Abstract
Nearly all patients with end-stage renal disease develop hyperphosphatemia. These patients typically require oral phosphate binders for life-long phosphorus management, in addition to dietary restrictions and maintenance dialysis. Recently, niacin, a traditional antilipemic agent, drew attention as an experimental treatment for hyperphosphatemia. The purpose of this article was to report on new findings regarding niacin’s novel effects and to review the possibility of repurposing niacin for hyperphosphatemia treatment in dialysis patients by elucidating its safety and efficacy profiles along with its synergistic clinical benefits. Following approval from the Institutional Review Board, we tracked the yearly trends of order frequency of niacin in comparison with statins and sevelamer in a tertiary care hospital. Also, a Cochrane Library and PubMed literature search was performed to capture prospective clinical trials on niacin’s hypophosphatemic effects in dialysis patients. Niacin use in clinical settings has been on the wane, and the major contribution to that originates from the wide use of statins. Niacin use rates have further plummeted following a trial failure which prompted the suspension of the niacin-laropiprant (a flushing blocker) combination product in the global market. Our literature search identified ten relevant articles. Overall, all studies demonstrated that niacin or nicotinamide (the metabolite form) reduced serum phosphorus levels as well as Ca-P products significantly. Additive beneficial effects on lipid parameters were also observed. Sevelamer appeared superior to niacin in a comparative study, but the study design had several limitations. The intervention dosage for niacin ranged from 375 to 1,500 mg/day, with the average daily dose of approximately 1,000–1,500 mg. Niacin can be a patient-convenient and inexpensive alternative or adjunctive therapy for phosphorus management in dialysis patients. Further well-designed, large-scale, long-term, comparative trials are needed to successfully repurpose niacin for the new indication.
Introduction
Abnormalities in calcium–phosphorus (Ca-P) homeostasis and marked elevations in serum phosphorus levels are characteristic of advanced chronic renal disease.Citation1 Nearly all patients with end-stage renal disease (ESRD) develop hyperphosphatemia, which is a significant risk factor for hypertension, vascular calcification, and substantial cardiovascular morbidity and mortality.Citation2,Citation3 In a study by Kestenbaum et al,Citation4 each 1 mg/dL rise in serum phosphorus was linked to an estimated 23% increased risk of mortality. Therefore, patients with ESRD require tight control of serum phosphorus in the form of dietary restrictions in conjunction with pharmacotherapy and maintenance dialysis.Citation5,Citation6 Current phosphorus-lowering treatments in ESRD patients include calcium-containing phosphate binders and non-calcium containing phosphate binders, such as aluminum hydroxide, sevelamer, and lanthanum carbonate. Studies have shown that all phosphate binders are equally effective in lowering serum phosphorus concentrations.Citation7 However, these agents are not comparable in their cost, toxicity, and tolerability. Therefore, the most appropriate binder must be selected in consideration of several factors, such as side effects of a particular binder as well as individual patient characteristics.
The traditional phosphate binders have common drawbacks that may negatively influence patient adherence to the medication regimen. Calcium salts have fallen out of favor due to possible hypercalcemic events and increased coronary artery and aortic valve calcification risks.Citation7,Citation8 All currently available phosphorus-lowering agents work by binding dietary phosphate in the gastrointestinal (GI) tract, and the chelate is eliminated in the feces, preventing the absorption of phosphorus into the bloodstream. Therefore, these agents must be taken with oral nutrient intake or tube feeding, otherwise they do not work. Other limitations include large pill burden, GI side effects, and aluminum toxicities specifically with aluminum hydroxide.Citation9
Currently, sevelamer, an anion exchange resin, has sustained a clinically preferred safety profile over other calcium-based or non-calcium containing binders because it is not absorbed, hence poses no risk of cation-induced toxicities.Citation10 Among the two available salt forms, the carbonate form of sevelamer is better tolerated in patients than the previous hydrochloride form, as the latter often exacerbates the tendency of patients with advanced kidney disease to metabolic acidosis.Citation11 Also, the new powder formulation of sevelamer carbonate for oral suspension provides a novel, patient-convenient alternative to traditional tablet-form phosphate binders. However, despite the tolerability and formulational improvements, there still exist the disadvantages, such as large dose burden, GI side effects, and the strict direction to be taken three times daily with meals.
