Abstract
Angiotensin II (Ang II), part of the renin–angiotensin–aldosterone system (RAS), is a potent vasoconstrictor and has been recently approved for use by the US Food and Drug Administration in high-output shock. Though not a new drug, the recently published Angiotensin II for the Treatment of High Output Shock (ATHOS-3) trial, as well as a number of retrospective analyses have sparked renewed interest in the use of Ang II, which may have a role in treating refractory shock. We describe refractory shock, the unique mechanism of action of Ang II, RAS dysregulation in shock, and the evidence supporting the use of Ang II to restore blood pressure. Evidence suggests that Ang II may preferentially be of benefit in acute kidney injury and acute respiratory distress syndrome, where the RAS is known to be disrupted. Additionally, there may be a role for Ang II in cardiogenic shock, angiotensin converting enzyme inhibitor overdose, cardiac arrest, liver failure, and in settings of extracorporeal circulation.
Keywords:
Introduction
Circulatory shock is life-threatening, and is characterized by hypotension, tissue hypoperfusion, and inadequate cellular oxygen utilization.Citation1 The most common form of circulatory shock is vasodilatory shock, which accounts for two-thirds of cases and is associated with the risk of multi-organ failure and death.Citation2 A central tenet of the management of shock is the defense of the mean arterial pressure (MAP), which often requires vasopressor therapy. Traditionally, catecholamines and vasopressin have been used to achieve the MAP goal, sometimes at the risk of adverse events, including peripheral and splanchnic ischemia, dysrhythmias, and organ dysfunction.Citation3,Citation4 To date, no specific vasopressor has been shown to improve mortality. A 2016 Cochrane Review meta-analysis concluded that other than the potential arrhythmogenicity of dopamine, no vasopressor outperformed any other with respect to mortality.Citation5 Angiotensin II (Ang II) has been shown to increase blood pressure in patients with hypotensionCitation6 and has recently been approved by the US Food and Drug Administration as a vasopressor (Giapreza™; La Jolla Pharmaceutical Company, La Jolla, CA, USA) in the treatment of distributive shock. With this approval and the renewed interest in Ang II, there exists a need for better understanding of its mechanisms of action, risks and opportunities for use, and future areas of research.
Refractory shock
The concept of inadequate hemodynamic response to high doses of vasopressors is often referred to as refractory shock.Citation7 While no consensus definition exists, most efforts to delineate this level of illness highlight either failure of response to conventional therapyCitation8–Citation10 or increased levels of morbidity and mortality.Citation4,Citation11,Citation12 Refractory shock is common, occurring in, by some estimates, 6%–7% of critically ill patients,Citation13,Citation14 and mortality can range from 37% to 66%, depending on the definition used.Citation7 Catecholamines are traditionally used as first-line therapy in shockCitation15 and at higher doses, are strongly associated with mortality.Citation16–Citation19 Additionally, high-dose catecholamines may have toxic effects, contributing substantially to morbidityCitation20–Citation22 and may be an independent predictor of mortality.Citation23
The phenotype of refractory shock can be described as profound vasodilation and marked tissue hypoxia. Vasodilation is mediated by the presence of nitric oxide and the deficiency of important innate vasoactive peptides such as catecholamines, cortisol, vasopressin, and Ang II.Citation24–Citation28 The reduced catecholamine responsiveness seen in refractory shock may be a result of this dysfunction and deficiency at the subcellular level.Citation7 However, the process is not uniform – considerable microcirculatory heterogeneity exists, which can contribute to regional and organ-specific hypoxia.Citation29 Catecholamine therapy may also contribute to the maldistribution of blood flow and oxygenation.Citation30,Citation31 Defense of the MAP is the primary treatment goal, which is typically attempted with a myriad of therapeutic options, including catecholamine and non-catecholamine vasopressors, corticosteroids, and other rescue therapies.Citation15
Non-catecholamine vasopressor support has emerged as an important idea in the treatment of refractory shock.Citation32,Citation33 Catecholamine sparing, or the reduction of catecholamine doses with non-adrenergic alternatives, may reduce the potential toxicities associated with high doses of catecholamine therapy via vasoconstriction using alternative mechanisms of action. Mounting evidence suggests that multimodal blood pressure support with catecholamine and non-catecholamine therapies may improve outcomes, such as reduction of tachyarrhythmia and resolution of renal failure.Citation4,Citation34 Data are conflicting as to whether this practice improves mortality.Citation35–Citation39 This approach makes teleological sense – cardiovascular homeostasis in humans is maintained through the complex, yet harmonious, interplay between sympathetic tone and hormonal systems, including the renin–angiotensin–aldosterone (RAS) system and the arginine–vasopressin system. A detailed discussion of the role of vasopressin in refractory shock is beyond the scope of this paper, but can be found throughout the literature.Citation28,Citation35 Future studies will be required to determine whether or not the mimicking of this innate response via exogenous multi-modal therapy can translate into meaningful outcome-based endpoints.
The use of Ang II in shock
The randomized, controlled, double-blind, Phase 3 Angiotensin II for the Treatment of High-Output Shock (ATHOS-3) trial (ClinicalTrials.gov, NCT02338843) showed that Ang II significantly increased MAP vs placebo in patients with shock with a trend toward 28-day survival.Citation36 Patients included in this study were required to 1) have vasodilatory features (cardiac index >2.3 L/min/m2 or central venous oxygen saturation >70% coupled with central venous pressure >8 mmHg) and 2) be on high doses of standard-of-care vasopressors (>0.2 μg/kg/min of norepinephrine equivalent dose). Additionally, the vasopressor effects of Ang II have been demonstrated throughout the historical literature in patients with distributive, cardiogenic, and other forms of shock, including hypotension associated with chronic dialysis, angiotensin converting enzyme (ACE) inhibitor overdose and hypotension in the perioperative setting.Citation6 Multiple dose ranges have been studied including continuous infusions of 10 ng/kg/min to bolus dose therapy of 1,500 mcg. Appropriate doses, based on the currently available literature, appear to be in the range of 5 to 40 ng/kg/min.Citation6,Citation27,Citation36,Citation40
The use of Ang II in circulatory shock as part of a balanced approach, along with catecholamines and vasopressin, makes teleological sense. Ang II and the RAS system have evolved in conjunction with the arginine–vasopressin and sympathetic nervous systems over eons as part of human physiology to support blood pressure.Citation41,Citation42 Ang II does this through multiple mechanisms, including direct vasoconstriction of peripheral vessels, water reabsorption through potentiation of antidiuretic hormone, sodium retention via the synthesis of aldosterone, and through synergistic activity with catecholamines.Citation43,Citation44 During hypotension, the RAS is activated in response to decreased pressure and solute content in the kidney. The subsequent release of renin, Ang II, and aldosterone, as well as antidiuretic hormone and catecholamines acts to harmoniously restore blood pressure.Citation45,Citation46 There is some evidence to suggest that circulating levels of vasoactive peptides are decreased or dysfunctional in sepsis.Citation24 Replacement of these peptides exogenously forms the basis of treatment in shock.
