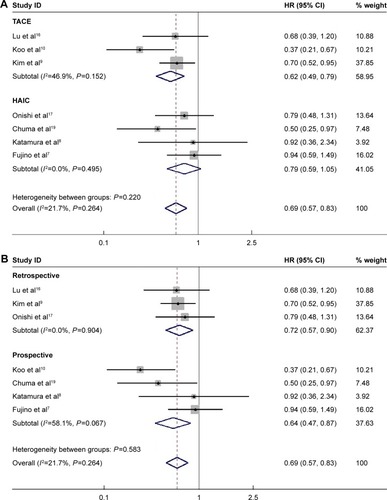
Overall survival
Median survival time (MST) was reported in all included studies, ranging from 7.5 to 13.02 months in TACE plus RT group and from 4.1 to 9.1 months in TACE-alone group. Among these studies, three studies showed that the MST was similar between the two groups, four studies demonstrated that the MST was significantly higher in the TACE combined with RT group, and the remaining one did not report the difference between two groups.
Seven studies were identified with the available data of HR for OS after treatment. Among these studies, four studies showed that the OS was similar between the two groups, whereas the remaining three studies showed that the OS was significantly better in the TACE plus RT group than the TACE-alone group. The number of patients from these studies ranged from 32 to 83 and a total of 847 patients were included. No significant statistical heterogeneity was detected among these studies (I2=21.7%; P=0.264), and the fixed-effect model was used. Meta-analysis showed that the combination of intra-arterial chemoembolization and RT was associated with improved overall survival compared with intra-arterial chemoembolization-alone (HR, 0.69; 95% CI, 0.57–0.83; P=0.001; ). The pooled HR was found to be 0.62 in TACE plus RT group (95% CI, 0.49–0.79; P<0.001; ) and 0.79 in HAIC plus RT group (95% CI, 0.59–1.05; P=0.109; ). In other words, the TACE plus RT would significantly improve the patients overall survival while the HAIC plus RT did not. By performing subgroup analyses with regard to study design, we noticed that there was significantly improved overall survival in intra-arterial chemoembolization plus RT group in both retrospective studies (HR, 0.72; 95% CI, 0.57–0.90; P=0.005; ) and prospective studies (HR, 0.64; 95% CI, 0.47–0.87; P=0.004; ).
Figure 4 Comparison of the combination of intra-arterial chemoembolization and radiotherapy and intra-arterial chemoembolization alone for hepatocellular carcinoma patients with portal vein tumor thrombus in terms of overall survival.
Abbreviations: CI, confidence interval; HAIC, hepatic arterial infusion chemotherapy; HR, hazard ratio; TACE, transarterial chemoembolization.
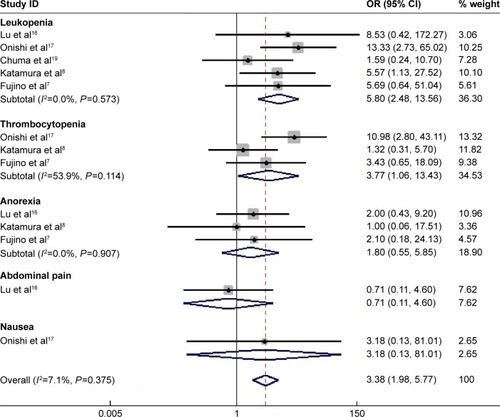
Adverse events
All included studies reported the occurrence of adverse events after treatment, including thrombocytopenia, leukopenia, blood bile increased, hepatic enzyme increase, anorexia, nausea, and abdominal discomfort. However, only five studies provided available data of grade 3 or 4 toxicities for analysis. There was no difference between two groups in terms of the incidence of anorexia (OR, 1.80; 95% CI, 0.55–5.85; P=0.329), abdominal pain (OR, 0.71; 95% CI, 0.11–4.60; P=0.723), and nausea (OR, 3.18; 95% CI, 0.13–81.01; P=0.483). However, a meta-analysis showed that TACE plus RT significantly increased the incidence of the leukopenia (OR, 5.80; 95% CI, 2.478–13.56; P<0.001) and thrombocytopenia (OR, 3.77; 95% CI, 1.06–13.43; P=0.041). As for the total rate of these adverse events, the pooled OR (95% CI, 1.98–5.77; P<0.001; ) was found to be 3.38, indicating that patients treated with TACE plus RT had significantly more grade 3 or 4 adverse events.
