Abstract
Introduction
The third report of the National Cholesterol Education Program guidelines recommends calculating the 10-year morbidity of atherosclerotic cardiovascular disease (ASCVD) using risk calculators when treating high blood cholesterol in adults. We analyzed the changes in cardiovascular risk (CVR) among Mexican patients with HIV.
Patients and methods
This observational, prospective cohort study compared the CVR after 1 year of antiretroviral treatment among 460 HIV patients from a Mexican clinic. Changes using the ASCVD risk estimator and changes in clinical outcomes were analyzed. The results were categorized as low or high CVR using a cutoff of 7.5%.
Results
The CVR initially had a median of 2.3% (interquartile range [IQR]: 1%–4.8%), which changed to 2.4% (IQR: 1.5%–5.5%) after 1 year (P=0.001). After CVR stratification, we found that 84.3% of the patients had a low CVR, and 18% in this subgroup had metabolic syndrome (MS). Moreover, 15.7% had high CVR, and 47% in this subgroup had MS. The 4.3% of patients had an increase in CVR from the low to high subgroup, and 2.6% had a decrease in CVR from the high to low subgroup. Out of all patients, 22.3% had MS.
Conclusion
More than 50% of the population had an increase in CVR after 1 year. Of these patients, 4.3% changed from the low to high CVR group. Although the guidelines proposed different time periods for performing CVR estimations, this study showed that such assessments offered valuable clinical data over a relatively short-term period.
Introduction
Because of the success of easier, less toxic, more effective, highly active antiretroviral therapies (HAARTs), the mortality of people living with HIV (PLWH) and AIDS has declined.Citation1,Citation2 The factors that contribute to increased cardiovascular risk (CVR) in PLWH are complex because of inflammatory pathway activation and comorbidi-ties that are associated with risk behaviors and lifestyle habits.Citation3 It is well known that HAARTs can induce metabolic abnormalities and increase toxicity markers such as serum cholesterol, triglycerides, and hepatic enzymes.Citation4,Citation5 Underlying HIV infection per se might also result in an increased risk of CVR.Citation6 Increases in lipid levels promote lipoatrophy development, lipo-accumulation, and insulin resistance with consequent hyperglycemia and hyperlipidemia.Citation6–Citation8 Chronic inflammatory processes in PLWH resulting from an imbalance in immune/inflammatory responses can increase the levels of systemic pro-inflammatory markers and adiponectin.Citation9
Previous studies suggested that cardiovascular disease (CVD) is approximately 1.5- to 2-fold higher in PLWH vs noninfected people.Citation10,Citation11 However, the specific CVR factors that result from the metabolic effects of HIV infection and its therapies suggest that useful approaches exist to screen for CVD in PLWH.Citation10
National and international guidelines propose that multivariate risk tools such as the Framingham equations should be incorporated into CVR assessment.Citation12–Citation16 In Mexico, CVR evaluation is recommended each year,Citation12 whereas Spain recommends evaluation every 2 years.Citation13 Studies in the US have used the Framingham assessment guidelines to address CVR management.Citation13 CVR evaluation in Mexican patients has not been documented to date. Nevertheless, studies have reported an increase in cardiovascular events in the United States.Citation14 Evidence from prospective, observational, and surrogate end point studies suggests that HAARTs are associated with an increased risk of cardiovascular events and are related in part to dyslipidemia. The American College of Cardiology/American Heart Association (ACC/AHA) clinical guidelinesCitation15 emphasize CVR assessment for two reasons: 1) to address modifiable risk factors for reducing CVR in patients and 2) to demonstrate CVD risk reduction benefits. Both of these factors help determine whether a patient is at high risk and identify how to address any CVR factors present.Citation14,Citation16 CVD risk reduction must be one of the primary goals of medical care; for that reason, this study sought to analyze the changes in the CVR and clinical outcomes of PLWH attending a specialized clinic over a 1-year period.
Patients and methods
Design
An observational and prospective cohort study was conducted to compare CVR among PLWH and clinical outcomes after 1 year of HAART (which is defined as a combination of three or more antiretroviral drugs to inhibit the replication of HIV) at a specialized clinic. The study was approved by the National Ethics Committee on Health Research and the Bio-security Committee, which both belong to the Mexican Institute of Social Security (IMSS; number: F-CNCI-2015–156). Therefore, the study was performed according to the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Written informed consent for publication was obtained from all the authors and participants.
