Abstract
Aim
To compare endoscopic papillary large balloon dilation (EPLBD) alone with EPLBD following endoscopic sphincterotomy (EST) in patients with large and/or multiple common bile duct stones.
Methods
We conducted a comprehensive search of PubMed, EMBASE, and the Cochrane Library database to identify relevant available articles until July 19, 2018. Complete common bile duct stone (CBDS) removal rate, frequency of mechanical lithotripsy (ML) usage, total procedure time and intra- and postoperative adverse events were analyzed. We used RevMan 5.3 to perform the pooled analyses.
Results
Seven RCTs matched the selection criteria. A total of 369 patients underwent EPLBD alone, and 367 patients underwent EPLBD following EST. Our meta-analysis revealed that there were no significant differences in terms of initial success rate (OR =0.69, 95% CI=0.44–1.09, P=0.11), frequency of ML usage (OR =1.18, 95% CI=0.68–2.05, P=0.55), rate of post-endoscopy pancreatitis (PEP) (OR =0.88, 95% CI=0.43–1.78, P=0.72), total procedure time (MD =1.52, 95% CI=-0.13–3.17, P=0.07), or other intra- and postoperative adverse events between the groups for patients with large and/or multiple CBDSs.
Conclusions
EPLBD alone was comparable to EPLBD with prior EST in patients with large and/or multiple CBDSs. Further studies are required to confirm the mechanisms of PEP in patients who accept EPLBD during endoscopic retrograde cholangiopancreatography (ERCP).
Introduction
Since endoscopic sphincterotomy (EST) was first reported in 1974 by Kawai et al,Citation1 it has gradually become a well-established treatment option for common bile duct stones (CBDSs). Endoscopic papillary balloon dilation (EPBD) was first introduced in 1982 by Staritz et al.Citation2 Due to the advantages of reduced risks of bleeding and perforationCitation3 and the successful application in patients with surgically altered anatomy,Citation4 EPBD is an alternative to EST in patients with choledocholithiasis. EPBD protects the function of papillary sphincter; however, it may be accompanied by increased rates of post-endoscopic pancreatitis (PEP).Citation5
Endoscopic papillary large balloon dilation (EPLBD) with prior EST was introduced in 2003 by Ersoz et alCitation6 for the treatment of patients with unsuccessful extraction of large CBDSs by EST and standard basket/balloon. Although EST with a large incision may be effective to achieve stone clearance and may have a clearance rate similar to that of EPLBD with prior EST for large and/or multiple CBDSs, the former procedure increases the risk of adverse events such as bleeding and perforation and more mechanical lithotripsy (ML) would be required.Citation7 As for EPLBD vs EPBD use in patients with large and/or multiple CBDSs, EPLBD has been proven to require fewer endoscopy sessions and lower frequency of ML usage.Citation8,Citation9
After years of application and development, EPLBD with prior EST gradually became a widely used technique for treatment of large and/or multiple CBDSs because of its safety and efficacy.Citation10–Citation12 With the development of therapeutic principle, simplified procedures and assurance of therapeutic effects in strategies of endoscopic procedures were required, EPLBD alone gradually became an attractive option.Citation13 The international consensus guidelines for EPLBDCitation12 and the Japan Gastroenterological Endoscopy Society guidelines for EPLBDCitation11 both suggested that EPLBD can be successfully used for large and/or multiple CBDSs with or without EST; however, the evidence level about whether EST is necessary was low. Meanwhile, EPLBD with prior EST was thought to improve the clearance rate in the initial session and might reduce the usage of ML. Recently, the results of a random-ized controlled trial (RCT) with 200 patients were published by Park et al,Citation13 the results for EPLBD alone and EST with EPLBD were similar in their study.
Due to these conflicting findings and the outcomes reported in the RCT, we carried out a meta-analysis to compare EPLBD alone with EPLBD following EST in patients with large and/or multiple CBDSs, in terms of initial success rate, the frequency of ML usage, total procedure time and rate of PEP and other intra- and postoperative adverse events.