Publication bias
As the most included studies reported the ORR to treatment, we chose this data parameter to perform the analysis of publication bias. No significant publication bias was identified in this meta-analysis (Harbord’s test; P=0.311 for ORR of PVTT; P=0.463 for ORR of primary liver tumor).
Discussion
The progression of PVTT is an independent prognostic factor for HCC patients, so the treatment of PVTT plays an important role in improving the patients, survival.Citation10 In the present systematic review and meta-analysis, we collected the comparative data and assessed the tumor control, survival benefit, and safety in HCC patients with PVTT undergoing intra-arterial chemoembolization plus RT and intra-arterial chemoembolization alone. The pooled results demonstrated that in patients with HCC and PVTT, those who were treated with intra-arterial chemoembolization plus RT could achieve significantly higher PVTT response (OR =4.205; 95% CI, 3.055–5.790; P<0.001) and better overall survival (HR, 0.681; 95% CI, 0.546–0.848; P=0.001) than those with intra-arterial chemoembolization alone. The response rates of intrahepatic tumor in the intra-arterial chemoembolization plus RT group and intra-arterial chemoembolization alone group were similar (OR, 1.366; 95% CI, 0.670–2.786; P=0.390). There was likewise a statistically significant increase in toxicity (OR, 3.892; 95% CI, 2.274–6.659; P<0.001). However, they were mostly mild to moderate and successfully treated with conservative treatment. The combination therapy of intra-arterial chemoembolization and RT was well tolerated without no major complications with concurrent associated with the combination treatment. Based on these results, it was suggested that intra-arterial chemoembolization in combination with RT is a feasible and better choice for HCC patients with PVTT with tolerable toxicity.
Various treatment modalities have been proposed to treat HCC patients with PVTT. Surgical resection has been considered a preferred modality but it can only be performed for highly selected patients with hepatic functional reserved and the PVTT of whom is localized in the distal branch. Leng et alCitation20 demonstrated that HCC patients with PVTT treated with TACE had a significantly better 1-year survival rate compared with patients with liver resection. Wu et alCitation21 reported that the therapeutic efficacy of TACE plus RT was comparable to that of surgical intervention for PVTT in HCC patients. According to the BCLC guidelines for HCC treatment, sorafenib is recommended as the standard therapy for HCC patients with PVTT.Citation22 Pinter et alCitation23 reported that patients treated with TACE had a higher MST compared with patients with sorafenib (9.2 vs 7.4 months, P=0.377). Kim et alCitation9 also demonstrated that a combination of TACE and RT to treat target PVTT was to be superior, or at least comparable, to sorafenib with regard to overall survival and time to progression.Citation9 Selective internal radiation therapy (SIRT) and radioembolization with yttrium-90 (Y-90) microspheres also had been recommended to advanced HCC patients who are not eligible for transarterial chemoembolization due to PVTT.Citation24,Citation25 Therefore, prospective randomized and controlled studies with comparison data between these treatments are required to fully assess which kind of medication is better for improving the patients, survival.
