Abstract
Background
Valvular aortic stenosis is a common disease in the elderly, often in multimorbid patients. It is often associated with coronary artery disease and peripheral artery disease. In this situation, the risk of conventional open-heart surgery is too high, and other treatment strategies have to be evaluated.
Case report
A 79-year-old female patient with severe aortic stenosis, coronary artery disease and end-stage chronic obstructive pulmonary disease suffering from dyspnea at rest and permanently dependent on oxygen was treated in three steps. Firstly, her pulmonary infection was treated with antibiotics for 7 days. Then, the left anterior descending artery was stented (bare-metal stent). In the same session, valvuloplasty of the aortic valve was performed. She was sent to rehabilitation to improve her pulmonary condition and took clopidogrel for 4 weeks. Finally, she underwent transapical aortic valve replacement. She was released to rehabilitation on postoperative day 12.
Conclusion
A combination of modern interventional and minimally invasive surgical techniques to treat aortic stenosis and coronary heart disease can be a viable option for multimorbid patients with extremely high risk in conventional open-heart surgery.
Introduction
Severe aortic stenosis can only be treated adequately with some form of aortic valve replacement, either conventionally with a median (or partial) sternotomy and open-heart surgery, with a minimally invasive left thoracotomy on the beating heart (transapical), or via access over the peripheral vessels (transfemoral/transaxillary) without opening the chest at all.Citation1–Citation3 Sometimes, patients with aortic stenosis also have severe concomitant diseases which dramatically increase the risk of the standard surgical procedures. Treating these patients requires a multidisciplinary approach with a combination of procedures that are performed one after another.
Case report
We report on a 79-year-old female patient who presented with dyspnea at rest (New York Heart Association IV) and chest pain. She had a history of smoking (63 pack years) and end-stage chronic obstructive pulmonary disease with a forced expiratory volume in 1 second (FEV1) at admittance of 0.64 L and saturation at rest of 72%. She took steroids orally, inhaled tiotropium bromide, steroids, and β2-mimetics and had an indication for long-term oxygen therapy.
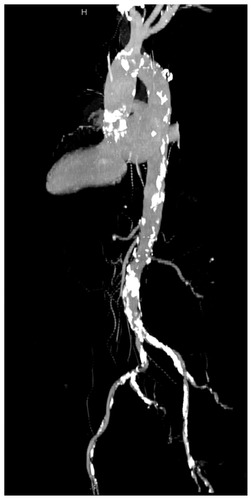
Echocardiography revealed severe aortic stenosis with an effective orifice area of 0.3 cm2, a mean gradient of 50 mmHg, and mitral regurgitation of II°. Ejection fraction was not impaired. Heart catheterization was performed because of a positive troponin test and showed coronary heart disease with stenoses in all three main vessels. The left anterior descending artery (LAD) was the biggest coronary artery, filling the chronically occluded right coronary artery retrograde. The circumflex artery was small. Computed tomography angiography revealed severe calcifications around the aortic arch and along the whole thoracic and abdominal aorta down to the femoral arteries which were only 6.5 mm in diameter (). The patient had had thromboendarterectomy of the left internal carotid artery in 2003 and had a moderate stenosis of the right (<70%). At admission, she was also suffering from pneumonia. Under these conditions, our anesthesiologists decided to postpone the aortic valve replacement surgery as she would not have been able to tolerate general anesthesia. A multidisciplinary approach was scheduled. Firstly, her infection was treated with antibiotics (tazobactam + piperacillin) for 7 days until leukocytes and C-reactive protein (CRP) normalized. Then we performed the first interventional step: the patient underwent cardiac catheterization and the LAD, which was the patient’s largest and most important coronary artery, was dilated and a bare-metal stent was placed. The circumflex artery was small, and the right coronary artery was chronically occluded after myocardial infarction. In the same session, valvuloplasty of the aortic valve was performed successfully without neurological complications and a resulting effective orifice area of 0.9 cm2. After that, the patient was almost symptom-free but had aortic insufficiency of II°. She was sent to rehabilitation to improve her pulmonary condition and took clopidogrel for 4 weeks because of the new bare-metal stent (600 mg loading dose, followed by 75 mg daily). At re-admission, lung function tests were repeated and showed an improved FEV1 with 1.33 L. She was now in a better condition to tolerate general anesthesia, so we performed a transapical aortic valve replacement (Edwards SAPIEN Ø 26 mm; Edwards Lifesciences, Irvine, CA) using a left mini-thoracotomyCitation2 in our hybrid-operating room with a heart-lung machine on standby.