Recently, niacin, also known as nicotinic acid and vitamin B3, drew attention as an experimental option for elevated serum phosphorus concentrations in chronic renal disease patients.Citation12–Citation15 Animal models suggested that niacin decreases phosphorus absorption in the GI tract by the direct inhibitory effect of nicotinamide (or niacinamide), a metabolite of niacin, on active sodium-phosphate cotransporter in the small intestine.Citation16,Citation17 This is a distinct mechanism of action from the traditional phosphate binders. Preliminary studies showed that niacin can be a useful primary or add-on therapy for hyperphosphatemia in ESRD patients.Citation12–Citation15 Once-daily oral niacin treatment for elevated serum phosphorus levels has been investigated in a limited number of clinical trials in dialysis patients,Citation18 but the clinical investigation of niacin’s novel effects is still in its early stages.
As the first cholesterol-reducing agent, niacin has well-documented beneficial effects in hyperlipidemia management. It specifically reduces serum triglycerides as well as low-density lipoprotein cholesterol (LDL-C) and most effectively raises high-density lipoprotein cholesterol (HDL-C), by up to 35%.Citation19 Boosting HDL-C levels can be as important as lowering LDL-C because studies have confirmed the status of low HDL-C level as an independent risk factor for cardiovascular events.Citation20,Citation21 Despite the robust evidence for the impact of niacin treatment for dyslipidemia, present-day researchers encounter practical challenges when organizing clinical trials to investigate niacin’s novel effects – the vitamin is now rarely used in clinical settings.
With its cost-effectiveness and additive effects as a traditional dyslipidemia treatment, niacin can be a promising candidate for drug repositioning as a phosphorus-lowering agent in ESRD patients. However, due to a paucity of concrete clinical evidence on its efficacy and safety in comparison with the gold standard phosphorus-lowering therapy, clinicians are still faced with uncertainties in practice as to whether they should consider niacin as a primary or adjunctive hyperphosphatemia treatment in ESRD patients. The purpose of this article was to report on new findings regarding the use of niacin in the treatment of hyperphosphatemia in dialysis patients and to review the possibility of repurposing niacin for the new indication by elucidating its safety and efficacy profiles along with its synergistic clinical benefits.
Methods
After obtaining approval from the Institutional Review Board in June 2014, we tracked the yearly trends of order frequency of niacin in comparison with statins and sevelamer since the adoption of electronic medical records in 1999 at the Ajou University Hospital in Korea.
We also performed a literature search to identify clinical trials of ESRD patients on dialysis that evaluated the effects of niacin and its analog in lowering serum phosphorus concentrations. PubMed and Cochrane Library were searched, without language and geographical restrictions, for articles published since 2004. The search terms included niacin, nicotinic acid, nicotinamide, niacinamide, and hyperphosphatemia. The reference lists of captured articles and previous reviews were also searched to find additional primary literature that may not have been captured through the initial search. Two reviewers independently screened the article titles, abstracts, and full texts to identify clinical trials that may be suitable for inclusion criteria. The inclusion criteria were broken into four categories: 1) only prospective studies, including placebo- or comparator-controlled trials, were eligible; 2) adult patients on hemodialysis or peritoneal dialysis were included; 3) niacin (nicotinic acid) or nicotinamide (niacinamide) must have been used for hyperphosphatemia treatment; and 4) endpoints must include serum phosphorus levels, and other outcome measures include corrected/uncorrected serum Ca, Ca-P product, HDL-C, LDL-C, triglycerides, thrombocytopenia, diarrhea, flushing, pruritus, and rash. We also conducted another search through http://clinicaltrials.gov to identify ongoing clinical trials. A dose-finding study (NCT01200784) was returned through this search, but the results have not yet been published.