Intra-arterial chemoembolization alone has limited efficacy for HCC patients with PVTT. RT was demonstrated to be an effective way to kill malignancy tumor cells and quickly relieve the portal venous occlusion.Citation26 The reduction in intravascular tumor size by appropriate RT may induce the restoration of portal blood flow, which would contribute to alleviation of hepatic ischemia and preservation of liver function and improve the chance of further intra-arterial chemoembolization with maximum treatment effect. When to use intra-arterial chemoembolization alone and in combination with radiation therapy in HCC patients with PVTT is a concern. Li et al reported that the outcome of combination therapy is not satisfactory for patients with PVTT-I and PVTT-IV while it could give a better survival outcome to patients with PVTT-II and PVTT-III.Citation18 Restricted by the incomplete data of the included literatures, we did not do a separate analysis regarding the classification of PVTT. Radiation was applied solely to treat PVTT in six of eight studies in this analysis because intrahepatic tumor tends to be large and multiple, whereas repeat intra-arterial chemoembolization was used to treat intrahepatic tumor. However, the tumor outside the fields of radiation quickly experiences a growth during RT. Therefore, a more short-term fractionation regimen may be able to resolve this problem. Many investigators have demonstrated that the combination of TACE and stereotactic body radiation therapy is an effective and feasible treatment modality for HCC patients with PVTT with good responses and minimal side effects.Citation1,Citation27,Citation28 Thus, comparative trials on the various dose fractionation schedules for the treatment of PVTT need to be carried out to analyze the clinical effect analysis. In addition, though there were several dose–response studies exploring the correlation between the RT dose and PVTT response, the optimal RT dose has not yet been established.Citation29,Citation30
The results of this meta-analysis are consistent with a prior meta-analysis that demonstrated therapeutic benefit from the combination of TACE and RT compared with TACE alone for unresectable HCC.Citation31 The meta-analysis involved 21 controlled trials that involving 2,577 HCC patients. They found that TACE plus RT significantly improved 1-year overall survival and CR (HR, 1.36 and 2.73, respectively; P<0.001 and P<0.001, respectively) compared with TACE alone. The MST for TACE plus RT (1,032 patients) was significantly higher than for TACE alone (1,354 patients; 22.7 vs 13.5 months; P<0.001). However, Huo et al included studies that compared TACE plus RT and TACE alone in patients with HCC whether the PVTT was present or not.Citation31 Our meta-analysis was performed to assess the combination of intra-arterial chemoembolization and RT compared with TACE alone on therapeutic effect for HCC patients with PVTT.
The limitations of our meta-analysis should be taken into account when interpreting the results. First, although we have taken into consideration the heterogeneity of available data from these studies, some other factors in study baseline characteristics such as the dose and type of intra-arterial chemoembolization protocols, the location of venous thrombus, type of tumor (diffuse or nodular) and the primary tumor size were not consistent across the trials and confounded the conclusions. Performing a more detailed subgroup analysis of survival is difficult with the limited individual patient’s data. Second, treatment schedule may have been selected based on patients, physical condition and it was biased. Patients with better liver function tended to be selected into the intra-arterial chemoembolization plus RT group, whereas those with poorer liver function may have been willing to receive intra-arterial chemoembolization alone. Third, the limited number of studies, a relatively small sample size, and the retrospective nature of the studies may increase the heterogeneity and affect the results of our analysis. Finally, all of the studies included in this meta-analysis come from Asia, which is the highest risk area for HCC.
In conclusion, our meta-analysis provided evidence that intra-arterial chemoembolization plus RT improved survival compared with intra-arterial chemoembolization alone for HCC with PVTT. This combination modality might be a promising therapeutic option for management of advanced HCC with PVTT in selective patients with acceptable toxicities. Given the overall sample size and the heterogeneity of our meta-analysis, further well-designed prospective controlled trials are warranted to evaluate the feasibility and efficacy of this combination therapy.
Disclosure
The authors report no conflicts of interest in this work.
References
- NakazawaTAdachiSKitanoMPotential prognostic benefits of radiotherapy as an initial treatment for patients with unresectable advanced hepatocellular carcinoma with invasion to intrahepatic large vesselsOncology2007731–2909718337620
- ZhangXBWangJHYanZPQianSDuSSZengZCHepatocellular carcinoma with main portal vein tumor thrombus: treatment with 3-dimensional conformal radiotherapy after portal vein stenting and transarterial chemoembolizationCancer200911561245125219156918