The RAS system and physiology of Ang II
The RAS plays a vital role in blood pressure regulation, fluid and electrolyte balance, and preservation of volume status and vascular tone, which together influence arterial pressure and cardiac output. Located ubiquitously throughout the body, the RAS participates in the regulation of cardiovascular homeostasis as well as other processes via autocrine, paracrine, and endocrine mechanisms and a network of intracellular signaling pathways.Citation47 A schematic of the RAS is presented as .
Figure 1 The renin–angiotensin–aldosterone system.
Abbreviations: ACE, angiotensin converting enzyme; ADH, antidiuretic hormone.
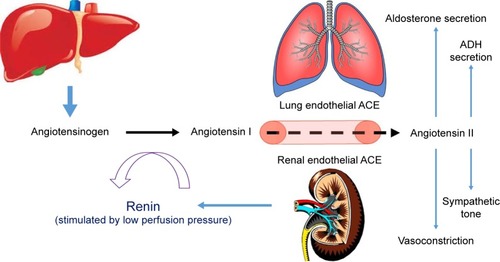
Renin is a proteolytic enzyme secreted from the juxtaglomerular apparatus of the kidney in response to activation of the sympathetic nervous system, reduction in afferent arterial pressure, or a drop in solute concentrations in the distal tubules.Citation48 Renin does not have any peripheral receptors and, therefore, does not directly affect hemodynamics, but does cleave angiotensinogen into angiotensin I (Ang I). Upregulation of renin synthesis occurs as a result of chronic RAS blockade (via ACE inhibition) and downregulation can occur in the presence of exogenous Ang II.Citation49,Citation50
Angiotensinogen is an α-glycoprotein produced by the liver and released into systemic circulation where it is transformed by renin converting it to Ang I. Ang I is then cleaved by ACE into Ang II. This occurs mostly by endothelial-bound ACE in the lungs, but can also occur in plasma as well as in the vascular bed of the kidneys, heart, and brain and, to a lesser extent, by chymases stored in granules in the mast cells.Citation48 ACE also plays a role in the degradation of bradykinin, which causes vasodilation and natriuresis.Citation51 A homologue of ACE named ACE2 is expressed in a more limited way throughout the body and efficiently hydrolyzes Ang II into angiotensin 1–7 (Ang 1–7), which opposes the actions of Ang II and causes vasodilation, natriuresis, and reduced blood pressure.Citation52,Citation53
Ang II, an octapeptide, has a myriad of physiologic effects, depending on the receptor type, which mediate cardiovascular, sodium, and water homeostasis. It is rapidly metabolized by aminopeptidase A and ACE2 to Ang 1–7 in plasma, erythrocytes, and many major organs.Citation130 Because of its rapid degradation, its half-life is ~30 seconds in the circulation; however, in the tissues, the half-life is extended to 15–30 minutes. Ang II regulates fluid and electrolytes and maintains hemodynamic stability by binding to specific angiotensin (AT) receptors on the cell membrane. The major physiologic effects in humans are mediated by the AT-1 receptor, which is located in the kidneys, vascular smooth muscle, lung, heart, brain, adrenal gland, pituitary gland, and liver. These effects include direct vasoconstriction (via receptors located in the endothelium of peripheral vessels), inotropy and cardiac remodeling (via receptors located in the myocardium), potentiation of the sympathetic nervous system, vasopressin release, regulation of the thirst mechanism (via receptors in the brain, sympathetic ganglia, and pituitary), and regulation of aldosterone release (via receptors in the adrenal gland).Citation54 AT-1 receptors have different subcellular signaling pathways, including G-coupled protein receptors (GPCRs) as well as a β-arrestins which, when activated by Ang II, carry out very different physiologic tasksCitation55 including the physiologically opposed effects of hypertension (via a GPCR mechanism) and hypotension (via a β-arrestin mechanism).Citation56 AT-2 receptors are expressed primarily in the vascular endothelium, brain, adrenals, and selected cutaneous, renal, and cardiac structures, and mediate antiproliferation, vasodilation, and anti-inflammation, and thereby antagonize the actions of the AT-1 receptor-mediated effects of Ang II. A discussion of some of the pharmacologic details pertaining to Ang II is provided in the Supplementary material.
Ang II is associated with myocardial ventricular remodeling in the setting of cardiac dysfunction or hypertension. A chronic increase in cardiac pressures produced by Ang II leads to hypertrophy and collagen deposition, and its blockade via ACE inhibition or AT receptor blocker therapy represents a cornerstone of cardiovascular protection against common disease states such as congestive heart failure (CHF) and hypertension.Citation57,Citation58 In addition to direct hypertrophic effects on smooth muscle cells, Ang II enhances sympathetic excitation, fibrogenesis, chemotaxis of fibroblasts, and inflammation, all of which contribute to remodeling.Citation59–Citation61 Patients with CHF can have elevated Ang II levels, despite commonly using ACE inhibition therapy, which is associated with increased morbidity and mortality.Citation62,Citation63 In contrast, patients with circulatory shock may exhibit a physiologic deficiency in Ang II.