Results
Niacin use on the wane
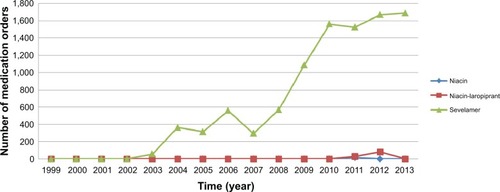
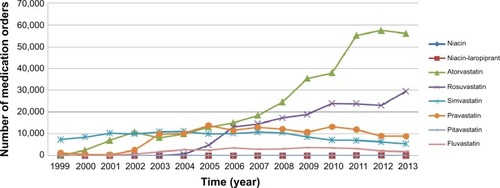
The major contribution to the usage drop originates from the rise of statins, which include the blockbuster cholesterol-lowering medications, such as atorvastatin and rosuvastatin. As an example, the yearly trends of order frequency of niacin versus statins in a tertiary-care hospital with over 1,000 patient-beds in Korea are presented in . Niacin use rates were constantly minimal and have plummeted into near nonexistence since 2012. Conversely, statin use rates, especially atorvastatin and rosuvastatin, have skyrocketed over the past 15 years. Additionally, demonstrates the yearly order patterns of niacin versus sevelamer, the phosphate binder with the most favorable safety profile. The current order patterns clearly show that designing a comparative study between niacin and sevelamer retrospectively is not plausible.
Figure 1 Order frequency of niacin versus statins in a single tertiary-care institution.
Another factor that might have negatively affected the usage rates of niacin is its most prominent side effect, facial flushing. Niacin promotes cutaneous vasodilation via stimulating the production of prostaglandins.Citation22 The subsequent burning sensation is harmless but unpleasant and made it difficult for patients to comply with niacin therapy. Pretreatment with aspirin has been frequently utilized to reduce the incidence of flushing, but provided limited effects. In 2007, Merck developed a new version of niacin (Tredaptive) that was combined with laropiprant, a novel and highly selective prostaglandin D2 receptor subtype 1 inhibitor, to decrease the incidence and intensity of niacin-induced skin flushing.Citation23 However, unexpected adverse effects, such as bleeding and infections, have been reported with the combined niacin-laropiprant product,Citation23 and no concrete evidence has been provided on which component of the combination is responsible for the adverse outcomes. The study results prompted the suspension of Tredaptive worldwide and, since then, the use of niacin has further plummeted. All these factors are posing practical barriers to implementing further clinical investigation on niacin.
Previous study results on niacin’s hypophosphatemic effects
By our literature search, 12 relevant articles were originally identified, and two were excluded as they only included patients free of clinical renal disease. The ten eligible trials enrolled 261 adult patients in the active group and 135 adult patients in the control group. Of the ten articles, five were a placebo-controlled design including two crossover trials, and one was a head-to-head comparison against sevelamer hydrochloride. The important findings from the selected trials are summarized in , including concomitant statin use and changes in lipid parameters. Niacin was the study drug in six trials; while in four trials, the metabolite form of nicotinamide (or niacinamide) was studied. Other phosphate binder use was not strictly limited in five studies. Statin was used concomitantly in three trials, while the remaining trials did not specify the information.Citation12–Citation15,Citation18,Citation24–Citation28
Table 1 Summary of the selected clinical trials of niacin and nicotinamide in end-stage renal disease patients on dialysis
A prospective, open-label study of 2004 in Japan enrolled 65 hemodialysis patients with elevated baseline phosphorus.Citation12 The patients received nicotinamide for 12 weeks, at a starting dose of 500 mg/day, with titration every 2 weeks by 250 mg/day. The serum phosphorus level decreased from 6.9±1.5 to 5.4±1.3 mg/dL (P<0.0001), and the Ca-P product dropped significantly from 59.8±14.5 to 47.3±13.4 mg2/dL2 during the 12-week treatment (P<0.0001). Adverse effects of nicotinamide included reversible thrombocytopenia and diarrhea.
