Abstract
Despite advances in the diagnosis and management of asthma, uncontrolled disease is still associated with a substantial mortality and morbidity burden. Patients often overestimate their level of asthma control while also reporting that asthma symptoms affect their quality of life and ability to work or study. There is some evidence of success with primary prevention measures in high-risk children and the secondary prevention of asthma in sensitized individuals or those at risk of developing occupational asthma. There are challenges with diagnosis – with under- and overdiagnosis and misdiagnosis being common – and in the treatment of asthma, despite clear treatment guidelines. In particular, severe asthma presents a huge challenge to the clinician, and its complex and heterogeneous nature warrants a personalized medicine approach to match therapies to individual patients. However, the tools for this are currently lacking in primary care. This article reviews the current unmet need in the diagnosis and clinical management of asthma, and provides an overview of the limitations of current therapies.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
The global prevalence of clinical asthma has increased over the past 60 years, particularly in children,Citation1 with estimates of more than 300 million people of all ages affected worldwide.Citation2,Citation3 Although clinical advances in diagnosis and management have led to a reduction in the number of asthma-related deaths, there remains no cure and a substantial mortality burden still exists. Between 1990 and 2015, the age-standardized asthma-related death rate fell by 58.8%, with 397,000 deaths due to asthma in 2015.Citation4 The National Review of Asthma Deaths, a UK-wide investigation of asthma deaths occurring between 2012 and 2013, reported that >50% of deaths occurred in patients treated for mild or moderate asthma, and, importantly, factors that could have prevented deaths were identified in 46% of cases.Citation5
In addition to mortality, uncontrolled asthma is associated with substantial morbidity, despite the availability of effective treatments, and patients often overestimate their level of asthma control. For example, >80% of respondents to the Europe-wide Recognize Asthma and Link to Symptoms and Experience survey who had experienced acute exacerbations in the previous year considered their asthma to be controlled, despite only a fifth of respondents having Global Initiative for Asthma (GINA)-defined asthma control.Citation6 There is thus a need to improve the assessment of control from both a patient and physician perspective through education measures. Furthermore, among patients treated with an inhaled corticosteroid (ICS) and a long-acting β2-agonist (LABA), poor asthma control is associated with worse health-related quality of life compared with those with well-controlled asthma when considering mental and physical component scores and health utility.Citation7 Additionally, compared with well-controlled asthma, poorly controlled asthma is associated with increased loss of work productivity, including higher rates of presenteeism and overall work impairment.Citation7 In 2016, 24% of patients participating in Asthma UK’s Annual Asthma Survey reported that asthma symptoms affected their ability to work or study, with more than a quarter reporting at least 1 week off work or education as a result of their asthma in the previous year.Citation8
Scope
There have been several articles on unmet needs in asthma. These have been mainly secondary care-based,Citation9,Citation10 but some also consider the patient’s perspective.Citation11 This review aims to provide an up-to-date review of the literature, together with the author’s primary care perspective. Although this was not intended to be a systematic literature review, literature searches were conducted on PubMed from August to November 2017 using the keywords “asthma prevention”, “asthma diagnosis” and “asthma management”. Further relevant articles were obtained from the reference lists of reviewed articles. This review forms the first part of a thematic series, which reviews the use of anticholinergics in asthma.
Asthma prevention
Primary prevention of asthma
Asthma is a heterogeneous disease, and its development and persistence are associated with gene–environment interactions. Findings from intervention studies suggest that a “window of opportunity” may exist in early life, perhaps even in utero, during which targeted interventions can be used to minimize the risk of future asthma development. The aim of primary prevention measures is to prevent the onset of asthma in high-risk individuals, such as those with a family history of atopy or asthma, through the use of targeted interventions that minimize exposure to dietary, environmental, and/or pharmacologic allergens.Citation1,Citation12
A number of factors have been associated with an increased risk of developing asthma in young children who wheeze; however, evidence is mostly inconclusive. Positive associations with future asthma development have been reported for maternal factors during gestation (smoking, cesarean delivery, stress, high body mass index [BMI]), familial factors (genetics, family history of atopy), infections (respiratory syncytial virus, rhinovirus, pertussis), medication (paracetamol, β2-agonists, antibiotics), diet, and inhalation exposure (tobacco smoke, indoor and outdoor air pollution, house dust mite, mold).Citation1 Conversely, factors found to be negatively associated with the development of childhood asthma include agricultural subsistence, lifestyle, day care, diet, endotoxin, and farm animal exposure.Citation1
Primary prevention measures have investigated intervention and avoidance programs that focus on individual risk factors; however, these have generally yielded inconclusive results. Based on the heterogeneous nature of asthma development and the interplay of multiple environmental and genetic factors, another approach is to implement multifaceted prevention programs that target high-risk children during gestation and/or early life. A number of multifaceted programs have been trialed, with varying results. For example, the Canadian Asthma Primary Prevention Study aimed to minimize exposure to allergens (house dust mites and pet allergens) and environmental tobacco smoke, and encouraged breastfeeding during the first year of life. These measures successfully reduced the prevalence of pediatric allergist-diagnosed asthma and asthma symptoms among high-risk children up to 7 years of age by 56% compared with the control group.Citation13,Citation14 Similarly, the Isle of Wight Prevention Study was successful in reducing the development of allergic disease, including asthma, among high-risk children during the first 8 years of life by reducing exposure to food and house dust mite allergens in infancy.Citation15 A Cochrane review found that multifaceted rather than monofaceted intervention was preferable to usual care for the primary prevention of asthma in children aged <5 or ≥5 years; however, no significant differences were found between mono- and multifaceted interventions in reducing the frequency of asthma diagnosis in children aged <5 or ≥5 years or in reducing the likelihood of nocturnal coughing.Citation16 Despite the promising findings of these studies, other multifaceted prevention programs in primary care settings, such as the PREVASC study, have not been effective at reducing asthma symptoms in high-risk infants up to 2 years of age.Citation17 Selected primary prevention studies are detailed in .