The physiology of Ang II deficiency in shock
RAS dysregulation during sepsis is well described.Citation64,Citation65 The vasodilation seen in septic shock may be associated with activation of adenosine triphosphate (ATP)-sensitive potassium channels (KATP) in the vascular smooth muscle, which results from reduced cellular ATP or increased hydrogen and lactate concentrations.Citation66 Activation of KATP channels is known to inhibit Ang II–induced vasoconstriction.Citation67 RAS may be over- or understimulated, affecting both systemic and microcirculation, and varying levels of Ang I, Ang II, and renin have been reported in sepsis.Citation68–Citation70 Additionally, ACE levels in patients admitted with lung dysfunction are known to be reduced, compared to healthy controls.Citation71 ACE dysfunction in sepsis is thought to be the result of both pulmonary and vascular endothelial damage from inflammatory molecules and blood-borne substrates.Citation72 Additionally, endotoxins associated with gram-negative infections have the ability to inactivate ACE.Citation70 Studies have also demonstrated a down-regulation and dysfunction of both AT-1 and AT-2 receptors during septic shock.Citation73,Citation74 AT-1 downregulation may be a result of proinflammatory cytokines and nitric oxide production.Citation75 The downregulation of these receptors ultimately leads to decreases in catecholamine and aldosterone levels and the risk of hypotension.Citation47
Defects in ACE and AT receptors in sepsis suggest that a relative Ang II deficiency may be a root cause in the hemodynamic instability seen in sepsis. Low levels of Ang II and ACE in septic patients are associated with morbidity and mortality,Citation68 and there is evidence that replacement of physiologic levels of Ang II in septic shock is effective in reversing hemodynamic instability.Citation39 Based on early physiologic studies, a dose of 5 ng/kg/min of Ang II is thought to be analogous to replacement of physiologic serum levels,Citation76 and it was found that among the ATHOS-3 Ang II recipients, almost half (48.5%) responded to doses ≤5 ng/kg/min. Dose-related efficacy and safety parameters were compared, post hoc, in patients enrolled in the Ang II arm of the ATHOS-3 study and dichotomized based on doses of ≤5 vs >5 ng/kg/min. More patients receiving the lower dose (≤5 ng/kg/min) exhibited a blood pressure response compared to patients requiring >5 ng/kg/min, and this variable was independently predictive of response. The lower dose of Ang II was also associated with a mortality and morbidity benefit. This phenomenon is further supported in an analysis of ACE capacity and functionality within the ATHOS-3 population. The precursor and product of ACE (Ang I and Ang II, respectively) and the ratio of Ang I/II are reflective of ACE functionality.Citation77,Citation78 While the normal Ang I/II ratio is 0.5, the median ratio was 1.63 in patients in the ATHOS-3 study,Citation36 suggesting dysregulated ACE functionality in septic shock. In further post hoc analysis of ATHOS-3 patients with Ang I/II ratios of >1.63 (reflecting an Ang II deplete state and less ACE functionality), those receiving Ang II exhibited a mortality benefit compared to placebo, whereas patients with an Ang I/II ratio <1.63 (reflecting an Ang II replete state) receiving Ang II did not.Citation79 As such, hyperresponsiveness to a low dose of Ang II or a high Ang I/II ratio identifies those patients with ACE deficiency who would most benefit from Ang II administration.
Historical uses and risks associated with the use of Ang II
Ang II was discovered in the 1930s, but use was not reported in the literature until the early 1960s. In total, use is reported in >31,000 subjects, including healthy humans, as well as a diagnostic tool in the identification of pre-eclampsia, for enhancing delivery of chemotherapy to solid tumors, in prevention of hypotension during anesthesia, and for treatment of hypotension following ACE Inhibitor overdose.Citation40 Is has been given to patients suffering from numerous medical conditions, including pulmonary, renal, cardiovascular, endocrine, and hepatic failure, trauma, and malignancy.
In the obstetric population, Ang II was used to treat hypotension and compared favorably to ephedrine with regard to uterine oxygen delivery and pH levels.Citation80–Citation82 Similarly, the acid–base status in neonates of women given Ang II was better than with ephedrine infusions.Citation83 Additionally, Ang II was used to risk-stratify pregnant women at risk for pre-eclampsia,Citation84,Citation85 who have high levels of circulating estrogen. Estrogen induces AGT gene transcription in the liver (which makes angiotensinogen), and the M235T variant is associated with pre-eclampsia.Citation48 Moreover, the ratio of reduced to oxidized Ang II in pre-eclamptic women is different from healthy pregnant women, and RAS dysregulation was thought to elucidate the hypertension seen in pre-eclampsia.
Ang II is physiologically a rational treatment for hypotension following ACE inhibitor overdose. Exogenous infusion of Ang II restores the innate deficiency resulting from the inhibition of ACE. Several case studies have shown successful resolution of hypotension in ACE inhibitor overdose with Ang II.Citation86–Citation88 In these reports, patients were refractory to other treatment modalities, but experienced a profound increase in blood pressure upon receiving the drug.
Ang II has been used to enhance the delivery of chemo-and radiation therapy to solid tumors.Citation89,Citation90 By selectively increasing blood flow to tumor tissue with Ang II, investigators were able to simulate hyperbaric oxygenation radiation therapy, thus improving tumor response and minimizing healthy tissue damage.Citation89 Additionally, chemotherapy delivery was found to be enhanced via selective Ang II-induced hypertension, resulting in reduction of tumor size and less toxicity.Citation91 Mechanistically, the increase of tumor blood flow caused by Ang II was thought to demonstrate a loss of autoregulation and allow for increased delivery of therapy to the tumor.Citation92 Despite the aforementioned investigations, there have been no recent reports of this use of Ang II.
Physiologic effects, side effects, and adverse events of Ang II were evaluated in a large systematic review of safety.Citation40 Common findings included increased systemic and pulmonary blood pressure, reduced heart rate and cardiac output, and decreased renal blood flow and glomerular filtration rate. Additionally, investigators cited increased plasma aldosterone and other endocrine perturbations, alterations of electrolyte balance, and reduction in sodium and water excretion. Common side effects in the literature included headache, sensation of chest pressure, dyspepsia, and orthostatic hypotension upon cessation of the drug. Ang II was found to worsen bronchoconstriction during an asthma exacerbationCitation93–Citation95 and worsen ventricular function when administered to patients with acute CHF.Citation96 Two deaths were found to be attributable to Ang II, including that of a 36-year-old healthy male who died of a hypertensive cerebral hemorrhage while receiving a 6-day infusion of Ang II,Citation97 and that of a patient with pre-infusion symptoms of acute heart failure who failed to respond to Ang II during profound cardiogenic shock.Citation96 While the adverse event rates were similar in the patients studied in ATHOS-3 (excluded from the aforementioned review), the incidence rates of thromboembolic events, delirium, and infection were higher in the Ang II cohort.Citation36 While speculative at this time, it is plausible that immune dysregulation, alterations in microvascular blood flow, and the prothrombotic potential of Ang II may be causative. Further analyses are required to more clearly elucidate these potential areas of concern, and proper precaution is warranted in patients at risk for these conditions.