- WooHYHeoJNew perspectives on the management of hepatocellular carcinoma with portal vein thrombosisClin Mol Hepatol201521211512126157747
- ChoiJHRhoHKohYTSuhKSLeeKURisk factors of early recurrence after curative hepatic resection for hepatocellular carcinoma1999311165172
- XueTCXieXYZhangLYinXZhangBHRenZGTransarterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombus: a meta-analysisBMC Gastroenterol20131311923280118
- ChengSHLinYMChuangVPA pilot study of three-dimensional conformal radiotherapy in unresectable hepatocellular carcinomaJ Gastroenterol Hepatol199914101025103310530500
- FujinoHKimuraTAikataHRole of 3-D conformal radiotherapy for major portal vein tumor thrombosis combined with hepatic arterial infusion chemotherapy for advanced hepatocellular carcinomaHepatol Res201445660761725052365
- KatamuraYAikataHTakakiSIntra-arterial 5-fluorouracil/interferon combination therapy for advanced hepatocellular carcinoma with or without three-dimensional conformal radiotherapy for portal vein tumor thrombosisJ Gastroenterol200944549250219330281
- KimGAShimJHYoonSMComparison of chemoembolization with and without radiation therapy and sorafenib for advanced hepatocellular carcinoma with portal vein tumor thrombosis: a propensity score analysisJ Vasc Interv Radiol2015263320329.e625612807
- KooJEKimJHLimYSCombination of transarterial chemoembolization and three-dimensional conformal radiotherapy for hepatocellular carcinoma with inferior vena cava tumor thrombusInt J Radiat Oncol Biol Phys200978118018719926229
- LiberatiAAltmanDGTetzlaffJThe PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaborationBMJ2009339b270019622552
- MoherDLiberatiATetzlaffJAltmanDGPRISMA GroupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementInt J Surg20108533634120171303
- LencioniRLlovetJMModified RECIST (mRECIST) assessment for hepatocellular carcinomaSemin Liver Dis2010301526020175033
- TierneyJFStewartLAGhersiDBurdettSSydesMRPractical methods for incorporating summary time-to-event data into meta-analysisTrials2007811617555582
- DerSimonianRKackerRRandom-effects model for meta-analysis of clinical trials: an updateContemp Clin Trials200728210511416807131
- LuDHFeiZLZhouJPHuZTHaoWSA comparison between three-dimensional conformal radiotherapy combined with interventional treatment and interventional treatment alone for hepatocellular carcinoma with portal vein tumour thrombosisJ Med Imaging Radiat Oncol201559110911425088249
- OnishiHNousoKNakamuraSEfficacy of hepatic arterial infusion chemotherapy in combination with irradiation for advanced hepatocellular carcinoma with portal vein invasionHepatol Int20159110511225788384
- LiXLGuoWXHongXDEfficacy of the treatment of transarterial chemoembolization combined with radiotherapy for hepatocellular carcinoma with portal vein tumor thrombus: a propensity score analysisHepatol Res201646111088109826783741
- ChumaMTaguchiHYamamotoYEfficacy of therapy for advanced hepatocellular carcinoma: intra-arterial 5-fluorouracil and subcutaneous interferon with image-guided radiationJ Gastroenterol Hepatol20112671123113221501224
- LengJJXuYZDongJHEfficacy of transarterial chemoembolization for hepatocellular carcinoma with portal vein thrombosis: a meta-analysisANZ J Surg2016861081682025088384
- WuZJCaiJXuABCombined three-dimensional conformal radiotherapy plus transcatheter arterial chemoembolization and surgical intervention for portal vein tumor thrombus in patients with hepatocellular carcinomaZhonghua Yi Xue Za Zhi2011914028412844 Chinese22333546
- FornerAReigMEde LopeCRBruixJCurrent strategy for staging and treatment: the BCLC update and future prospectsSemin Liver Dis2010301617420175034
- PinterMHuckeFGraziadeiIAdvanced-Stage Hepatocellular Carcinoma: Transarterial Chemoembolization versus SorafenibRadiology2012263259059922438359
- EdelineJCrouzetLCampillogimenezBSelective internal radiation therapy compared with sorafenib for hepatocellular carcinoma with portal vein thrombosisEur J Nucl Med Mol Imaging201643463564326455499
- OzkanZGPoyanliAUcarAFavorable survival time provided with radioembolization in hepatocellular carcinoma patients with and without portal vein thrombosisCancer Biother Radiopharm201530313213825760644
- ParkSHKimJCKangMKTechnical advances in external radiotherapy for hepatocellular carcinomaWorld J Gastroenterol201622327311732127621577
- KangJNieQRuiDUStereotactic body radiotherapy combined with transarterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombosisMol Clin Oncol201421435024649306
- ChoiBOChoiIBHongSJStereotactic body radiation therapy with or without transarterial chemoembolization for patients with primary hepatocellular carcinoma: preliminary analysisBMC Cancer2008835119038025
- KimDYParkWLimDHThree-dimensional conformal radiotherapy for portal vein thrombosis of hepatocellular carcinomaCancer2005103112419242615822130
- ToyaRMurakamiRBabaYConformal radiation therapy for portal vein tumor thrombosis of hepatocellular carcinomaRadiother Oncol200784326627117716760
- HuoYREslickGDTranscatheter arterial chemoembolization plus radiotherapy compared with chemoembolization alone for hepatocellular carcinoma: a systematic review and meta-analysisJAMA Oncol20151675676526182200