Table 1 Selected mono- and multifaceted studies investigating primary and secondary prevention measures in asthma
It is possible that primary intervention programs have limited generalizability to other populations beyond those studied, who may have different lifestyles and are thus exposed to different risk factors. Additionally, the essential components of multifaceted programs remain unknown.Citation12 Nonetheless, there is compelling evidence to suggest that reducing exposure to multiple allergens reduces the likelihood of an asthma diagnosis in children versus usual care; however, further studies are warranted.
Secondary prevention of asthma
For sensitized individuals, secondary prevention measures aim to prevent the subsequent development of chronic and persistent disease, and include the avoidance of indoor and outdoor environmental pollution and allergens. For example, active and passive smoking in childhood and adolescence substantially increases the incidence of wheeze and the risk for new-onset asthma, particularly in nonallergic children and in those exposed in utero to maternal smoking.Citation18 Additionally, exposure to outdoor allergens in the form of environmental traffic-related air pollution during early and late childhood has been associated with a significant increase in the incidence of childhood asthma and allergic disease up to the age of 12 years.Citation19
Occupational asthma refers to new-onset asthma caused directly by exposure to substances in the workplace, and represents the most common work-related respiratory disease in industrialized countries.Citation20 Notably, it is estimated that ≥10% of cases of new or recurrent adult asthma are work-related, although the exact frequency is unknown.Citation20,Citation21 Although guidelines recommend that individuals with suspected occupational asthma be asked whether their symptoms improve when away from work, this approach may lack diagnostic accuracy. Therefore, the use of an objective test, such as a specific allergen challenge, is recommended.Citation21,Citation22 In cases of confirmed occupational asthma, further exposure should be prevented as early as possible to reduce the risk of developing established disease and to promote recovery.Citation20
In summary, interventions to improve primary and secondary prevention of asthma have been disappointing. However, research in this area remains a priority. In 2017, the European Asthma Research and Innovation Partnership project included the following statement in the top 15 research priorities in asthma: “Understand the increase in asthma (both childhood asthma and different types of asthma, such as allergic and hyper-responsive asthma) to help develop primary and secondary prevention strategies”.Citation23 It is hoped that further research in this area can help improve understanding of the risk factors associated with asthma development so that appropriate and successful prevention measures can be implemented in a timely manner.
Unmet needs in asthma diagnosis
A recent cross-sectional study found that patients diagnosed with asthma exhibit heterogeneous patterns of airway dysfunction, despite having similar symptom scores, highlighting the need for accurate asthma diagnosis before treatment initiation, particularly in primary care.Citation24 Currently, there is no single gold-standard diagnostic test for asthma, and guidelines recommend the use of an initial structured clinical assessment to determine the probability of asthma in individuals with respiratory symptoms, with consideration of a personal or family history of atopy.Citation21,Citation22 When asthma is suspected, objective tests are then recommended to assess pulmonary function and demonstrate airway obstruction; these include spirometry, bronchodilator reversibility, peak expiratory flow variability, assessment of airway inflammation, and airway hyperreactivity.Citation21,Citation22 Nevertheless, the tests have varying degrees of false positive and false negative values underlying the premise that there is no one gold standard test, and although positive findings on objective tests only indicate the probability of asthma, these tests are not being carried out, resulting in high rates of false-positive and false-negative findings.Citation22 Similarly, in patients with suspected asthma, outcomes of objective tests and the presence of respiratory symptoms may vary over time, reflecting the heterogeneous nature of the disease. Therefore, guidelines recommend that testing is repeated and compared in patients during symptomatic and asymptomatic periods.Citation22 The sensitivity and specificity of objective tests used in the diagnosis of asthma are summarized in .