Methods and materials
Search strategies
The present research was conducted according to the PRISMA statement.Citation14 Two authors searched electronic databases, including MEDLINE, EMBASE, and the Cochrane Library to identify relevant articles until July 19, 2018. The search terms included: “balloon dilation,” “balloon dilatation,” “endoscopic papillary balloon dilation,” “endoscopic papillary balloon dilatation,” “endoscopic papillary large balloon dilation,” “endoscopic papillary large balloon dilatation,” “EPBD” and “EPLBD” combined with the terms “sphincterotomy,” “EST,” and “ES.” Furthermore, ClinicalTrials.gov and the reference lists of included studies were reviewed. The searches were limited to articles published in English.
Inclusion and exclusion criteria
The inclusion criteria were as follows: 1) EPLBD with or without EST was used in patients suffering from large (no less than 10 mm) or multiple CBDSs; 2) the diameter of the balloon was no less than 10 mm; 3) the study included a comparison of EPLBD alone and EPLBD with prior EST; 4) patients were aged 18 years or older; 5) study was a randomized clinical trial (RCT); 6) study presented at least one outcome of interest. The exclusion criteria were as follows: 1) non-RCT; 2) duplicated report. Two investigators scrutinized the titles and abstracts of all identified articles to exclude irrelevant studies first and then read the full texts to further exclude unqualified studies. A third author would intervene if consensus was not reached.
Data extraction and quality assessment
Data extraction was carried out by predesigned forms. One author extracted the following data that was checked carefully by other authors: 1) basic information about the included studies (study design, study comparison, inclusion criteria of CBDSs, diameter of the balloon used in both groups, and whether post-procedure biliary drainage was used); 2) demographics and clinical characteristics of the patients (stone size, maximum CBDS diameter, number of periampullary diverticula, and total bilirubin prior to procedure); 3) intraoperative and postoperative outcomes (initial success rate, overall success rate, no of sessions for complete stone removal, total adverse events, frequency of ML usage, rate of PEP, bleeding, and perforation).
Statistical analysis
The meta-analysis was conducted using RevMan software version 5.3 (The Nordic Cochrane Center, Cochrane Collaboration, Copenhagen, Denmark). A quantitative statistical analysis for dichotomous variables was carried out using the odds ratio (OR) as the summary statistic. Mean differences (MDs) were used as the summary statistic for quantitative analysis of continuous variables. Both the OR and MD values were reported as 95% CI. For those studies comprising continuous data, the mean and SD were calculated using the methods described by Hozo et alCitation15 if necessary. The level of heterogeneity between studies was evaluated by I2 statistics. I2 <,30% was considered to be low heterogeneity, 30% ≤ I2 ≤50% was considered to be moderate heterogeneity, and I2 >50% represented high heterogeneity. A random-effects model was applied for all comparisons. Statistical significance across the studies was defined as P<0.05.
Sensitivity analysis and assessment of the risk of bias
Sensitivity analysis was performed by removing one study at a time to assess whether the results could be markedly affected by a single study. The Cochrane collaboration tool, which is an instrument for assessing the quality of RCTs, was used to assess the risk of bias for quality assessment of the included trials.
Results
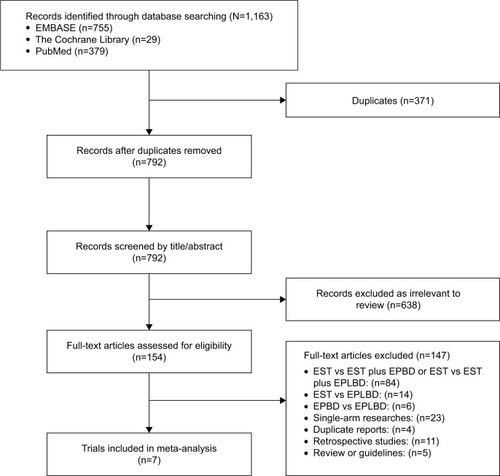
According to the search strategy, a total of 1,163 articles were identified, of which 371 were excluded after deduplication. We then excluded 638 articles that were irrelevant to the topic based on the title and abstract, leaving out 154 articles. Of these, only seven RCTsCitation13,Citation16–Citation21 (including one conference abstract) were finally included in this meta-analysis after full-text assessment. A study selection flow diagram and reasons for final exclusion are shown in .