Ang II in acute kidney injury patients
Acute kidney injury (AKI) in septic shock is associated with poor outcomes.Citation98 Mortality in patients with AKI who require renal replacement therapy can reach 50%.Citation99,Citation100 Though a common occurrence,Citation101 the mechanisms involved in the development of sepsis-induced AKI are incompletely understood. It is thought that sepsis-induced AKI results in part not only from decreased renal perfusion in the setting of hypotension,Citation102 but also from renal microvascular dysregulation and shunting, inflammatory and immune activation, and cell-cycle arrest.Citation103–Citation105 Systemic hypotension and intrarenal vasodilation are accompanied by a reduction in glomerular filtration rate due to reduced intra-glomerular perfusion pressure.Citation106 Vasopressors, vasodilators, inotropes, and natriuretic peptides have failed to demonstrate improved outcomes in AKI.Citation107,Citation108 In the renal microcirculation, Ang II preferentially constricts efferent arteriolar tone, more so than the afferent tone, thereby restoring glomerular perfusion pressureCitation109,Citation110 and may have a unique role in sepsis-associated AKI. In an animal model, Ang II was found to restore systemic blood pressure, though with a concomitant decrease in renal blood flow.Citation106 However, despite this decrease, animals receiving Ang II exhibited improved urinary output and creatinine clearance. The beneficial effects on renal function have been found in other pre-clinical work as well,Citation111,Citation112 though in clinical practice, results are equivocal.Citation27,Citation87,Citation113–Citation115
Ang II has recently been evaluated in patients with septic shock, as part of a post hoc analysis of ATHOS-3.Citation34 Patients with shock and AKI requiring renal replacement were found to have improved 28-day survival, improved renal recovery (liberation from renal replacement therapy at day 7), fewer days on ventilation, and shorter intensive care unit and hospital length of stay. These results suggest that the AKI seen in septic shock is, at least in part, due to decreased glomerular perfusion, and that Ang II may mitigate this phenomenon. The microcirculatory properties of Ang II are not seen when using other vasopressors which do not reverse the phenotypical pattern of efferent vasodilation at the level of the glomerulus.Citation103 Further supporting this is that pre-morbid RAS manipulation with ACE inhibition or AT receptor blocker therapy (which causes efferent arteriolar dilatation) increases the risk of sepsis-induced AKI.Citation116 There remains continued interest in the manipulation of the RAS system to improve renal outcomes in septic shock.Citation117
Ang II in acute respiratory distress syndrome patients
Some patients with septic shock also have acute respiratory distress syndrome (ARDS), which may in part be due to similar or linked pathophysiologic mechanisms between the two syndromes.Citation118 The hallmark of ARDS is pulmonary endothelial injury and accumulation of protein-rich fluid inside the alveoli, which is due to increased pulmonary capillary permeability. Endothelium-bound ACE converts Ang I into Ang II,Citation119 and in conditions of significant lung injury, reductions in this enzymatic process may result in decreased levels of Ang II.Citation120 Supplementation with exogenous Ang II has been shown to be effective in supporting hemodynamics in patients with ARDS.Citation33,Citation36
In a post hoc analysis using data from the ATHOS-3 population, the efficacy of Ang II was evaluated in patients with septic shock and ARDS.Citation121 Patients with ARDS based on the Berlin criteriaCitation122 at the time of study drug initiation were analyzed for blood pressure response and clinical outcomes. Almost three-quarters of the patients enrolled in ATHOS-3 had some degree of lung injury, and a greater proportion of lung-injured patients treated with Ang II experienced a blood pressure response compared to placebo. Moreover, the blood pressure response was most evident in patients with severe ARDS. While 28-day mortality increased in both the Ang II group and the placebo group with increasing ARDS severity, the progression in the rate of mortality by ARDS severity was lower in the Ang II group and the magnitude of the 28-day mortality benefit was most evident in severe ARDS ().
Figure 2 Progressive Kaplan–Meier analysis of the mortality effect of Ang II in patients with ARDS.
Abbreviations: Ang II, angiotensin II; ARDS, acute respiratory distress syndrome.
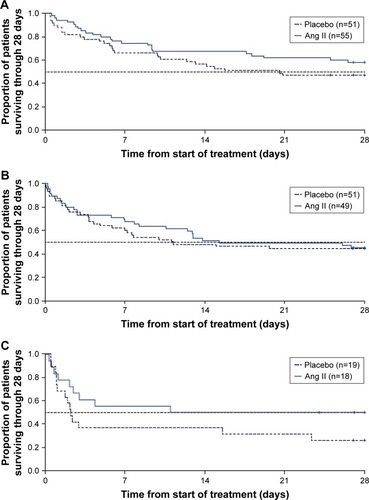
The findings in this analysis suggest that exogenous Ang II may be beneficial in reversing the hemodynamic compromise in patients with ARDS and septic shock. The pulmonary vascular endothelium is essential for the synthesis and degradation of Ang II, and it has been demonstrated that ACE activity is altered in severe lung injury, and this dysfunction correlates with the severity of the disease.Citation72 While incompletely understood, other components of the RAS, including ACE homologues such as ACE2, may play a role in modulation of disease in ARDS.Citation123,Citation124 Further research is needed to more fully understand the unique role for Ang II in ARDS.
Future directions
Ang II has been well studied in distributive shock, but may play a role in other disease states as well. Some data have suggested that Ang II may be beneficial in both cardiogenic shock and cardiac arrest. Though data are limited, patients with cardiogenic shock who received Ang II infusion experienced robust improvement in blood pressure.Citation6 Like patients with septic shock, patients with cardiogenic shock may exhibit RAS dysregulation via “ACE escape”, whereby the levels of Ang I, Ang II, renin, and ACE are altered in the setting of pre-morbid ACE inhibition.Citation62,Citation63 In a historical analysis of the use of Ang II in shock, five patients with heart failure who had pre-morbid ACE inhibitor exposure experienced a dramatic improvement in blood pressure when receiving Ang II for cardiogenic shock.Citation6 The restoration of hemodynamic stability with intravenous Ang II in this patient population suggests both a role for Ang II in cardiogenic shock as well as ACE inhibitor overdose, the latter of which has been reported in the literature.Citation86–Citation88
In an analysis of the historical literature, 14 patients with presumed cardiac arrest were found to have a profound blood pressure effect upon return of spontaneous circulation after administration of Ang II.Citation6 The authors hypothesized that successful resuscitation and normalization of blood pressure may have been from a number of potential mechanisms, including restoration of blood flow to vital organs, increased inotropy, potentiation of catecholamines, or improved coronary perfusion. To date, no human trials have sought to evaluate Ang II in cardiac arrest, but Ang II levels were evaluated in a porcine model of cardiac arrest and found to be elevated.Citation125 The influence of Ang II on the RAS system during cardiac arrest is a potential target for future investigation.