Table 2 Sensitivity and specificity of objective tests in asthma diagnosis
The lack of a single well-defined gold-standard diagnostic measure for patients with suspected asthma means that both over- and underdiagnosis are common. For example, in one study, no evidence of asthma was found in a third of participants who had previously received a physician diagnosis of asthma upon serial assessment of symptoms, lung function, and airway reversibility.Citation25 In addition, undiagnosed asthma (defined as the presence of asthma-like symptoms with one or more obstructive airway abnormalities in the absence of physician-diagnosed asthma) was reported in a third of adolescents; underdiagnosis was independently associated with self-reported family problems, daily exposure to indoor tobacco smoke, low physical activity, high BMI and the absence of serial sneezing.Citation26 It is likely that the problem of asthma underdiagnosis also reflects the underrepresentation of respiratory symptoms to primary care physicians, despite the presence of decreased lung function in some individuals.Citation27
The overdiagnosis of asthma may in part explain the increasing prevalence of asthma observed in recent years, whereas its underdiagnosis and subsequent undertreatment may be reflected in the reported morbidity and mortality associated with asthma. In the Netherlands, an asthma diagnostic consultancy service was established with the aim of assisting general practitioners in their diagnostic process. Subsequently, an asthma diagnosis was excluded in approximately half the patients referred to this service, and a change in maintenance therapy was recommended in three-quarters.Citation28
In addition to the under- and overdiagnosis of asthma, misdiagnosis is also common, and has implications for the correct management of patients diagnosed with asthma who may have another respiratory condition that is neither appropriately investigated nor treated. Young children commonly present with sporadic respiratory symptoms; however, diagnosing asthma in children aged <5 years is challenging, as the routine assessment of airflow limitation is not possible in young children.Citation21 For example, recurrent viral wheeze is common among this population, and usually occurs in combination with an upper respiratory tract infection. However, a diagnosis of asthma based on the initial presentation of wheeze is difficult.Citation12 In this population, “trial by treatment” is the diagnostic approach commonly used, with reviews recommended every 2–3 months to assess response to controller treatment and temporal patterns of symptoms. In addition, a diagnosis of asthma in young children should consider any family history of atopy.Citation12 GINA recommend that symptoms be treated based upon the physician’s clinical judgment and objective tests performed once the child reaches an appropriate age.Citation12
Despite advances in the understanding of asthma pathophysiology and an increased awareness of patient risk factors, there is still a need for improved diagnostic measures and procedures. Therefore, asthma diagnosis should be considered a key unmet need, as improvements in this area will ensure timely and accurate diagnosis of patients with suspected asthma, and allow them subsequently to receive appropriate management.
Unmet needs in asthma management
According to GINA recommendations, the long-term aims of asthma management in patients of all ages are to achieve control of asthma symptoms and to reduce the risk of future exacerbations and fixed airflow limitation.Citation12,Citation22 In control-based asthma management, which involves a continuous cycle of assessment, treatment adjustment, and review, both symptoms and future exacerbation risk should be considered when initiating therapy and establishing a management plan.Citation12 However, even with the availability of different treatment options and guidelines to aid clinical decision-making, a high proportion of patients with asthma fail to obtain guideline-defined control and remain symptomatic.Citation29
Poor asthma control can arise through a combination of patient and physician factors. Patient factors associated with poor asthma control include poor adherence to treatment, poor perception, lower annual household income, previous exacerbation or emergency room visit, psychoemotional factors, and poor inhaler technique, including errors and comorbidities (rhinitis, obesity, depression).Citation5,Citation7,Citation30 In the UK, almost two-thirds of individuals who pay for their asthma medication stated that this impacted their finances, with the highest impact on patients in northeast England.Citation8
A review of local, national, and multinational survey data revealed inadequate patient education in terms of both their underlying disease and its treatment, underreporting of symptoms, and a mismatch between patient perception of their asthma control and symptoms. Importantly, patients often tolerated poor asthma control and underreported symptoms, with direct implications on disease classification and management.Citation29–Citation31 For example, >65% of patients questioned in the Asthma UK survey reported symptoms in the previous week, although >80% considered their asthma to be “controlled”, highlighting the disconnection between the patients’ perception of their disease and its control.Citation32 Similarly, in the Asthma Insights and Reality in Europe study, only 5.3% of participants achieved the goals set forth in the GINA recommendations.Citation29 Furthermore, in Asthma UK’s 2016 Annual Asthma Survey, 82% of participants reported having poorly controlled asthma, which affected the everyday life of more than half the patients.Citation8
The Global Asthma Physician and Patient (GAPP) survey aimed to identify differences in opinions on the management of asthma between patients and physicians, and identified a direct link between patient–physician communication and treatment compliance.Citation11 Notably, there was a mismatch between the perception of education provision, with 87% of physicians stating that up to 50% of the time spent in office visits was devoted to education, compared with 64% of patients who, on average, stated that only 25% of the appointment was spent discussing educational issues.Citation11 Similarly, there was a mismatch in the perception of compliance, with patients overstating their level of treatment compliance compared with that reported by the physician.Citation11 There was a direct association between better patient–physician communication and greater patient-reported compliance.