Study participants
The sample consisted of registered outpatients from the Retrovirus Clinic of the Regional General Hospital Number 1 of the IMSS in Morelos, Mexico. Patients aged ≥18 years with complete clinical records were eligible for study inclusion.
Data collection
All patients’ clinical records in February 2015 were analyzed; a second data analysis was conducted in February 2016. Each patient had a monthly medical appointment at the Retrovirus Clinic, in which anthropometric and blood pressure (BP) measurements were taken by a nurse. The physician specialist obtained a complete medical interview, physical examination, and laboratory findings from each patient. The patients received their monthly medication based on Mexican guidelines.Citation12 Other services such as social care and psychology were provided.
Initially, the following information was manually collected: 1) HIV/AIDS diagnosis date; 2) history of CVD (myocardial infarction [MI], stroke, or an intervention for coronary artery disease), type 2 diabetes mellitus (T2DM), and hypertension diagnosis date; 3) cigarette smoking status; 4) HAART regimen; and 5) hypoglycemic, antihypertensive, and lipid-lowering medication use.
Study variables
The outcome variables evaluated in this study included CVR assessment, clinical measures (systolic and diastolic BP, waist circumference, weight, and height), laboratory values (fasting glucose [FG], total cholesterol [TC], and high-density lipoprotein cholesterol [HDL-C]), triglycerides, CD4+ cell count, and metabolic syndrome (MS) profile. CVR calculation was performed using the atherosclerotic CVD (ASCVD) risk estimator recommended by the ACC/AHA clinical guidelinesCitation15 to quantify the estimated 10-year absolute ASCVD risk at and after a 1-year period. The ASCVD estimator is based on a parametric statistical model controlling for multiple CVD risk factors including age, gender, race, TC, HDL-C, systolic BP, hypertension treatment, T2DM status, and smoking history. A CVR value of 7.5% was considered as the cutoff point for this study, because this percentage is used by the ACC/AHACitation15 as a reference point for establishing the intensity of lipid-lowering therapy. When the CVR is ≥7.5%, the use of moderate-to-high statin therapy should be considered; when the CVR is <7.5%, a low-to-moderate intensity statin can be considered. In this study, <7.5% values were considered as “low CVR”, and the ≥7.5% values were considered as “high CVR”.
The MS profile was defined as the presence of three or more of the following National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATP III) criteria:Citation17 1) waist circumference >88 cm in women or >102 cm in men; 2) BP ≥130 mmHg systolic or ≥85 mmHg diastolic or use of antihypertensive medications; 3) triglycerides ≥150 mg/dL or use of lipid-lowering medications; 4) serum FG ≥100 mg/dL, physician-diagnosed diabetes or use of diabetic medications; 5) HDL-C <50 mg/dL in women or <40 mg/dL in men. These criteria reference values were used to compare the initial and 1-year period data as defined by the NCEP-ATP III criteria.Citation17
Statistical analyses
Categorical variables were expressed as frequencies and percentages. The Pearson’s chi-squared and Fisher’s exact tests were used to calculate 95% CI for categorical variables. Non-normal distributed continuous variables were expressed as medians and interquartile ranges (IQRs), and differences were determined using Wilcoxon signed-rank test with a 5% error. All statistical analyses were performed using Minitab version 17 for Windows (Statistical software, State College, PA, USA).
Results
The sample consisted of 460 patients: 79.3% were men and 20.7% were women. The median age of the sample was 43 years (IQR: 34–52 years); women (46 years) were older than men (42 years) on average (P<0.001). Ninety-one (19.7%) patients were current smokers, 71 (15.4%) patients received antihypertensive treatment, 35 (7.6%) patients received T2DM treatment, and 219 (47.5%) patients received lipid-lowering treatment. We found MS and CVD event rates of 22.3% and 2.6%, respectively. The HAARTs applied in the current sample had a median duration of 6 years (IQR: 3–14 years); nucleoside reverse transcriptase inhibitor (NRTI) plus protease inhibitor (PI) was the most common therapy ().
Table 1 Description of the characteristics among PLWH stratified by CVR at baseline
The overall median CVR at baseline was 2.3% (IQR: 1%–4.8%), with a range of 0.2%–50.1%; after 1 year, the median was 2.4% (IQR: 1.1%–5.5%), with a range of 0.2%–33.2% (P=0.001). At the beginning, the patients with low CVR comprised 84.3% of the sample, and the group with high CVR comprised 15.7%. Patients with low CVR had a higher proportion of one or two MS risk factors and a higher MS percentage (18%) compared with the high CVR patient group (P<0.001). Lipid-lowering treatment was found in similar proportions between the low and high CVR groups.