Another prospective, open-label study in India enrolled 34 patients on maintenance hemodialysis with hyperphosphatemia.Citation13 Niacin therapy was initiated at 375 mg/day, with dose increase to twice daily if necessary after 2 weeks of therapy. Following the 8 weeks of treatment, the serum phosphorus level decreased from 7.7±1.5 to 5.6±1 mg/dL (P<0.001), and a concurrent fall in Ca-P product was observed from 63.1±15.1 to 48.7±10.9 mg2/dL2 (P<0.001). Two patients experienced mild pruritus, otherwise niacin was well tolerated.
In a German study of 2007, researchers enrolled 17 dialysis patients who tolerated a daily dose of at least 1,000 mg (average dosage 1,470±110 mg/day).Citation14 Niacin was initiated at 375 mg/day, with titration every 2 weeks to 500, 1,000, 1,500, and 2,000 mg/day, respectively. Six patients stopped therapy prematurely because of flushing, weight loss, or hypotension during dialysis. Overall, serum phosphorus values decreased from 7.2±0.5 to 5.9±0.6 mg/dL (P=0.015). Adverse effects due to niacin were flushing and diarrhea.
A Colombian study of 2008 recruited nine renal disease patients on dialysis with a baseline serum phosphorus level >5.5 mg/dL despite standard phosphate binder treatment.Citation15 Patients were started on niacin 500 mg/day, and 3 months later, the dosage was increased to 1,000 mg/day. The 8-month treatment resulted in a significant reduction in serum phosphorus from 6.46±0.53 to 3.94±0.76 mg/dL (P<0.01). The reduction in Ca-P product was also significant. No adverse events attributable to niacin were reported.
Cheng et alCitation24 enrolled 33 hemodialysis patients with elevated baseline phosphorus in a crossover trial of nicotinamide versus placebo. The patients were randomly assigned to 8 weeks of active or placebo treatment. Nicotinamide was started at 500 mg/day, then the dosage was titrated up to 1,000 mg/day at week 3 and 1,500 mg/day at week 5. A 2-week washout period preceded the switch from treatment to placebo or vice versa. A significant fall in serum phosphorus was achieved, from 6.26±1.28 to 5.47±1.49 mg/dL with nicotinamide (P=0.02), but not with placebo. The Ca-P product also fell significantly with nicotinamide. One patient experienced diarrhea and another complained of a transient rash while receiving nicotinamide. Thrombocytopenia developed in nine patients on nicotinamide and five on placebo.
Young et alCitation25 conducted an 8-week, randomized, placebo-controlled trial of 15 peritoneal dialysis patients with a baseline phosphorus value >4.9 mg/dL. Patients were initiated on nicotinamide 500 mg/day, with titration to 1,500 mg/day. In the active group, the plasma phosphorus fell by an average of 0.7±0.9 mg/dL, and the absolute between-group difference in serum phosphorus levels was 1.1 mg/dL (P=0.037). Two patients in the active arm had to discontinue treatment due to drug-induced adverse effects, such as diarrhea and pruritus.
In an Iranian study by Shahbazian et al,Citation26 48 dialysis patients with hyperphosphatemia were enrolled in an 8-week, randomized, placebo-controlled trial. The initial dose of nicotinamide was 500 mg/day in the first 4 weeks, then the dosage was titrated up to 1,000 mg/day in the remaining 4 weeks. The nicotinamide treatment achieved a significant fall in serum phosphorus levels, from 5.9±0.58 mg/dL to 4.77±1.43 mg/dL at week 4 (P=0.002) and to 4.66±1.06 mg/dL at week 8 (P=0.000). The mean Ca-P product also decreased significantly. Adverse effects related to nicotinamide included thrombocytopenia and diarrhea.