Ang II may preferentially reverse shock in a number of disease states which, by their nature, can be associated with RAS dysregulation. Patients with liver failure or cirrhosis, for example, have impaired synthesis of angiotensinogenCitation126,Citation127 and may respond well to exogenous Ang II. Likewise, in patients receiving extracorporeal circulation support (cardiopulmonary bypass), circumvention of the pulmonary circulation is associated with altered ACE levelsCitation128,Citation129 may be associated with increased Ang II sensitivity. Presumably, patients on extracorporeal membrane oxygenation circuits would exhibit similar ACE dysfunction, though there is no data describing this as of yet. describes the current and contemplated uses of Ang II.
Table 1 Current and contemplated uses of Ang II
Conclusion
Ang II is a potent vasoconstrictor and part of the RAS, a highly conserved system involved in blood pressure control, fluid and electrolyte homeostasis, and hormonal activity in humans. Recently approved for use as a novel vasopressor in high-output shock, Ang II may prove to be a beneficial addition to the armamentarium against refractory shock by virtue of its unique mechanism of action, which is complementary to that of the currently available therapies. RAS dysregulation in shock is common, and evidence suggests that exogenous Ang II may reverse the deficiency seen in many patients with this syndrome. Multiple studies have evaluated Ang II, which has been shown to restore blood pressure in septic shock and may preferentially be of benefit in AKI and ARDS. Additionally, there may be a role for Ang II in cardiogenic shock, ACE inhibitor overdose, and cardiac arrest, which may be evaluated in future research efforts.
Supplementary materials
Pharmacology of Ang II
Giapreza® (angiotensin II) was approved by the US Food and Drug Administration in December 2017 with a labeled indication for increasing blood pressure in adults with septic or other distributive shock. The medication is to be administered via continuous intravenous infusion with a starting rate, per the label, of 20 ng/kg/min and titrated every 5 minutes by increments of up to 15 ng/kg/minute as needed.Citation1 Although off label, an initial starting rate of 10 ng/kg/min has been suggested, since some patients may respond with a rapid increase in blood pressure. The initial maximum infusion rate is 80 ng/kg/min within the first 3 hours, with a maximum maintenance infusion rate of 40 ng/kg/min.Citation1 Because of the unique metabolism and very short half-life of <1 minute, Giapreza does not need to be dose adjusted for renal or hepatic impairment.Citation2
Giapreza is available as a 2.5 mg/1 mL vial to be diluted in normal saline to a final concentration of 5,000 or 10,000 ng/mL for fluid-restricted patients.Citation1 Vials may be stored at 2°C–8°C, and compounded drips may be stored diluted at room temperature or under refrigeration for no longer than 24 hours.Citation2 Giapreza has intravenous compatibility with other vasopressors.Citation2 Adverse reactions include thrombosis, tachycardia, deep vein thrombosis, peripheral ischemia, delirium, acidosis, hyperglycemia, thrombocytopenia, fungal infection.Citation1 Of note, these adverse reactions are the result of combination therapy with other vasopressors. Drug interactions include angiotensin converting enzyme inhibitors and angiotensin receptor blockers.Citation2 There are no contraindications listed in the manufacturer’s labeling.
References
- Giapreza [angiotensin II] [prescribing information]San Diego, CALa Jolla Pharmaceutical Company122017
- Giapreza Lexi-Drugs Lexicomp Online [database online]Hudson, OHLexi-Comp, Inc2018 Available from: http://online.lexi.com/lco/action/doc/retrieve/docid/patch_f/6582570Accessed March 26, 2018
Disclosure
LWB reports receiving consulting fees from La Jolla Pharmaceutical Company. The authors report no other conflicts of interest in this work.
References
- VincentJ-Lde BackerDCirculatory ShockN Engl J Med Overseas Ed20133691817261734
- de BackerDBistonPDevriendtJComparison of Dopamine and Norepinephrine in the Treatment of ShockN Engl J Med Overseas Ed20103629779789
- SchmittingerCATorgersenCLucknerGSchröderDCHLorenzIDünserMWAdverse cardiac events during catecholamine vasopressor therapy: a prospective observational studyIntensive Care Med201238695095822527060
- DünserMWMayrAJUlmerHArginine Vasopressin in Advanced Vasodilatory Shock: A Prospective, Randomized, Controlled StudyCirculation2003107182313231912732600
- GamperGHavelCArrichJVasopressors for hypotensive shockCochrane Database Syst Rev2016339Cd003709
- BusseLWMccurdyMTAliOHallAChenHOstermannMThe effect of angiotensin II on blood pressure in patients with circulatory shock: a structured review of the literatureCritical Care201721132429282149
- JentzerJCVallabhajosyulaSKhannaAKChawlaLSBusseLWKashaniKBManagement of Refractory Vasodilatory ShockChest Epub201819
- BassiEParkMAzevedoLCPTherapeutic Strategies for High-Dose Vasopressor-Dependent ShockCrit Care Res Pract20132013265470865471024151551
- LucknerGDünserMWJochbergerSArginine vasopressin in 316 patients with advanced vasodilatory shockCrit Care Med200533112659266616276194
- BrownSMLanspaMJJonesJPSurvival After Shock Requiring High-Dose Vasopressor TherapyChest2013143366467122911566
- LucknerGMayrVDJochbergerSComparison of two dose regimens of arginine vasopressin in advanced vasodilatory shockCrit Care Med200735102280228517944015
- TorgersenCDünserMWWenzelVComparing two different arginine vasopressin doses in advanced vasodilatory shock: a randomized, controlled, open-label trialIntensive Care Med2010361576519756505
- BenbenishtyJWeissmanCSprungCLBrodsky-IsraeliMWeissYCharacteristics of patients receiving vasopressorsHeart & Lung: The Journal of Acute and Critical Care201140324725220630594
- JenkinsCRGomersallCDLeungPJoyntGMOutcome of patients receiving high dose vasopressor therapy: a retrospective cohort studyAnaesth Intensive Care200937228628919400494