After 1 year, we found that the low CVR group showed a CVR increase from 2.3% to 2.7% (P<0.001), and the high CVR group showed a CVR decrease from 16% to 14.2% (P<0.001).
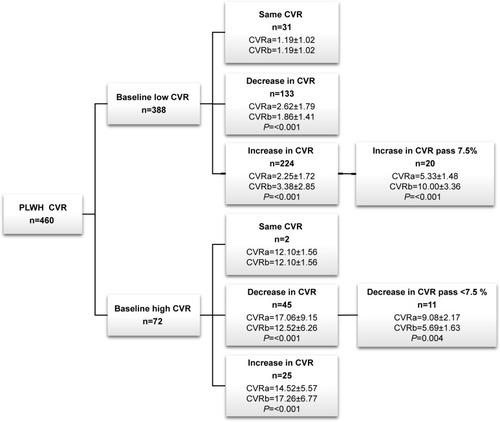
The analysis of the CVR changes over the 1-year period showed that 84.3% (388) of study patients were classified as low CVR at baseline. We found that 34.3% (133/388) of study patients showed a decrease in CVR (P<0.001), whereas 57.7% (224/388) of study patients showed an increase in CVR (P<0.001). Within the latter group, 8.9% (20/224) patients had an increase in CVR >7.5%.
We found that 15.7% (72) study patients showed high CVR. Of these patients, 62.5% (45/72 patients) showed a decrease in CVR, and 24.4% (11/45) of patients switched to a low CVR value ().
Figure 1 Distribution of CVR changes in the study population; CVR according to the ASCVD risk estimator.
Abbreviations: ASCVD, atherosclerotic cardiovascular disease; CVR, cardiovascular risk; PLWH, people living with HIV.
We found an increase in FG levels in the low and high CVR groups (P<0.05). The median triglyceride values in the high CVR group decreased (P<0.05) after a 1-year period ().
Table 2 Metabolic and clinical parameters during the study of CVR assessment in PLWH
We performed a subgroup analysis with regard to extreme changes. Twenty patients had an increase in their CVR above the 7.5% value, and eleven had a decrease in their CVR below the 7.5% cutoff. In the low CVR subgroup, TC and BP increased (P<0.05). The high CVR group showed a decrease in TC, triglyceride levels, and BP (P<0.05; ).
Table 3 Metabolic and clinical changes among PLWH with extreme CVR changes
Discussion
Although some studies have suggested an association between MS and the risk of CVD and diabetes in PLWH, the role of MS as an independent predictor of CVD risk is unclear.Citation20 According to the NCEP-ATP III criteria, the frequency of MS in this cohort presents an intermediate tendency compared with other studies.Citation18–Citation20
Although the high CVR group reported large numbers of antihypertensive, hypoglycemic, and lipid-lowering prescriptions, the prevalence of MS was high most likely because of the extended time of HAART use and time of HIV diagnosis.Citation20–Citation22 The presence of MS can increase CVD and diabetes risks.Citation19,Citation20
After CVR stratification, the analysis showed a significant CVR increase in 57.7% of the patients in the low CVR group after a 1-year period.
In the high CVR group, we found that PI plus NRTI was the most frequently used HAART, which was consistent with the Data Collection of Adverse Events due to Anti-HIV Drugs (DAD) studyCitation6 and other studies,Citation23–Citation25 in which the use of PI, a non-NRTI (NNRTI), or both, increased the CVD prevalence. Furthermore, when a PI, an NNRTI, or both are prescribed, the risk of MI increased up to 26% each year.Citation26 Our study found an MI prevalence of 2.6%, which was potentially related to the previous use of PI and NNRTI.
The results of a T2DM diagnosis in our study were not surprising because of the elevated prevalence of this disease in Mexico; however, it differed from those in the DAD study.Citation27 The FG increased in the low CVR group; however, this value remained at a controlled level according to the NCEP-ATP III recommendations. This increase might be the result of inducing decrements in insulin sensitivity resulting from PI treatment use.Citation8,Citation27
The low CVR group in our study showed a significant increase in TC, and this factor was one of those that significantly changed among the patients who showed extreme changes in CVR. The NRTI + PI regimens were mostly used for the low and high CVR groups as in previous studies,Citation6,Citation8 in which patients undergoing this regimen showed increases in TC levels compared with naive patients. HAARTs might contribute to CVD associated with an increased risk of atherosclerosis.Citation26,Citation28 A triglyceride reduction was found in the low and high CVR groups, but it was not enough to achieve the NCEP-ATP III goals, in which the reduction was apparently due to the wide use of statin therapy. Moreover, its use in this population might explain the CVR changes over a 1-year period.