More recently, Aramwit et alCitation18 in Thailand reported the results from a 12-week, randomized, placebo-controlled trial of 28 hemodialysis patients with hyperphosphatemia. The initial niacin dose was 375 mg/day, with titration once weekly to 500, 750, and 1,000 mg/day, as tolerated. The average serum phosphorus of the active group decreased significantly from 7.13±1.09 mg/dL to 5.65±1.22 mg/dL (P<0.001). However, the between-group difference in the post-intervention serum phosphorus levels was not significant. The level of Ca-P product dropped significantly in the treatment group (P<0.001). One patient experienced niacin-induced hot flushes.
In a crossover study by Edalat-Nejad et alCitation27 37 hemodialysis patients with hyperphosphatemia were randomly assigned to placebo or niacin with titration every 2 weeks from 400 to 600, 800, and 1,000 mg/day, respectively. After a washout period of 2 weeks, the patients were placed on the alternative therapy for the next 8 weeks. During the 8-week niacin treatment, serum phosphorus decreased from 6.66±1.40 to 5.96±0.87 mg/dL (P=0.006). Common adverse effects related to niacin included flushing, GI symptoms, and mild pruritus.
Lastly, Ahmadi et alCitation28 in Iran conducted the first head-to-head comparative study of niacin against sevelamer hydrochloride in 40 hemodialysis patients with hyperphosphatemia. Flat doses of 500 mg/day for niacin versus 1,600 mg/day for sevelamer were used during the 4-week study period. Both groups demonstrated a significant drop in serum phosphorus (2.2±0.6 mg/dL, P<0.0001 and 1.7±1 mg/dL, P=0.004, respectively). Reduction in the Ca-P product in the sevelamer group was 21.6±7 (P<0.0001), while that of the niacin group was 16.3±11 (P=0.007). Sevelamer appeared superior to niacin in this short-term study.
Discussion
As niacin’s clinical use has been traditionally limited to dyslipidemia treatment, institutional electronic medical records mostly lack baseline and repeated phosphorus measures which are essential to examine the vitamin’s potential effects on serum phosphorus as well as Ca-P products. The paucity of relevant data in addition to Merck’s 2013 decision to withdraw the niacin-laropiprant product from the global market made it difficult for researchers to initiate further clinical investigation on niacin’s novel effects. Subsequently, the combination product failure also overshadowed the drug repositioning prospects of niacin in the treatment of hyperhosphatemia in ESRD patients. Under these circumstances, it is deemed important and timely to provide for the clinical world an updated, comprehensive review of new research findings regarding niacin’s hypophosphatemic effects and provide suggestions for future studies.
Preliminary clinical trials demonstrated that niacin has the potential to be used as a cost-effective, alternative or adjunctive phosphorus-lowering treatment in dialysis patients.Citation12–Citation15 The availability of numerous generic formulations makes it more attractive to patients because they would prefer an inexpensive treatment option as a life-long therapy over patented phosphate binders such as sevelamer carbonate. In addition, with its well-documented, additive effects on lipid profile, chronic renal disease patients particularly with cardiovascular comorbidities can expect synergistic cardioprotective benefits from niacin therapy.Citation29–Citation31 Other advantages include its flexible once- or twice-daily dosing regimen as opposed to the dosing schedule of traditional phosphate binders typically given three times daily with meals. This will significantly improve patient convenience as well as compliance with therapy while decreasing daily pill burden.