Physician factors associated with poor asthma control include noncompliance with guidelines, lack of action plans, and no/poor assessment of asthma control. Basic asthma care includes an annual asthma review, an action plan, and an assessment of inhaler technique; however, only a third of patients surveyed received these three aspects of care.Citation8,Citation22 Notably, 42% of patients received an asthma action plan in 2016, compared with 24% in 2013; therefore, although this figure almost doubled between 2013 and 2016, more than half the patients surveyed did not have an asthma action plan, despite more than three-quarters (78%) attending an annual asthma review.Citation8 In the INSPIRE study, only 28% of participants had well-controlled asthma (defined by Asthma Control Questionnaire [ACQ] score), despite 70% receiving treatment with an ICS with or without a LABA. Consistently with previous reports, there was a disconnect between patient-reported and ACQ-defined asthma control.Citation31
In summary, there is encouraging evidence that asthma management can be improved by measures to enhance physician and patient education on supported self-management and developing better inhaler techniques. A detailed review of inhaler devices is covered by Dr Omar Usmani (Imperial College London) elsewhere in this thematic review series.
Unmet needs in the treatment of asthma
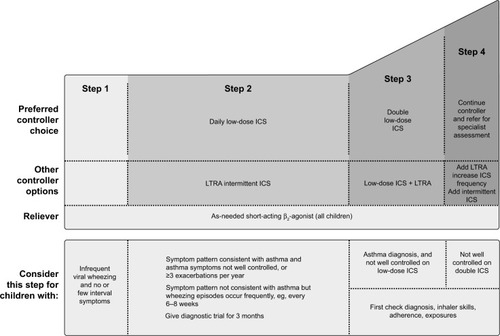
According to GINA recommendations, asthma treatment decisions should be based on assessing and adjusting treatment, as well as reviewing the treatment response.Citation12 Before stepping up treatment, the following should be considered: is the diagnosis of asthma correct? Are there any other significant comorbidities contributing to the worsening of symptoms? Is there compliance with the existing medication? Is the inhaler technique correct? Are there any other confounding factors, such as smoking or exposure to asthma triggers, at work?Citation12 The treatment can then be adjusted up or down in a stepwise approach, as shown in and . However, ineffective asthma treatment, such as inappropriate use of therapy, remains and can thus be considered a primary unmet need.
Figure 1 Stepwise asthma management in adults, adolescents, and children aged 6–11 years.
Abbreviations: ICS, inhaled corticosteroid; BDP, beclomethasone dipropionate; BUD, budesonide; LABA, long-acting β2-agonist; LTRA, leukotriene receptor antagonist; SABA, short-acting β2-agonist.
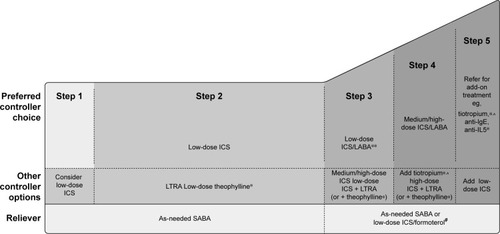
Figure 2 Stepwise asthma management in children aged ≤5 years.
Abbreviations: ICS, inhaled corticosteroid; LTRA, leukotriene-receptor antagonist.
Inhaled corticosteroids
Both physicians and patients believe there is a need for new medication options for the treatment of asthma.Citation11 A key element of asthma pathophysiology is airway inflammation. First-line asthma controller treatment with a low-dose ICS targets eosinophilic airway inflammation and is recommended early in the disease course to reduce the risk of future exacer-bations.Citation12 However, despite high agreement among physicians that ICS represents the gold standard for asthma treatment, the results of the GAPP survey reported an underuse in first-line ICS for asthma patients. Notably, first-line treatment for asthma is not prescribed in accordance with GINA recommendations, with physicians often prescribing a LABA only, despite the lack of efficacy of this drug class on airway inflammation.Citation11 Canonica et al concluded that the underuse of ICSs may be explained by physician dissatisfaction with this drug class and lack of adherence to treatment guidelines.Citation11
However, in the 3-year Inhaled Steroid Treatment as Regular Therapy in Early Asthma (START) study, early intervention with low-dose ICS (budesonide 200 or 400 μg/ daily) in children and adults with recent-onset mild persistent asthma reduced the risk of a severe asthma exacerbation versus placebo by 44%.Citation33 Importantly, ICS treatment was safe and well tolerated, with no unexpected unfavorable adverse events reported.Citation34 Although guidelines recommend the addition of a LABA to first-line ICS in asthma patients who remain symptomatic (), uncertainty exists regarding the optimal dose of ICS.Citation35 The dose–response relationship of fluticasone propionate in terms of improvement of symptoms and lung function begins to plateau at around 100–200 μg/day, with maximum efficacy achieved with doses of approximately 500 μg/day in adults and adolescents for lung function and symptom control, although data on the use of this dose in patients with asthma are limited.Citation36 Consistently with this, a meta-analysis has shown that if add-on therapy is warranted in patients with asthma who remain symptomatic despite the use of ICS, the addition of a LABA to moderate-dose ICS (approximately 200 μg/day fluticasone or equivalent) confers greater clinical benefit than doubling the dose of ICS.Citation35