The patient was weaned from the ventilator on the same day. She was in sinus rhythm, had no neurological symptoms, no dyspnea, and could be released to rehabilitation on postoperative day 12. The patient was fine at 6-month follow-up.
Discussion
Regarding the coronary disease of our patient, we limited revascularization to the LAD, as the circumflex artery was small and the right coronary artery chronically occluded after myocardial infarction. A bare-metal stent was chosen over a drug-eluting stent because double anti-platelet therapy is only required for a period of 4 weeks, just enough time to improve the pulmonary function and make general anesthesia with mechanical ventilation possible. Together with the stent implantation, aortic valvuloplasty was performed. This procedure helped reduce pulmonary congestion, which improved pulmonary functions.
Conventional aortic valve replacement with cardiopulmonary bypass under cardioplegic arrest is still the gold standard in the treatment of severe aortic valve stenosis and improves long-term survival compared to medical therapy.Citation4
Without her comorbidities, our patient would have been a candidate for conventional open-heart surgery with aortic valve replacement (bioprosthesis) and coronary artery bypass grafting (CABG), as the literature shows that even in older patients this procedure can be performed with low morbidity and mortality.Citation5,Citation6 In our patient’s case, however, the logistic European System for Cardiac Operative Risk Evaluation predicted a mortality of 40% for the conventional surgical procedure. Furthermore, clamping of the extremely calcified aorta () would have posed a high risk for embolic stroke. Wound healing had to be considered in our patient because of her long-term steroid medication and osteoporosis. Regarding these last factors, the transapical approach with a lateral mini-thoracotomy was, in our opinion, much safer than a median sternotomy.
As the long-term results of valvuloplasty are poorCitation7 and also inferior to transcatheter aortic valve implantation,Citation8 some sort of aortic valve replacement had to be performed thereafter, to resolve the symptoms of the patient and thus improve her quality of life. If the femoral vessels had been large enough (>6.5 mm in diameter for the Medtronic CoreValve delivery sheath which is 18 French) and free of calcifications, the transfemoral access would have been the method of choice because it can be performed without general anesthesia. If there are a lot of calcifications and the vessel is relatively small, as in our case, the risk for peripheral emboli could be reduced using the antegrade (transapical) access.Citation9 For all these reasons, we decided to perform a transapical aortic valve replacement.
Conclusion
A combination of modern interventional and minimally invasive surgical techniques to treat aortic valve stenosis and coronary heart disease can be a viable option for multimorbid patients with an extremely high risk for conventional open-heart surgery. These procedures should then be carried out only in experienced centers with a hybrid-operating room and in a multidisciplinary approach where all kinds of complications, eg, dissection of the femoral vessels, stroke, rhythm disorders, etc, can be handled sufficiently. A cardiac surgeon and a heart-lung machine should always be on standby.
For most patients however, treatment of aortic valve stenosis with valve replacement under cardioplegic arrest remains the gold standard until the long-term durability of interventional valve prostheses is fully evaluated in prospective randomized trials.
Disclosure
The authors report no conflicts of interest in this work.
References
- ElBardissiAWShekarPCouperGSCohnLHMinimally invasive aortic valve replacement in octogenarian, high-risk, transcatheter aortic valve implantation candidatesJ Thorac Cardiovasc Surg2011141232833521047646
- YeJCheungALichtensteinSVSix-month outcome of transapical transcatheter aortic valve implantation in the initial seven patientsEur J Cardiothorac Surg2007311162117126558
- CribierAEltchaninoffHBashAPercutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case descriptionCirculation2002106243006300812473543
- SchwarzFBaumannPMantheyJThe effect of aortic valve replacement on survivalCirculation1982665110511107127696
- LikoskyDSSorensenMJDaceyLJLong-term survival of the very elderly undergoing aortic valve surgeryCirculation2009120Suppl 11S127S13319752357
- AlexanderKPAnstromKJMuhlbaierLHOutcomes of cardiac surgery in patients > or =80 years: results from the National Cardiovascular NetworkJ Am Coll Cardiol200035373173810716477
- OttoCMMickelMCKennedyJWThree-year outcome after balloon aortic valvuloplasty. Insights into prognosis of valvular aortic stenosisCirculation19948926426508313553
- LeonMBSmithCRMackMTranscatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgeryN Engl J Med2010363171597160720961243
- BooneRHAltweggLAMassonJ-BTranscatheter aortic valve implantation in 168 high-risk patients with symptomatic severe aortic stenosis – single centre experience [abstract 3044]Circulation2008118SupplS807