Finding ways to overcome side effects contributable to niacin is a prerequisite for successfully identifying and developing the new indication for the vitamin. Niacin-induced facial flushing is rarely severe enough to lead patients to discontinue therapy, but it is the major cause of patient discomfort. Initiation at a low dose with slow titration and pretreatment with aspirin can attenuate the incidence and severity of the cutaneous side effect.Citation32 Additionally, selecting the extended-release (ER) formulation can help. Niacin is metabolized in the liver by either a conjugation or amidation pathway. The metabolite produced via the amidation pathway, nicotinamide, is mainly associated with GI symptoms and hepatotoxicity. Amidation is categorized as a high-affinity and low-capacity pathway.Citation22 Therefore, if niacin exists in low concentrations over time, such as with a sustained release formulation, amidation becomes a predominant metabolic pathway and produces more nicotinamide as a result.Citation33 In contrast, immediate-release niacin is likely to quickly saturate the low-capacity amidation pathway, shifting hepatic metabolism to conjugation. This will lead to greater production of nicotinuric acid and subsequent prostaglandin, resulting in more episodes of flushing. With its moderately slow metabolic rate, the ER formulation appears to be associated with the least incidence of flushing, GI symptoms, and hepatotoxicity.Citation22
Despite promising results from previous trials worldwide, niacin’s efficacy and safety data compared with the gold standard phosphate binder is very limited, and its clinical dosage has not yet been clearly defined. The only head-to-head trial thus far is the 2012 study by Ahmadi et al.Citation28 The research had several limitations in terms of sample size, subtherapeutic dose with no titration, treatment duration, comparator salt form, and confounder control. A dose-finding study (NCT01200784) in over 250 hemodialysis patients has been completed in July 2011, but the results remain unpublished. As a result, the optimal dosing strategy for niacin remains uncertain.
Further large-scale, randomized-controlled, comparative trials are required to clarify the uncertainties faced by providers in clinical practice regarding the use of niacin as monotherapy or add-on therapy for hyperphosphatemia in dialysis patients. Following are suggestions for future studies. As it is unclear whether nicotinamide has equivalent effects on lipid parameters, niacin is recommended to be chosen as a study drug to ensure the synergistic antilipemic effects. Based on previous studies, the intervention dosage ranged from 375 to 1,500 mg/day, with the average daily dose of approximately 1,000 to 1,500 mg. The usual dose of niacin ER for dyslipidemia control, 1,000–2,000 g/day, is similar to the estimated dose for hyperphosphatemia treatment. Researchers, therefore, may start low and titrate up the niacin dosage to the goal daily dose of approximately 1,000–1,500 mg. Recruiting patients with a higher phosphorus level at baseline may help researchers to readily identify the significance of hypophosphatemic effects of interventions.Citation34 To evaluate the sustainability of niacin’s therapeutic effects, long-term follow-up of patients is recommended. Lastly, potential confounders, such as dietary phosphorus intake, other phosphate binder use, and concurrent statin therapy, are required to be adequately controlled.
Conclusion
Niacin can be a patient-convenient and inexpensive alternative or add-on therapy for phosphorus management in dialysis patients. With its additive antilipemic effects, it can also provide synergistic benefits for chronic renal disease patients with cardiovascular comorbidities. Further well-designed, large-scale, long-term, comparative trials are needed to successfully repurpose niacin for the new indication.
Acknowledgments
This study was supported by the new faculty research fund of Ajou University and the Bio and Medical Technology Development Program of the National Research Foundation funded by the Ministry of Science, Information and Communications Technology, and Future Planning, Republic of Korea (No. 2013M3A9B5075838).
Disclosure
The authors declare that there is no conflict of interests regarding the publication of this article.