Figure 1 Study selection process.
Abbreviations: EPBD, endoscopic papillary balloon dilatation; EPLBD, endoscopic papillary large balloon dilatation; EST, endoscopic sphincterotomy.
Seven RCTs included 976 patients in all, and the sample sizes ranged from 60 to 255. The studies were published between 2013 and 2018, and study periods ranged from 2009 to 2015. Only 736 patients were included in the present comparisons. Of these, 369 underwent EPLBD alone, and 367 underwent EPLBD following EST for CBDSs removal. Seven trials were performed in three different countries (three in South Korea, two in China, and two in Egypt). For the study design of the seven including trials, Chu et alCitation21 conducted a 4-arm parallel-group trial comparing the efficacies of EST alone, EPLBD alone, EST plus EPLBD, and EPLBD plus EST (EST plus EPLBD: EST followed by EPLBD, EPLBD plus EST: EPLBD followed by EST); El Wakil et alCitation17 Sarhan et alCitation18 and Guo et alCitation19 conducted 3-arm trials comparing EST alone, EPLBD alone, EST with EPLBD, respectively. The remaining three studiesCitation13,Citation16,Citation20 performed in South Korea were 2-arm trials comparing EPLBD alone vs EPLBD following EST. The inclusion criteria of CBDSs were the maximum CBDS size of at least ≥10 mm (found in most studiesCitation13,Citation19,Citation21 but ≥12 mm in two studies).Citation16,Citation20 Only El Wakil et alCitation17 took the occurrence of large and/or multiple CBDSs as an inclusion criterion of CBDS. The maximum balloon diameter used in the included studies ranged from 10 to 20 mm. Guo et alCitation19 and Park et alCitation13 performed post-procedure biliary drainage using nasobiliary drainage or plastic stents routinely. Chu et alCitation21 used it based on the judgments of the treating physicians. The basic information regarding the seven included trials is presented in and the demographics and clinical characteristics of the patients are shown in .
Table 1 Basic information about the seven included studies
Table 2 Demographics and clinical characteristics of the patients treated by EPLBD alone or EST with EPLBD
Complete CBDSs removal rate
For the rate of successful CBDSs removal in the initial session, all seven studiesCitation13,Citation16–Citation21 reported this outcome, and there was no heterogeneity (I2=0%, P=0.98). The initial success rate was lower in the EPLBD alone groups (316/369, 85.9%) than in the EST with EPLBD groups (328/367, 89.3%); however, the combined result was not statistically significant (OR =0.69, 95% CI=0.44–1.09, P=0.11) (, ). Two studies provided data regarding overall success rate by carrying out multiple sessions. In Park et al’s study,Citation13 the overall success rate of CBDSs removal completely in EPLBD alone group was 92% (92/100) with 77 patients accomplishing this in the first session; 14 patients had two sessions and 1 patient had three sessions. The overall success rate in EST with EPLBD group was 88% (88/100) (78 patients with one session, 7 patients with two sessions, and 3 patients with three sessions). In Chu et al’s study,Citation21 the overall success rate was 97% (29/30) in the EPLBD alone group (20 patients with one session, 4 patients with two sessions, and 5 patients with three sessions) and 94% (31/33) in EST with EPLBD group (26 patients with one session and 5 patients with two sessions) ().
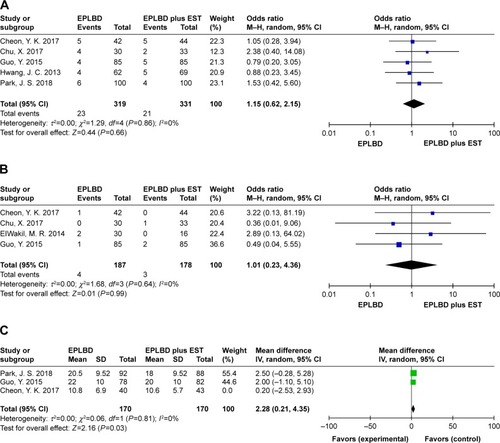
Figure 2 Forest plot of (A) initial success, (B) frequency of mechanical lithotripsy usage, (C) post-endoscopy pancreatitis, and (D) total procedure time.