In most patients with asthma, symptoms can be controlled by low-dose ICSs; however, some patients require high doses or oral steroids (steroid-insensitive asthma), while others are completely resistant to the effects of steroids regardless of dose (steroid-resistant asthma).Citation37 Additionally, patients with more severe asthma are less responsive to ICS than those with mild asthma. ICS resistance can occur through exposure to risk factors, such as smoking,Citation38 or through genotype effects. Evidence suggests that familial steroid resistance is linked to abnormalities in the glucocorticoid receptor (GR), including reduced GR-binding affinity, reduced nuclear translocation, and decreased GR expression in peripheral blood mononuclear cells.Citation37,Citation39 Additionally, abnormal histone acetylation and transcription factor activation may be mechanisms of steroid resistance in patients with asthma.Citation37 Additional studies on peripheral blood mononuclear cells isolated from steroid-resistant individuals have demonstrated that corticosteroids fail to inhibit the secretion of interleukin-2 (IL2) and interferon-γ (IFNγ) in these patients.Citation37 Therefore, steroid resistance represents an area of unmet need in asthma management, particularly in severe asthma, and additional therapies are required that target the underlying airway inflammation. Interestingly, there is some evidence to suggest that LABAs promote GR nuclear translocation and increase sensitivity to corticosteroids, and may thus enhance the function of glucocorticoids and assist in restoring their function in steroid-insensitive/resistant patients.Citation37,Citation40,Citation41
β2-Agonists
Since β2-agonists do not target airway inflammation in asthma, patients should only be treated with a β2-agonist alone in exceptional circumstances, including in those with mild intermittent asthma and infrequent symptoms.Citation12 Although LABAs in the absence of an ICS may be effective at reducing asthma symptoms, evidence from meta-analyses suggests that they may increase the risk of adverse outcomes in adult patients, including severe exacerbations and death.Citation42 Therefore, an as-needed short-acting β2-agonist is recommended as reliever therapy in GINA step 1 ( and ),Citation12 rather than regular use of a LABA. Patients have reported that suboptimal asthma control substantially affected their health-related quality of life, despite receiving maintenance treatment with an ICS with or without a LABA.Citation31 Therefore, such patients may benefit from additional bronchodilation, such as that provided by an anticholinergic (also known as a long-acting muscarinic antagonist).
Leukotriene receptor antagonists
Leukotriene receptor antagonists, such as montelukast, may be effective in some patient populations, including those with exercise-induced asthma, virus-induced wheeze, and asthma associated with allergic rhinitis.Citation43 However, no routine laboratory tests are currently available to predict leukotriene-receptor-antagonist responsiveness in individual patients.
Challenges of severe asthma
Severe asthma is defined by GINA as asthma that requires step 4 or 5 treatment to maintain symptom control (), and may present similarly to asthma that is poorly controlled due to lack of treatment.Citation12 Although severe asthma only affects 5%–10% of the asthma population,Citation44 it is responsible for a high proportion of total asthma-related deaths (39% in the recent National Review of Asthma Deaths survey).Citation5 Many patients with severe asthma are treated with oral corticosteroids, although these are associated with side effects in the majority of patients, as well as poor adherence and reduced quality of life.Citation45 Therefore, there is a need for effective treatments in this population of patients, and urgent solutions are required. A major unmet need in severe asthma is the development of therapies that match the individual phenotype of the patient. Biological therapies, such as omalizumab and mepolizumab, are now available for a more targeted approach to therapy.Citation46 However, in the absence of patient phenotyping, treatment options with efficacy over the range of asthma severities, including patients with severe asthma, are needed.
Limitations of current asthma therapies
Randomized clinical trials analyze group mean data; however, asthma is a heterogeneous disease, and different phenotypes (observable features) and endotypes (molecular mechanisms of pathogenesis) exist that may respond differently to therapy.Citation47 Additionally, real-world populations include both responders and nonresponders. Current diagnostic labels, including those for airway disease, are based on an outdated understanding of physiological mechanisms, and do not consider the heterogeneity of the disease, which may lead to suboptimal management.Citation48
The complex and heterogeneous nature of asthma warrants a precision medicine approach. Agusti et alCitation48 introduced the concept of “treatable traits” as a label-free precision-medicine strategy for chronic airway diseases, such as asthma and chronic obstructive pulmonary disease. Within the adult population, treatable traits are based upon phenotypes or an understanding of the underlying endotype, and include airflow limitation, which may be treated with a LABA and/or long-acting anticholinergic, and eosinophil airway inflammation, for which an ICS is recommended.Citation48 While this approach is certainly attractive, the tools required for precision medicine are currently lacking in clinical practice, especially in primary care. Additionally, the definitions proposed by Agusti et alCitation48 exclude children, who represent a large population of patients in need of improved diagnostic measures and treatment options. Until such time as the tools for precision medicine become universally available and pediatric patients are considered, there remains a need for asthma therapy with proven efficacy and safety over the range of disease severities and patients. Recently, the efficacy of tiotropium, a long-acting anticholinergic approved for the treatment of symptomatic patients at risk of exacerbation despite treatment with an ICS plus a LABA, was demonstrated to be independent of baseline characteristics and allergic status in patients with asthma.Citation49 This suggests that an anticholinergic such as tiotropium may be appropriate for targeting a broad population of patients. The evidence for the role of anticholinergics in adults, children, and preschool children is covered by several review articles in this series, and is thus not included here.