- RhodesAEvansLEAlhazzaniWSurviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016Intensive Care Med201743330437728101605
- MayrVDDünserMWGreilVCauses of death and determinants of outcome in critically ill patientsCritical Care2006106R15417083735
- JentzerJCCoonsJCLinkCBSchmidhoferMPharmacotherapy Update on the Use of Vasopressors and Inotropes in the Intensive Care UnitJ Cardiovasc Pharmacol Ther201520324926025432872
- VincentJLMorenoRTakalaJThe SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care MedicineIntensive Care Med19962277077108844239
- DünserMWRuokonenEPettiläVAssociation of arterial blood pressure and vasopressor load with septic shock mortality: a post hoc analysis of a multicenter trialCritical Care2009136R18119917106
- DünserMWHasibederWRSympathetic Overstimulation During Critical Illness: Adverse Effects of Adrenergic StressJ Intensive Care Med200924529331619703817
- AndreisDTSingerMCatecholamines for inflammatory shock: a Jekyll-and-Hyde conundrumIntensive Care Med20164291387139726873833
- AsfarPMezianiFHamelJ-FHigh versus Low Blood-Pressure Target in Patients with Septic ShockN Engl J Med Overseas Ed20143701715831593
- SviriSHashoulJStavIvan HeerdenPVDoes high-dose vasopressor therapy in medical intensive care patients indicate what we already suspect?J Crit Care201429115716024140297
- LevyBCollinSSennounNVascular hyporesponsiveness to vasopressors in septic shock: from bench to bedsideIntensive Care Med201036122019202920862451
- HosseinianLWeinerMLevinMAFischerGWMethylene Blue: Magic Bullet for Vasoplegia?Anesth Analg2016122119420126678471
- MarikPEPastoresSMAnnaneDRecommendations for the diagnosis and management of corticosteroid insufficiency in critically ill adult patients: Consensus statements from an international task force by the American College of Critical Care MedicineCrit Care Med20083661937194918496365
- ChawlaLSBusseLBrasha-MitchellEIntravenous angiotensin II for the treatment of high-output shock (ATHOS trial): a pilot studyCritical Care201418553425286986
- RussellJABench-to-bedside review: Vasopressin in the management of septic shockCritical Care2009154226
- WalleyKRHeterogeneity of oxygen delivery impairs oxygen extraction by peripheral tissues: theoryJ Appl Physiol19968128858948872660
- de BackerDCreteurJDuboisM-JThe effects of dobutamine on microcirculatory alterations in patients with septic shock are independent of its systemic effectsCrit Care Med200634240340816424721
- de BackerDCreteurJSilvaEVincentJ-LEffects of dopamine, norepinephrine, and epinephrine on the splanchnic circulation in septic shock: Which is best?Crit Care Med20033161659166712794401
- AsfarPRussellJATuckermannJRadermacherPSelepressin in Septic Shock: A Step Toward Decatecholaminization?Crit Care Med201644123423626672929
- ChawlaLSBusseLWBrasha-MitchellEAlotaibiZThe use of angiotensin II in distributive shockCritical Care201620113727230465
- TumlinJAMuruganRDeaneAMOutcomes in Patients with Vasodilatory Shock and Renal Replacement Therapy Treated with Intravenous Angiotensin IICrit Care Med201846694995729509568
- RussellJAWalleyKRSingerJVasopressin versus Norepinephrine Infusion in Patients with Septic ShockN Engl J Med Overseas Ed20083589877887
- KhannaAEnglishSWWangXSAngiotensin II for the Treatment of Vasodilatory ShockN Engl J Med Overseas Ed20173775419430
- RussellJALeeTSingerJBoydJHWalleyKRThe Septic Shock 3.0 Definition and Trials: A Vasopressin and Septic Shock Trial ExperienceCrit Care Med201745694094828333757
- SzerlipHBihoracAChangSEffect of disease severity on survival in patients receiving angiotensin II for vasodilatory shockCrit Care Med20184613868
- MccurdyMBGongLBoldtMAssociation of angiotensin II dose with all-cause mortality in patients with vasodilatory shockCritical Care201822Suppl 182
- BusseLWWangXSChalikondaDMClinical Experience With IV Angiotensin II Administration: A Systematic Review of SafetyCrit Care Med20174581285129428489648
- FournierDLuftFCBaderMGantenDAndrade-NavarroMAEmergence and evolution of the renin–angiotensin–aldosterone systemJ Mol Med201290549550822527880
- KuntzAThe evolution of the sympathetic nervous system in vertebratesJ Comp Neurol1911213215236
- BenigniACassisPRemuzziGAngiotensin II revisited: new roles in inflammation, immunology and agingEMBO Mol Med20102724725720597104
- ZhuoJLLiXCXcLNew insights and perspectives on intrarenal renin-angiotensin system: Focus on intracrine/intracellular angiotensin IIPeptides20113271551156521699940
- RolihCAOberKPThe endocrine response to critical illnessMed Clin North Am19957912112247808093
- du CheyronDLesageADaubinCRamakersMCharbonneauPHyperreninemic hypoaldosteronism: a possible etiological factor of septic shock-induced acute renal failureIntensive Care Med200329101703170914551679
- HallABusseLWOstermannMAngiotensin in Critical CareCritical Care20182216929558991
- SparksMACrowleySDGurleySBMirotsouMCoffmanTMClassical Renin-Angiotensin system in kidney physiologyCompr Physiol2014431201122824944035
- TimmermansPBWongPCChiuATAngiotensin II receptors and angiotensin II receptor antagonistsPharmacol Rev19934522052518372104
- KurtzAPfeilschifterJHutterARole of protein kinase C in inhibition of renin release caused by vasoconstrictorsAm J Physiol Cell Physiol19862504C563C571
- MargoliusHSKallikreins and Kinins: Molecular Characteristics and Cellular and Tissue ResponsesDiabetes199645Suppl 1S14S19
- DonoghueMHsiehFBaronasEA Novel Angiotensin-Converting Enzyme-Related Carboxypeptidase (ACE2) Converts Angiotensin I to Angiotensin 1-9Circ Res2000875e1e910969042
- FerrarioCMBrosnihanKBDizDIAngiotensin-(1-7): a new hormone of the angiotensin systemHypertension1991185_SupplIII126III1331937675
- PaulMPoyan MehrAKreutzRPhysiology of Local Renin-Angiotensin SystemsPhysiol Rev200686374780316816138
- ShenoySKLefkowitzRJAngiotensin II-stimulated signaling through G proteins and beta-arrestinSci STKE20052005311cm1416304060
- DewireSMViolinJDBiased Ligands for Better Cardiovascular Drugs: Dissecting G-Protein-Coupled Receptor PharmacologyCirc Res2011109220521621737816