The CD4+ cell count of our sample increased after a 1-year period. Although this result was not significant, it revealed a desirable immunological trend in these patients. Previous reports have shown that CVR factors and a low CD4+ cell count are independently associated with the risk of CVD events.Citation29 Better approaches for analyzing the immunological contributions from CD4+ cells are required.
Our results provide valuable information concerning the identification of CVR factors in a population of Mexican PLWH, suggesting that the assessment of such risk factors leads to CVR improvements and, consequently, CVD prevention. Although the NCEP-ATP III results strongly suggest measuring lipid profiles, they do not provide specific recommendations regarding how often CVR should be addressed in PLWH. However, our findings suggest that a CVR assessment each year is reliable enough to detect the variations that can lead to CVD.
Study limitations
The design used for this study was limited to only observing and analyzing CVR changes; it did not analyze the therapeutic interventions performed during the year. Clinical information was missing from patient’s records, including family histories of dyslipidemia and T2DM in addition to low-density lipoprotein cholesterol (LDL-C) measurements. Information about patients’ alcohol use was also missing. It was not possible to completely analyze the quality of the lipid-lowering treatments in the study sample because of the missing data. Our study did not have a control group.
Conclusion
More than 50% of PLWH in this sample had an increase in CVR after 1 year. Of these patients, 4.3% were those who changed from the low to high CVR group. The CVR estimator showed usefulness as a potential routine CVR assessment tool in the studied Mexican population. The opportune assessment of the risk factors that determine increases in CVD among PLWH in addition to the use of the CVR estimator should be employed routinely by medical practitioners working in the HIV/AIDS field. Opportune detection and interventions that address modifiable risk factors should be implemented and evaluated to improve the patients’ quality of life. Although the guidelines proposed different time periods for performing CVR estimations, this study showed that such assessments offered valuable clinical data over a relatively short-term period.
Availability of data and materials
All the data can be obtained from the first author and corresponding author on request or http://doi.org/10.3886/ E101082V1.Citation30
Author contributions
Study design, data collection, data analysis, and manuscript writing: AC-P. Study design, data analysis, and manuscript writing: MAS-A. Study design and manuscript writing: SG-J. Study design and manuscript writing: EP-M. Study design and manuscript writing: GB-F. Manuscript writing: MC-M. Data analysis and manuscript writing: LA-J. Study design, data collection, data analysis, and manuscript writing: CDT-J. All the authors read and approved the final manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors recognize the valuable contribution of Matthew Borrego, PhD, from the University of New Mexico, College of Pharmacy, Albuquerque, NM, USA, and to the appreciable support from the National Council of Science and Technology (CONACyT) for the funding through grant 354676 “Taken in part from the experimental work of the Pharm. Thesis of Cibrián Ponce Angelica”. A special thanks to the study participants for their valuable contribution to the study.
Disclosure
The authors report no conflicts of interest in this work.
References
- Info, AIDS, and US Department of Health and Human ServicesGuidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and AdolescentsUSAOffice of AIDS Research Advisory Council (OARAC)20131267 Available from: https://aidsinfo.nih.gov/content-files/adultandadolescentgl003371.pdfAccessed September 14, 2018
- RodgerAJLodwickRSchechterMMortality in well controlled HIV in the continuous antiretroviral therapy arms of the SMART and ESPRIT trials compared with the general populationAIDS201327697397923698063
- CurrierJSLundgrenJDGuidelines for managing cardiovascular risk: an evolving areaCurr Opin HIV AIDS20083320520619372967
- AboudMElgalibAPomeroyLCardiovascular risk evaluation and antiretroviral therapy effects in an HIV cohort: implications for clinical management: the CREATE 1 studyInt J Clin Pract20106491252125920653801
- FabbianiMCiccarelliNTanaMCardiovascular risk factors and carotid intima-media thickness are associated with lower cognitive performance in HIV-infected patientsHIV Med201314313614422994586