Conclusion
Asthma remains a disease with significant morbidity and preventable mortality. outlines the key areas of unmet need. Despite increased recognition of environmental and genetic factors, which are linked to the development of asthma, there is limited evidence of successful primary prevention measures. Similarly, there is a huge unmet need in reducing factors known to aggravate established asthma, such as vehicle pollution and tobacco smoke. Evidence for successful intervention has been variable to date. Under-and overdiagnosis of asthma is common, and there is a need for accurate objective tests that can be used widely in primary care, in addition to quality-assured implementation of guideline-recommended diagnostic procedures.
Figure 3 Key areas of unmet need in asthma.
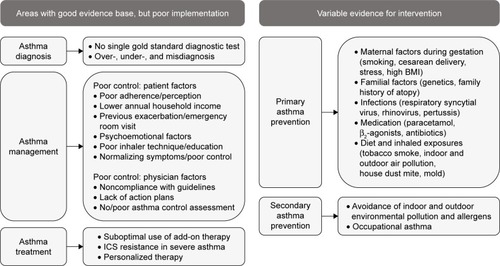
ICS therapy remains the cornerstone of asthma management, but compliance is still poor. Potential solutions include improved patient education/self-management and use of integral inhaler device monitors, which may improve outcomes. However, asthma is a heterogeneous disease, and there is a need to target treatment to the individual patient. Therefore, it may be beneficial to adopt the precision medicine approach, particularly given that the use of targeted biological therapy in patients with severe asthma is indeed progressing rapidly. Nevertheless, for the majority of patients with asthma, many of whom are treated in primary care, this approach is far from being established. Therefore, there is an important role for such agents as long-acting anticholinergics, which are effective across a broad spectrum of severity and age groups.
Acknowledgments
The author would like to thank Kjeld Hansen, a member of the Patient Ambassador Group for the European Lung Foundation, for his input to the video summary for this manuscript. Medical writing assistance in the form of the preparation and revision of the draft manuscript was supported financially by Boehringer Ingelheim and provided by Lisa Jolly, PhD, of MediTech Media, under the author’s conceptual direction and based on feedback from the author. Boehringer Ingelheim was given the opportunity to review the manuscript for factual accuracy only. The author takes full responsibility for the scope, direction, content, and editorial decisions relating to the manuscript, was involved at all stages of development, and has approved the submitted manuscript.
Disclosure
As a general practitioner, the author has provided a primary care perspective on the review topic. The author has acted as a medical consultant and spoken on behalf of Astra-Zeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Mundipharma/Napp, Nutricia, Pfizer, and Teva. The author reports no other conflicts of interest in this work.
References
- BeasleyRSempriniAMitchellEARisk factors for asthma: is prevention possible?Lancet201538699981075108526382999
- Global Burden of Disease 2016 Disease and Injury Incidence and Prevalence CollaboratorsGlobal, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016Lancet20173901211125928919117
- BousquetJKhaltaevNGlobal surveillance, prevention and control of chronic respiratory diseases: a comprehensive approachGenevaWorld Health Organization2007
- GBD 2013 Mortality and Causes of Death CollaboratorsGlobal, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease study 2013Lancet2015385996311717125530442
- Royal College of PhysiciansWhy Asthma Still Kills: The National Review of Asthma Deaths (NRAD)LondonRCP2014
- PriceDFletcherMvan der MolenTAsthma control and management in 8,000 European patients: the Recognise Asthma and Link to Symptoms and Experience (REALISE) surveyNPJ Prim Care Respir Med2014241400924921985
- PavordIDMathiesonNScowcroftAPedersiniRIsherwoodGPriceDThe impact of poor asthma control among asthma patients treated with inhaled corticosteroids plus long-acting β2-agonists in the United Kingdom: a cross-sectional analysisNPJ Prim Care Respir Med20172711728270657
- Asthma UKAnnual asthma survey: 2016 report2016 Available from: https://www.asthma.org.uk/globalassets/get-involved/external-affairs-campaigns/publications/annual-asthma-care-survey/annualasthmasur-vey2016final.pdfAccessed November 01, 2017
- ScalPDavernMIrelandMParkKTransition to adulthood: delays and unmet needs among adolescents and young adults with asthmaJ Pediatr20081524471.e1475.e118346498
- WorstellMAsthma: individual patient perspective and current unmet needsClin Exp Allergy200030Suppl 1111510849468
- CanonicaGWBaena-CagnaniCEBlaissMSDahlRKalinerMAValovirtaEJUnmet needs in asthma: Global Asthma Physician and Patient (GAPP) survey: global adult findingsAllergy200762666867417508972