- FelkerGMButlerJCollinsSPHeart failure therapeutics on the basis of a biased ligand of the angiotensin-2 type 1 receptor. Rationale and design of the BLAST-AHF study (Biased Ligand of the Angiotensin Receptor Study in Acute Heart Failure)JACC Heart Failure20153319320125650371
- FerrarioCMSchiffrinELRole of Mineralocorticoid Receptor Antagonists in Cardiovascular DiseaseCirc Res2015116120621325552697
- DavissonRLOliverioMICoffmanTMSigmundCDDivergent functions of angiotensin II receptor isoforms in the brainJ Clin Invest2000106110310610880053
- GeisterferAAPeachMJOwensGKAngiotensin II induces hypertrophy, not hyperplasia, of cultured rat aortic smooth muscle cellsCirc Res19886247497563280155
- IntenganHDSchiffrinELVascular remodeling in hypertension: roles of apoptosis, inflammation, and fibrosisHypertension2001383 Pt 258158711566935
- RoigEPerez-VillaFMoralesMClinical implications of increased plasma angiotensin II despite ACE inhibitor therapy in patients with congestive heart failureEur Heart J2000211535710610744
- van de WalRMAPlokkerHWMLokDJADeterminants of increased angiotensin II levels in severe chronic heart failure patients despite ACE inhibitionInt J Cardiol2006106336737216337046
- DoerschugKCDelsingASSchmidtGAAshareARenin-angiotensin system activation correlates with microvascular dysfunction in a prospective cohort study of clinical sepsisCritical Care2010141R2420175923
- AntonucciEGleesonPJAnnoniFAngiotensin II in Refractory Septic ShockShock201747556056627879559
- LandryDWOliverJAThe Pathogenesis of Vasodilatory ShockN Engl J Med Overseas Ed20013458588595
- QuayleJMNelsonMTStandenNBATP-sensitive and inwardly rectifying potassium channels in smooth musclePhysiol Rev1997774116512329354814
- ZhangWEIChenXHuangLSevere sepsis: Low expression of the renin-angiotensin system is associated with poor prognosisExp Ther Med2014751342134824940436
- DongLWChangYZTongLJTangJJySTangCSRole of regulatory peptide in pathogenesis of shockScience in China Series B, Chemistry, Life Sciences & Earth Sciences1994372162169
- DunnCWHortonJWRole of angiotensin II in neonatal sepsisCirc Shock19934021441508508519
- CaseyLKriegerBKohlerJRiceCOparilSSzidonPDecreased serum angiotensin converting enzyme in adult respiratory distress syndrome associated with sepsis: a preliminary reportCrit Care Med1981996516546268354
- OrfanosSEArmaganidisAGlynosCPulmonary Capillary Endothelium-Bound Angiotensin-Converting Enzyme Activity in Acute Lung InjuryCirculation2000102162011201811034953
- SchmidtCHöcherlKKurtBMoritzSKurtzABucherMBlockade of multiple but not single cytokines abrogates downregulation of angiotensin II type-I receptors and anticipates septic shockCytokine2010491303819914088
- BucherMHobbhahnJKurtzANitric oxide-dependent downregulation of angiotensin II type 2 receptors during experimental sepsisCrit Care Med20012991750175511546977
- BucherMIttnerK-PHobbhahnJTaegerKKurtzADownregulation of Angiotensin II Type 1 Receptors During SepsisHypertension200138217718211509472
- WolfRLMendlowitzMGitlowSENaftchiNMetabolism of Angiotensin II-I131 in Normotensive and Hypertensive Human SubjectsCirculation196123575475813786291
- LuqueMMartinPMartellNFernandezCBrosnihanKBFerrarioCMEffects of captopril related to increased levels of prostacyclin and angiotensin-(1-7) in essential hypertensionJ Hypertens19961467998058793704
- AziziMChatellierGGuyeneT-TMurieta-GeoffroyDMenardJAdditive Effects of Combined Angiotensin-Converting Enzyme Inhibition and Angiotensin II Antagonism on Blood Pressure and Renin Release in Sodium-Depleted NormotensivesCirculation19959248258347641363
- WunderinkRABusseTDeaneLBaseline angiotensin levels and ACE effects in patients with vasodilatory shock treated with angiotensin IIIntensive Care Medicine Experimental20175Suppl 20703
- RosenfeldCRNadenRPUterine and nonuterine vascular responses to angiotensin II in ovine pregnancyAm J Physiol Heart Circ Physiol19892571H17H24
- RaminSMRaminKDCoxKMagnessRRShearerVEGantNFComparison of prophylactic angiotensin II versus ephedrine infusion for prevention of maternal hypotension during spinal anesthesiaAm J Obstet Gynecol199417137347398092223
- NadenRPRosenfeldCREffect of angiotensin II on uterine and systemic vasculature in pregnant sheepJ Clin Invest19816824684747263862
- VincentRDWerhanCFNormanPFProphylactic Angiotensin II Infusion during Spinal Anesthesia for Elective Cesarean DeliveryAnesthesiology1998886147514799637639
- ContiCTranquilliALGarzettiGGRomaniniCModulation of vascular reactivity after acute calcium antagonist administration in pregnant women moderately sensitive to angiotensin infusionBollettino della Societa italiana di biologia sperimentale19947010–112432487702827
- ÖneyTKaulhausenHThe value of the angiotensin sensitivity test in the early diagnosis of hypertensive disorders in pregnancyAm J Obstet Gynecol1982142117207055166
- JacksonTCorkeCAgarJEnalapril overdose treated with angiotensin infusionThe Lancet19933418846703
- NewbyDELeeMRGrayAJBoonNAEnalapril overdose and the corrective effect of intravenous angiotensin II [letter]Br J Clin Pharmacol19954011031048527259
- TrilliLEJohnsonKALisinopril Overdose and Management with Intravenous Angiotensin IIAnn Pharmacother19942810116511687841571
- KatoTMurakamiYSaitoYNew modality of radiation therapy under increased tumor oxygen tension with angiotensin II: a pilot studyRadiat Med199311386908372242
- SatoHSugiyamaKHoshiMUrushiyamaMIshizukaKAngiotensin II (AII) induced hypertension chemotherapy (IHC) for unresectable gastric cancer: With reference to resection after down stagingWorld J Surg19951968368428553675
- NagamitsuAGreishKMaedaHElevating blood pressure as a strategy to increase tumor-targeted delivery of macromolecular drug SMANCS: cases of advanced solid tumorsJpn J Clin Oncol2009391175676619596662
- TomuraNKatoTKannoIIncreased blood flow in human brain tumor after administration of angiotensin II: demonstration by PETComput Med Imaging Graph19931764434498287355
- MillarEAAngusRMHulksGMortonJJConnellJMThomsonNCActivity of the renin-angiotensin system in acute severe asthma and the effect of angiotensin II on lung functionThorax19944954924958016772