- Friis-MøllerNWeberRReissPCardiovascular disease risk factors in HIV patients – association with antiretroviral therapy. Results from the DAD studyAIDS20031781179119312819520
- Li VecchiVMaggiPRizzoMMontaltoGThe metabolic syndrome and HIV infectionCurr Pharm Des201420314975500324320034
- GrinspoonSCarrACardiovascular risk and body-fat abnormalities in HIV-infected adultsN Engl J Med20053521486215635112
- DesvarieuxMBoccaraFMeynardJLInfection duration and inflammatory imbalance are associated with atherosclerotic risk in HIV-infected never-smokers independent of antiretroviral therapyAIDS201327162603261424100713
- GrinspoonSKGrunfeldCKotlerDPState of the Science ConferenceCirculation200811819821018566320
- FeinsteinMJNanceRMDrozdDRAssessing and Refining Myocardial Infarction Risk Estimation Among Patients With Human Immunodeficiency Virus: A Study by the Centers for AIDS Research Network of Integrated Clinical SystemsJAMA Cardiol20162155162
- SecretaríaSGuía de manejo antirretroviral de las personas que viven con VIHMéxicoSecretarıa de Salud, Gobierno de México2014 Available from: http://www.censida.salud.gob.mx/descargas/principal/Guia_ARV_2014V8.pdfAccessed September 14, 2018
- DubéMPSteinJHAbergJAGuidelines for the evaluation and management of dyslipidemia in human immunodeficiency virus (HIV)-infected adults receiving antiretroviral therapy: recommendations of the HIV Medical Association of the Infectious Disease Society of America and the Adult AIDS Clinical Trials GroupClin Infect Dis200337561362712942391
- LichtensteinKAArmonCBuchaczKProvider compliance with guidelines for management of cardiovascular risk in HIV-infected patientsPrev Chronic Dis201310E1023347705
- ChamnanPSimmonsRKSharpSJRepeat Cardiovascular Risk Assessment after Four Years: Is There Improvement in Risk Prediction?PLoS One2016112e014741726895071
- SteinJHManaging cardiovascular risk in patients with HIV infectionJ Acquir Immune Defic Syndr200538211512315671795
- WilliamsLNational Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final reportCirculation200210625314342112485966
- GuevaraFOCañónBLiévanoMCPrevalencia de síndrome metabólico en pacientes infectados con VIH [Prevalence of metabolic syndrome in HIV infected patients]Acta Med Colomb200833283
- SamarasKWandHLawMPrevalence of metabolic syndrome in HIV-infected patients receiving highly active antiretroviral therapy using International Diabetes Foundation and Adult Treatment Panel III criteriaDiabetes Care20073011311917192343
- KrishnanSSchoutenJTAtkinsonBMetabolic syndrome before and after initiation of antiretroviral therapy in treatment-naive HIV-infected individualsJ Acquir Immune Defic Syndr201261338138922828718
- Data Collection on Adverse Events of Anti-HIV Drugs Study GroupSabinCAd’Arminio MonforteAChanges over time in risk factors for cardiovascular disease and use of lipid-lowering drugs in HIV-infected individuals and impact on myocardial infarctionClin Infect Dis20084671101111018461712
- GrinspoonSKMetabolic syndrome and cardiovascular disease in patients with human immunodeficiency virusAm J Med2005118232815639205
- Mary-KrauseMCotteLSimonAClinical Epidemiology Group from the French Hospital Database. Increased risk of myocardial infarction with duration of protease inhibitor therapy in HIV-infected menAIDS2003172479248614600519
- CraneHMvan RompaeySEKitahataMMAntiretroviral medications associated with elevated blood pressure among patients receiving highly active antiretroviral therapyAIDS20062071019102616603854
- RiddlerSASmitEColeSRImpact of HIV infection and HAART on serum lipids in menJAMA2003289222978298212799406
- BozzetteSAAkeCFTamHKChangSWLouisTACardiovascular and cerebrovascular events in patients treated for human immunodeficiency virus infectionN Engl J Med2003348870271012594314
- CarrASamarasKThorisdottirADiagnosis, prediction, and natural course of HIV-1 protease-inhibitor-associated lipodystrophy, hyperlipidaemia, and diabetes mellitus: a cohort studyLancet199935391702093209910382692
- BehrensGDejamASchmidtHImpaired glucose tolerance, beta cell function and lipid metabolism in HIV patients under treatment with protease inhibitorsAIDS19991310F63F7010416516
- Friis-MøllerNWeberRReissPCardiovascular disease risk factors in HIV patients – association with antiretroviral therapy. Results from the DAD studyAIDS20031781179119312819520
- CibriánASánchezMAGarcíaSChanges in cardiovascular risk and clinical outcomes in a HIV/AIDS cohort study over a one-year period at a specialized clinic in Mexico2017