- Global Initiative for AsthmaGlobal strategy for asthma management and prevention2018 Available from: http://ginasthma.org/2018-gina-report-global-strategy-for-asthma-management-and-prevention/Accessed May 21, 2018
- Chan-YeungMFergusonAWatsonWThe Canadian Childhood Asthma Primary Prevention study: outcomes at 7 years of ageJ Allergy Clin Immunol20051161495515990772
- BeckerAWatsonWFergusonADimich-WardHChan-YeungMThe Canadian Asthma Primary Prevention study: outcomes at 2 years of ageJ Allergy Clin Immunol2004113465065615100668
- ArshadSHBatemanBSadeghnejadAGantCMatthewsSMPrevention of allergic disease during childhood by allergen avoidance: the Isle of Wight prevention studyJ Allergy Clin Immunol2007119230731317291851
- MaasTKaperJSheikhAMono and multifaceted inhalant and/or food allergen reduction interventions for preventing asthma in children at high risk of developing asthmaCochrane Database Syst Rev20093CD006480
- SchönbergerHJDompelingEKnottnerusJAThe PREVASC study: the clinical effect of a multifaceted educational intervention to prevent childhood asthmaEur Respir J200525466067015802340
- GillilandFDIslamTBerhaneKRegular smoking and asthma incidence in adolescentsAm J Respir Crit Care Med2006174101094110016973983
- BowatteGLodgeCLoweAJThe influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: a systematic review and a meta-analysis of birth cohort studiesAllergy201570324525625495759
- NicholsonPJCullinanPTaylorAJBurgePSBoyleCEvidence based guidelines for the prevention, identification, and management of occupational asthmaOccup Environ Med200562529029915837849
- National Institute for Health and Care ExcellenceAsthma: Diagnosis and Monitoring of Asthma in Adults, Children and Young PeopleLondonNICE2017
- British Thoracic Society (BTS)/Scottish Intercollegiate Guidelines Network (SIGN)British Guideline on the management of asthmaEdinburghSIGN2016QRG 153 [cited November 2017] Available from: http://www.sign.ac.ukAccessed November 01, 2017
- MasefieldSEdwardsJHansenKThe future of asthma research and development: a roadmap from the European Asthma Research and Innovation Partnership (EARIP)Eur Respir J2017495160229528461297
- ShawDGreenRBerryMA cross-sectional study of patterns of airway dysfunction, symptoms and morbidity in primary care asthmaPrim Care Respir J201221328328722786814
- AaronSDVandemheenKLBouletLPOverdiagnosis of asthma in obese and nonobese adultsCMAJ2008179111121113119015563
- SierstedHCBoldsenJHansenHSMostgaardGHyldebrandtNPopulation based study of risk factors for underdiagnosis of asthma in adolescence: Odense schoolchild studyBMJ199831671326516579522784
- van SchayckCPvan der HeijdenFMvan den BoomGTirimannaPRvan HerwaardenCLUnderdiagnosis of asthma: is the doctor or the patient to blame? The DIMCA projectThorax200055756256510856315
- GillisRMvan LitsenburgWvan BalkomRHMurisJWSmeenkFWThe contribution of an asthma diagnostic consultation service in obtaining an accurate asthma diagnosis for primary care patients: results of a real-life studyNPJ Prim Care Respir Med20172713528526889
- RabeKFVermeirePASorianoJBMaierWCClinical management of asthma in 1999: the Asthma Insights and Reality in Europe (AIRE) studyEur Respir J200016580280711153575
- HolgateSTPriceDValovirtaEAsthma out of control? A structured review of recent patient surveysBMC Pulm Med20066Suppl 1S217140420
- PartridgeMRvan der MolenTMyrsethSEBusseWWAttitudes and actions of asthma patients on regular maintenance therapy: the INSPIRE studyBMC Pulm Med200661316772035
- HylandMEStåhlEAsthma treatment needs: a comparison of patients’ and health care professionals’ perceptionsClin Ther200426122141215215823778
- PauwelsRAPedersenSBusseWWEarly intervention with budesonide in mild persistent asthma: a randomised, double-blind trialLancet200336193631071107612672309
- ShefferALSilvermanMWoolcockAJDiazPVLindbergBLindmarkBLong-term safety of once-daily budesonide in patients with early-onset mild persistent asthma: results of the Inhaled Steroid Treatment as Regular Therapy in Early Asthma (START) studyAnn Allergy Asthma Immunol2005941485415702816
- MasoliMWeatherallMHoltSBeasleyRSystematic review of the dose-response relation of inhaled fluticasone propionateArch Dis Child2004891090290715383431
- HoltSSuderAWeatherallMChengSShirtcliffePBeasleyRDose-response relation of inhaled fluticasone propionate in adolescents and adults with asthma: meta-analysisBMJ2001323730725325611485952
- BarnesPJCorticosteroid resistance in patients with asthma and chronic obstructive pulmonary diseaseJ Allergy Clin Immunol2013131363664523360759
- ChalmersGWMacleodKJLittleSAThomsonLJMcSharryCPThomsonNCInfluence of cigarette smoking on inhaled corticosteroid treatment in mild asthmaThorax200257322623011867826
- SherERLeungDYSursWSteroid-resistant asthma: cellular mechanisms contributing to inadequate response to glucocorticoid therapyJ Clin Invest199493133398282803