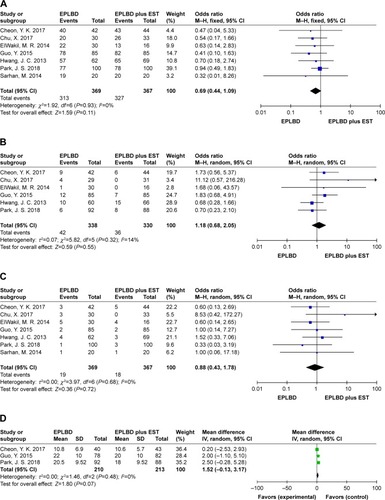
Table 3 Intraoperative and postoperative outcomes
The frequency of mechanical lithotripsy usage
In terms of the use of ML, six studiesCitation13,Citation16,Citation17,Citation19–Citation21 provided data for this outcome with low heterogeneity (I2=14%, P=0.32). The rate was lower in the EST with EPLBD group (36/330, 10.9%) than in the EPLBD alone group (42/338, 12.4%); however, the combined result was not statistically significant (OR =1.18, 95% CI=0.68–2.05, P=0.55) (, ).
Post-endoscopy pancreatitis
All seven trialsCitation13,Citation16–Citation21 provided data for this outcome with no heterogeneity (I2=0%, P=0.68). The rate of PEP was 5.1% (19/369) in the EPLBD alone group and 4.9% (18/367) in the EST with EPLBD group. In all cases, no patients suffered from severe or hemorrhagic PEP and all recovered with conservative treatment. The pooled data revealed that the result was not statistically significant (OR =0.88, 95% CI=0.43–1.78, P=0.72) (, ).
Total procedure time
Three trialsCitation13,Citation19,Citation20 provided data for this outcome, and no heterogeneity (I2=0%, P=0.48) was found. The pooled data demonstrated that the result was not statistically significant (MD =1.52, 95%=-0.13–3.17, P=0.07) (, ).
Other complications
In terms of total intra- and postoperative adverse events, the present meta-analysis revealed that the result was not statistically significant between groups (OR =1.15, 95% CI=0.62–2.15, P=0.66) (, ). The rate of post-endoscopy cholangitis was 2.1% (4/187) in the EPLBD alone group and 1.7% (3/178) in the EST with EPLBD group; the result was also not statistically significant (OR =1.01, 95% CI=0.23–4.36, P=0.99) (, ). The rate of bleeding was 0.5% in both groups (2/369 in the EPLBD alone group and 2/367 in the EST with EPLBD group). The rate of perforation was 0.3% (1/367) in the EST with EPLBD group with no patient suffering from perforation in the EPLBD alone group.
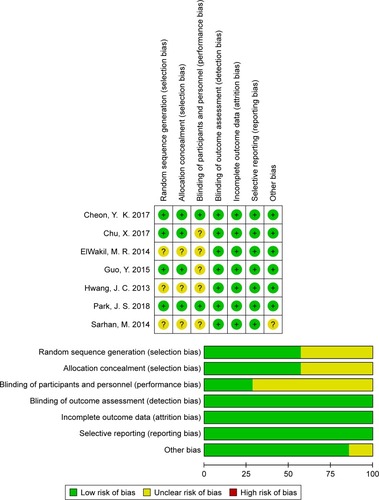
Sensitivity analysis and assessment of the risk of bias
Sensitivity analysis was performed by sequentially removing one trial at each turn to assess whether a single study would markedly affect the results. Sensitivity analysis suggested that the results in this meta-analysis were relatively stable in almost all comparisons except for the total procedure time. When removing Cheon et al,Citation20 total procedure time was significantly longer in the EPLBD alone group than in the EST with EPLBD group (OR =2.28, 95% CI=0.21–4.35, P=0.03) (). The risk of bias of each trial is summarized in . In general, trials included in the present meta-analysis were classified as moderate or high quality.