- MillarEANallyJEThomsonNCAngiotensin II potentiates methacholine-induced bronchoconstriction in human airway both in vitro and in vivoEur Respir J1995811183818418620948
- RamsaySGClaytonRADaggKDThomsonLJNallyJEThomsonNCEffect of angiotensin II on histamine-induced bronchoconstriction in the human airway both in vitro and in vivoRespir Med199791106096159488894
- CohnJNLuriaMHStudies in clinical shock and hypotension. II. Hemodynamic effects of norepinephrine and angiotensinJ Clin Invest19654491494150414332162
- AmesRPBorkowskiAJSicinskiAMLaraghJHProlonged infusions of angiotensin II and norepinephrine and blood pressure, electrolyte balance, and aldosterone and cortisol secretion in normal man and in cirrhosis with ascitesJ Clin Invest19654471171118614328394
- JoannidisMDrumlWForniLGPrevention of acute kidney injury and protection of renal function in the intensive care unit: update 2017: Expert opinion of the Working Group on Prevention, AKI section, European Society of Intensive Care MedicineIntensive Care Medicine201743673074928577069
- GaudrySHajageDSchortgenFInitiation strategies for renal-replacement therapy in the intensive care unitN Engl J Med Overseas Ed20163752122133
- ZarbockAKellumJASchmidtCEffect of early vs delayed initiation of renal replacement therapy on mortality in critically Ill patients with acute kidney injuryJAMA2016315202190219927209269
- ZarjouAAgarwalASepsis and acute kidney injuryJ Am Soc Nephrol2011226999100621566052
- LangenbergCBagshawSMMayCNBellomoRThe histopathology of septic acute kidney injury: a systematic reviewCrit Care2008122R3818325092
- LankadevaYRKosakaJEvansRGBaileySRBellomoRMayCNIntrarenal and urinary oxygenation during norepinephrine resuscitation in ovine septic acute kidney injuryKidney Int201690110010827165831
- ChenHBusseLWNovel therapies for acute kidney injuryKidney Int Rep20172578579929270486
- SchrierRWWangWPooleBMitraAAcute renal failure: definitions, diagnosis, pathogenesis, and therapyJ Clin Invest2004114151415232604
- WanLLangenbergCBellomoRMayCNAngiotensin II in experimental hyperdynamic sepsisCrit Care2009136R19019948019
- Herget-RosenthalSSanerFChawlaLSApproach to hemodynamic shock and vasopressorsClin J Am Soc Nephrol20083254655318256381
- GordonACMasonAJThirunavukkarasuNEffect of early vasopressin vs norepinephrine on kidney failure in patients with septic shock: The VANISH randomized clinical trialJAMA2016316550951827483065
- AbueloJGNormotensive ischemic acute renal failureN Engl J Med2007357879780517715412
- ProwleJRBellomoRSepsis-associated acute kidney injury: macrohemodynamic and microhemodynamic alterations in the renal circulationSemin Nephrol2015351647425795500
- LankadevaYRKosakaJEvansRGBellomoRMayCNUrinary Oxygenation as a Surrogate Measure of Medullary Oxygenation During Angiotensin II Therapy in Septic Acute Kidney InjuryCrit Care Med2018461e41e4829077618
- BrennerMSchaerGLMalloryDLSuffrediniAFParrilloJEDetection of renal blood flow abnormalities in septic and critically ill patients using a newly designed indwelling thermodilution renal vein catheterChest19909811701792361386
- ThomasVLNielsenMSAdministration of angiotensin II in refractory septic shockCrit Care Med1991198108410851860334
- TovarJLBujonsIRuizJCIbañezLSalgadoATreatment of severe combined overdose of calcium antagonists and converting enzyme inhibitors with angiotensin IINephron19977722399346394
- WrayGMCoakleyJHSevere septic shock unresponsive to noradrenalineLancet1995346899016047500755
- SuberviolaBRodrigoEGonzález-CastroASerranoMHerasMCastellanos-OrtegaÁAssociation between exposure to angiotensin-converting enzyme inhibitors and angiotensin receptor blockers prior to septic shock and acute kidney injuryMed Intensiva2017411212728341094
- CorrêaTDTakalaJJakobSMAngiotensin II in septic shockCrit Care2015199825886853
- UmbrelloMFormentiPBolgiaghiLChiumelloDCurrent Concepts of ARDS: A Narrative ReviewInt J Mol Sci201618164
- RyanJWProcessing of endogenous polypeptides by the lungsAnnu Rev Physiol1982442412556176181
- OrfanosSELanglebenDKhouryJPulmonary capillary endothelium-bound angiotensin-converting enzyme activity in humansCirculation199999121593159910096936
- BusseLAGongTThompsonMOutcomes in patients with acute respiratory distress syndrome receiving angiotensin II for vasodilatory shockCritical Care201822Suppl 182
- ARDS Definition Task ForceRanieriVMRubenfeldGDThompsonBTAcute respiratory distress syndrome: the Berlin DefinitionJAMA2012307232526253322797452
- ImaiYKubaKRaoSAngiotensin-converting enzyme 2 protects from severe acute lung failureNature2005436704711211616001071
- LambertDWHooperNMTurnerAJAngiotensin-converting enzyme 2 and new insights into the renin-angiotensin systemBiochem Pharmacol200875478178617897633
- WangGZhangQYuanWWuJLiCEnalapril protects against myocardial ischemia/reperfusion injury in a swine model of cardiac arrest and resuscitationInt J Mol Med20163851463147327633002
- ArnalJFCudekPPlouinPFGuyenneTTMichelJBCorvolPLow angiotensinogen levels are related to the severity and liver dysfunction of congestive heart failure: implications for renin measurementsAm J Med199190117221824738
- ImaiMSokabeHPlasma renin and angiotensinogen levels in pathological states associated with oedemaArch Dis Child1968432304754794299072
- FaymonvilleMELarbuissonRRadermeckerMLimetRFournyJLamyMSerum activity of angiotensin converting enzyme during extra-corporeal circulation in manC R Seances Soc Biol Fil198317722522586309338
- PanagiotopoulosIPalatianosGMichalopoulosAChatzigeorgiouAPrapasSKamperEFAlterations in biomarkers of endothelial function following on-pump coronary artery revascularizationJ Clin Lab Anal201024638939821089169
- GiaprezaLexi-Drugs Lexicomp Online [database online]Hudson, OHLexi-Comp, Inc2018 Available from: http://online.lexi.com/lco/action/doc/retrieve/docid/patch_f/6582570Accessed March 26, 2018
- BusseLAGongTThompsonMOutcomes in patients with acute respiratory distress syndrome receiving angiotensin II for vasodilatory shockCritical Care201822Suppl 182