- UsmaniOSItoKManeechotesuwanKGlucocorticoid receptor nuclear translocation in airway cells after inhaled combination therapyAm J Respir Crit Care Med2005172670471215860753
- KobayashiYMercadoNMiller-LarssonABarnesPJItoKIncreased corticosteroid sensitivity by a long acting β2 agonist formoterol via β2 adrenoceptor independent protein phosphatase 2A activationPulm Pharmacol Ther201225320120722401993
- SalpeterSRBuckleyNSOrmistonTMSalpeterEEMeta-analysis: effect of long-acting β-agonists on severe asthma exacerbations and asthma-related deathsAnn Intern Med20061441290491216754916
- MarcelloCCarloLAsthma phenotypes: the intriguing selective intervention with montelukastAsthma Res Pract201621127965779
- BusseWWBanks-SchlegelSWenzelSEPathophysiology of severe asthmaJ Allergy Clin Immunol200010661033104211112883
- Asthma UKSevere asthma: the unmet need and the global challenge2017 Available from: https://www.asthma.org.uk/globalassets/get-involved/external-affairs-campaigns/publications/severe-asthma-report/auk_severeasthma_2017.pdfAccessed November 01, 2017
- MenzellaFGaleoneCBertoliniFCastagnettiCFacciolongoNInnovative treatments for severe refractory asthma: how to choose the right option for the right patient?J Asthma Allergy20171023724728919788
- LötvallJAkdisCABacharierLBAsthma endotypes: a new approach to classification of disease entities within the asthma syndromeJ Allergy Clin Immunol2011127235536021281866
- AgustiABelEThomasMTreatable traits: toward precision medicine of chronic airway diseasesEur Respir J201647241041926828055
- KerstjensHAMoroni-ZentgrafPTashkinDPTiotropium improves lung function, exacerbation rate, and asthma control, independent of baseline characteristics including age, degree of airway obstruction, and allergic statusRespir Med201611719820627492532
- International Standard Randomised Controlled Trial NumberManchester Asthma and Allergy study: primary prevention of asthma and allergy by allergen avoidance in high risk infants2005 Available from: http://www.isrctn.com/ISRCTN63558189Accessed November 01, 2017
- CustovicASimpsonBMSimpsonAKissenPWoodcockAEffect of environmental manipulation in pregnancy and early life on respiratory symptoms and atopy during first year of life: a randomised trialLancet2001358927718819311476835
- WoodcockALoweLAMurrayCSEarly life environmental control: effect on symptoms, sensitization, and lung function at age 3 yearsAm J Respir Crit Care Med2004170443343915142868
- Prevention and Incidence of Asthma and Mite AllergyThe PIAMA research project Available from: http://piama.iras.uu.nl/index-en.phpAccessed November 01, 2017
- CorverKKerkhofMBrusseeJEHouse dust mite allergen reduction and allergy at 4 yr: follow up of the PIAMA studyPediatr Allergy Immunol200617532933616846450
- HalmerbauerGGartnerCSchierlMStudy on the Prevention of Allergy in Children in Europe (SPACE): allergic sensitization at 1 year of age in a controlled trial of allergen avoidance from birthPediatr Allergy Immunol2003141101712603706
- HorakFJrMatthewsSIhorstGEffect of mite-impermeable mattress encasings and an educational package on the development of allergies in a multinational randomized, controlled birth-cohort study: 24 months results of the Study of Prevention of Allergy in Children in EuropeClin Exp Allergy20043481220122515298561
- ArshadSHBojarskasJTsitouraSPrevention of sensitization to house dust mite by allergen avoidance in school age children: a randomized controlled studyClin Exp Allergy200232684384912047429
- ZeigerRSHellerSThe development and prediction of atopy in high-risk children: follow-up at age seven years in a prospective randomized study of combined maternal and infant food allergen avoidanceJ Allergy Clin Immunol1995956117911907797786
- RamseyCChanEChooniedassRThe Canadian Asthma Primary Prevention Study (CAPPS): outcomes at 15 years of ageAm J Resp Crit Care Med2013181A3520
- ArshadSHBatemanBSadeghnejadAGantCMatthewsSMPrevention of allergic disease during childhood by allergen avoidance: the Isle of Wight prevention studyJ Allergy Clin Immunol2007119230731317291851
- GuilbertTWMorganWJZeigerRSLong-term inhaled corticosteroids in preschool children at high risk for asthmaN Engl J Med2006354191985199716687711
- MurrayCSWoodcockALangleySJMorrisJCustovicASecondary prevention of asthma by the use of Inhaled Fluticasone propionate in Wheezy Infants (IFWIN): double-blind, randomised, controlled studyLancet2006368953775476216935686
- JacobsenLNiggemannBDreborgSSpecific immunotherapy has long-term preventive effect of seasonal and perennial asthma: 10-year follow-up on the PAT studyAllergy200762894394817620073
- National Institute for Health and Care ExcellenceAsthma: Diagnosis, Monitoring and Chronic Asthma ManagementLondonNICE2017