Discussion
The present meta-analysis revealed that there were no significant differences in terms of initial success rate (OR =0.69, 95% CI=0.44–1.09, P=0.11), frequency of ML usage (OR =1.18, 95% CI=0.68–2.05, P=0.55), rate of PEP (OR =0.88, 95% CI=0.43–1.78, P=0.72), total procedure time (MD =1.52, 95%=-0.13–3.17, P=0.07), or other intra-and postoperative adverse events between EPLBD alone and EST following EPLBD for patients with large and/or multiple CBDSs. The rate of bleeding, perforation and post-endoscopy cholangitis were very low in both groups.
The superiority of EPBD or EPLBD without EST over EST or combined technique during ERCP is well known for patients with high risk of bleeding and surgically altered anatomy.Citation22,Citation23 For general patients with large and/or multiple CBDSs, EPLBD with or without EST was shown to be an at least equal or superior technique to EST alone or EPBD in terms of efficacy and safety.Citation24 For EPLBD, the decision to perform prior EST is generally based on judgments of the clinicians with respect to the patients’ physical conditions. Theoretically, EPLBD alone is more conveniently performed than EST with EPLBD for EST being omitted, and EPLBD alone is more frequently performed in patients with high risk of bleeding such as liver cirrhosis or antiplatelet drug use.Citation12,Citation25 On the other hand, EPLBD following limited or medium EST can provide a larger orifice that may make it more convenient to remove the CBDSs and it may reduce the procedure time and number of endoscopic sessions required for complete stone removal. The result of pooled data in two included trialsCitation13,Citation21 showed that 19.8% (24/121) of patients in the EPLBD alone group and 13.2% (15/114) of patients in the EST with EPLBD group required more than one session for total CBDSs clearance. The present meta-analysis demonstrated that there were no significant differences in initial success rate (OR =0.69, 95% CI=0.44–1.09, P=0.11) or total procedure time (MD =1.52, 95%=-0.13–3.17, P=0.07). These results may be explained by the notion that EPLBD alone may be more convenient to perform but more sessions may be required for total CBDSs clearance than EPLBD with a prior EST.
The mechanisms of PEP are not clearly defined, it was widely believed to be related to the compression on the pancreatic duct by balloon during dilation previously. For this reason, EST before EPLBD with a limited or medium incision in the direction of 11 or 12 points was thought to reduce pressure on the pancreatic duct by the balloon and the pressure of the balloon could be released in the direction of the incision. Thus, EPLBD following EST was thought to reduce the risk of PEP. Nevertheless, current studies suggested that EPLBD alone is safe and effective to treat large CBDSs without increasing the rate of PEP.Citation26 Fujisawa et alCitation27 reviewed studies of balloon dilation and reevaluated the incidence of PEP, and concluded that PEP may not be caused by papillary damage, suggesting that the catheterization of the EPLBD was not the main reason for PEP, whereas the frequency of ML usage and total procedure time may be the main reasons for patients suffering from PEP. In addition, Park et alCitation28 performed a multicenter retrospective study with 946 patients who underwent EPLBD (balloon size 12–20 mm), and their results suggested that balloons $14 mm in diameter were associated with a lower risk of pancreatitis (OR =0.27, P=0.015). In our present meta-analysis, the frequency of ML usage and total procedure time were both higher in the EPLBD alone group than in the EPLBD with EST group (ML: 12.4% vs 10.9%), and the rate of PEP was higher in the EPLBD alone group (PEP: 5.1% vs 4.9%). Although the differences were not statistically significant, this may further prove this point of view. Further studies are needed to confirm the mechanisms of PEP in patients undergoing EPLBD during ERCP. Recent studies showed that post-endoscopy biliary drainage with nasobiliary drainage or biliary stent reduced the incidence of PEP. In an RCT performed by Huang et alCitation29 of 160 patients in China, PEP was significantly lower in the endoscopic nasobiliary drainage (ENBD) catheter group (1.28% vs 10.4%; P=0.018). To avoid the occurrence of PEP, two of the included trialsCitation13,Citation19 performed post-procedure biliary drainage routinely and Chu et alCitation21 performed it on the judgment of the treating physicians. Besides, prophylactic pancreatic stenting has been proven effective in preventing the occurrence of PEP, and it has been recommended in all patients with pancreatic guidewire-assisted biliary cannulation.Citation23 However, there is still a lack of relevant clinical study about prophylactic pancreatic duct stenting in EPLBD to prevent PEP. More clinical data are needed to assess its feasibility and efficacy.
Although the safety and effectiveness of EPLBD with or without EST have been proven, the contraindications to EPLBD should still be mentioned. In addition to the contraindications in patients with a high risk of bleeding during ERCP, perforation, which is a serious complication, should be mentioned. A retrospective studyCitation28 performed in South Korea revealed that distal CBD stricture independently predicted perforation. In view of this result, EPLBD is not recommended in patients with obvious stricture of the distal bile duct.Citation11,Citation12 Meanwhile, the functional recovery of sphincter of Oddi (SO) after EPLBD should also be noted. Cheon et alCitation20 found that SO function was not recovered after 1 year and the loss of SO function in the EPLBD alone group and the EPLBD following EST group was persistent and comparable in their research.
Finally, there were several limitations in the present meta-analysis. First, the inclusion criteria for CBDs varied across the trials, possibly leading to bias to this meta-analysis; meanwhile, the most common size was $10 mm, and it is different from the commonly clinical endoscopy practice (>15 mm), and we could not proceed with further analysis based on the size of stones because of the lack of more detailed data. Second, the maximum balloon diameter used in the included trials varied, the maximum balloon diameter used in Guo et alCitation19 and El Wakil et alCitation17 trials was 15 mm while maximum balloon diameter was 20 mm in the other trials; however, we were not sure whether the results would be affected by this difference. Third, only three of the included trials reported the use of post-endoscopy biliary drainage. This may lead to bias in the result of PEP rate, and further subgroup analysis could not be implemented because of the lack of detailed information.
Conclusion
EPLBD alone was comparable to EPLBD with prior EST during ERCP in patients with large and/or multiple CBDSs. Although there were advantages in the rate of initial success, the frequency of ML usage, the rate of PEP, and total procedure time, these results were not statistically significant. Further studies are required to confirm the mechanisms of PEP in patients undergoing EPLBD during ERCP.
Disclosure
The authors report no conflicts of interest in this work.
References
- KawaiKAkasakaYMurakamiKTadaMKoliYNakajimaMEndoscopic sphincterotomy of the ampulla of VaterGastrointest Endosc19742041481514825160
- StaritzMEweKMeyer Zum BüschenfeldeKHEndoscopic papillary dilatation, a possible alternative to endoscopic papillotomyLancet19821828413061307
- LiuYSuPLinSEndoscopic papillary balloon dilatation versus endoscopic sphincterotomy in the treatment for choledocholithiasis: a meta-analysisJ Gastroenterol Hepatol201227346447121913984
- ItoKMasuKKannoYOhiraTNodaYAmpullary intervention for bile duct stones in patients with surgically altered anatomyDig Endosc201426Suppl 211612124750160
- WeinbergBShindyWLoSCochrane Hepato-Biliary GroupEndoscopic balloon sphincter dilation (sphincteroplasty) versus sphincter-otomy for common bile duct stonesCochrane Database Syst Rev2006331Cd004890
- ErsozGTekesinOOzutemizAOGunsarFBiliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extractGastrointest Endosc200357215615912556775
- JinPPChengJFLiuDMeiMXuZQSunLMEndoscopic papillary large balloon dilation vs endoscopic sphincterotomy for retrieval of common bile duct stones: a meta-analysisWorld J Gastroenterol201420185548555624833886
- FujisawaTKagawaKHisatomiKKubotaKNakajimaAMatsuhashiNEndoscopic papillary large-balloon dilation versus endoscopic papillary regular-balloon dilation for removal of large bile-duct stonesJ Hepatobiliary Pancreat Sci201421640540924123873
- HakutaRKawahataSKogureHEndoscopic papillary large balloon dilation and endoscopic papillary balloon dilation both without sphincterotomy for removal of large bile duct stones: a propensity-matched analysisEndoscopy2018626 Epub ahead of print
- DoshiBYasudaIRyozawaSLeeGHCurrent endoscopic strategies for managing large bile duct stonesDig Endosc201830Suppl 1596629658655
- ItoiTRyozawaSKatanumaAJapan Gastroenterological Endoscopy Society guidelines for endoscopic papillary large balloon dilationDig Endosc201830329330929411902
- KimTHKimJHSeoDWInternational consensus guidelines for endoscopic papillary large-balloon dilationGastrointest Endosc2016831374726232360
- ParkJSJeongSLeeDKComparison of endoscopic papillary large balloon dilation with or without endoscopic sphincterotomy for the treatment of large bile duct stonesEndoscopy201873 Epub ahead of print
- LiberatiAAltmanDGTetzlaffJThe PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaborationBMJ2009339b270019622552
- HozoSPDjulbegovicBHozoIEstimating the mean and variance from the median, range, and the size of a sampleBMC Med Res Methodol2005511315840177
- HwangJCKimJHLimSGEndoscopic large-balloon dilation alone versus endoscopic sphincterotomy plus large-balloon dilation for the treatment of large bile duct stonesBMC Gastroenterol20131311523324454
- El WakilMRMAbdelkaderNASalemHE-DMHalima AboASDifferent techniques for management of common bile duct stones: a single centre experienceJ Egypt Soc Parasitol201444353954625643496
- SarhanMEnabaMEl-BedewyMEl Raouf Sarhan Sarhan MEA. Is combination of biliary sphincterotomy and balloon dilation a better option than either alone in endoscopic removal of bile duct stones? A comparative studyJ Gastroenterol Hepatol201429154
- GuoYLeiSGongWA preliminary comparison of endoscopic sphincterotomy, endoscopic papillary large balloon dilation, and combination of the two in endoscopic choledocholithiasis treatmentMed Sci Monit20152126072612 http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/572/CN-01097572/frame.html26334173
- CheonYKLeeTYKimS-NShimCSImpact of endoscopic papillary large-balloon dilation on sphincter of Oddi function: a prospective randomized studyGastrointest Endosc2017854e781782790
- ChuXZhangHQuRSmall endoscopic sphincterotomy combined with endoscopic papillary large-balloon dilation in the treatment of patients with large bile duct stonesEur Surg2017491916 http://cochranelibrary-wiley.com/o/cochrane/clcentral/articles/294/CN-01332294/frame.html
- KamadaKItoiTSofuniASu1641. Efficacy and safety of EPLBD for bile duct stones in patients with surgically altered anatomy: a large case series at single high volume centerGastrointest Endosc2015815AB362
- TestoniPAMarianiAAabakkenLPapillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical GuidelineEndoscopy201648765768327299638
- ParkCHJungJHNamEComparative efficacy of various endoscopic techniques for the treatment of common bile duct stones: a network meta-analysisGastrointest Endosc2018871e104357
- LiQLGaoWDZhangCIs endoscopic sphincterotomy plus large-balloon dilation a better option than endoscopic large-balloon dilation alone in removal of large bile duct stones? A retrospective comparison studyIndian J Cancer201551Suppl 2e13e1725712833
- ParkJSKimTNKimKHEndoscopic papillary large balloon dilation for treatment of large bile duct stones does not increase the risk of post-procedure pancreatitisDig Dis Sci201459123092309824996378
- FujisawaTKagawaKHisatomiKKubotaKNakajimaAMatsuhashiNIs endoscopic papillary balloon dilatation really a risk factor for post-ERCP pancreatitis?World J Gastroenterol201622265909591627468185
- ParkSJKimJHHwangJCFactors predictive of adverse events following endoscopic papillary large balloon dilation: results from a multicenter seriesDig Dis Sci20135841100110923225136
- HuangQShaoFWangCQiWQiuLJLiuZNasobiliary drainage can reduce the incidence of post-ERCP pancreatitis after papillary large balloon dilation plus endoscopic biliary sphincterotomy: a randomized controlled trialScand J Gastroenterol201853111411929043861