References
- TonelliMPannuNMannsBOral phosphate binders in patients with kidney failureN Engl J Med2010362141312132420375408
- FriedmanEAConsequences and management of hyperphosphatemia in patients with renal insufficiencyKidney Int Suppl200595S1S715882307
- LopesAATongLThummaJPhosphate binder use and mortality among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS): evaluation of possible confounding by nutritional statusAm J Kidney Dis20126019010122385781
- KestenbaumBSampsonJNRudserKDSerum phosphate levels and mortality risk among people with chronic kidney diseaseJ Am Soc Nephrol200516252052815615819
- KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD)Kidney Int Suppl2009113S1S130
- HruskaKAMathewSLundRQiuPPrattRHyperphosphatemia of chronic kidney diseaseKidney Int200874214815718449174
- LiuLWangYChenHZhuXZhouLYangYThe effects of non-calcium-based phosphate binders versus calcium-based phosphate binders on cardiovascular calcification and bone remodeling among dialysis patients: a meta-analysis of randomized trialsRen Fail201419
- GoodmanWGVascular calcification in chronic renal failureLancet200135892881115111611597661
- MallucheHHAluminium and bone disease in chronic renal failureNephrol Dial Transplant200217Suppl 2212411904354
- ChertowGMBurkeSKRaggiPTreat to Goal Working GroupSevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patientsKidney Int200262124525212081584
- OkaYMiyazakiMMatsudaHSevelamer hydrochloride dose-dependent increase in prevalence of severe acidosis in hemodialysis patients: analysis of nationwide statistical survey in JapanTher Apher Dial2014181374324499082
- TakahashiYTanakaANakamuraTNicotinamide suppresses hyperphosphatemia in hemodialysis patientsKidney Int20046531099110414871431
- SampathkumarKSelvamMSoorajYSGowthamanSAjeshkumarRNExtended release nicotinic acid – a novel oral agent for phosphate controlInt Urol Nephrol200638117117416502077
- MullerDMehlingHOttoBNiacin lowers serum phosphate and increases HDL cholesterol in dialysis patientsClin J Am Soc Nephrol2007261249125417913971
- Restrepo ValenciaCACruzJSafety and effectiveness of nicotinic acid in the management of patients with chronic renal disease and hyperlipidemia associated to hyperphosphatemiaNefrologia20082816166 Spanish18336133
- KataiKTanakaHTatsumiSNicotinamide inhibits sodium-dependent phosphate cotransport activity in rat small intestineNephrol Dial Transplant19991451195120110344361
- EtoNMiyataYOhnoHYamashitaTNicotinamide prevents the development of hyperphosphataemia by suppressing intestinal sodium-dependent phosphate transporter in rats with adenine-induced renal failureNephrol Dial Transplant20052071378138415870221
- AramwitPSrisawadwongRSupasyndhOEffectiveness and safety of extended-release nicotinic acid for reducing serum phosphorus in hemodialysis patientsJ Nephrol201225335436221748722
- TothPPHigh-density lipoprotein and cardiovascular riskCirculation2004109151809181215096460
- YusufSHawkenSOunpuuSEffect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control studyLancet2004364943893795215364185
- BarterPGottoAMLaRosaJCHDL cholesterol, very low levels of LDL cholesterol, and cardiovascular eventsN Engl J Med2007357131301131017898099
- PieperJAOverview of niacin formulations: differences in pharmacokinetics, efficacy, and safetyAm J Health Syst Pharm20036013 Suppl 2S9S14 quiz S2512901025
- Group HTCLandrayMJHaynesREffects of extended-release niacin with laropiprant in high-risk patientsN Engl J Med2014371320321225014686
- ChengSCYoungDOHuangYDelmezJACoyneDWA randomized, double-blind, placebo-controlled trial of niacinamide for reduction of phosphorus in hemodialysis patientsClin J Am Soc Nephrol2008341131113818385391
- YoungDOChengSCDelmezJACoyneDWThe effect of oral niacinamide on plasma phosphorus levels in peritoneal dialysis patientsPerit Dial Int200929556256719776051
- ShahbazianHZafar MohtashamiAGhorbaniAOral nicotinamide reduces serum phosphorus, increases HDL, and induces thrombocytopenia in hemodialysis patients: a double-blind randomized clinical trialNefrologia2011311586521270914
- Edalat-NejadMZameniFTalaieiAThe effect of niacin on serum phosphorus levels in dialysis patientsIndian J Nephrol201222317417823087550
- AhmadiFShamekhiFLessan-PezeshkiMKhatamiMRComparison of efficacy of the phosphate binders nicotinic acid and sevelamer hydrochloride in hemodialysis patientsSaudi J Kidney Dis Transpl201223593493822982903
- CannerPLBergeKGWengerNKFifteen year mortality in Coronary Drug Project patients: long-term benefit with niacinJ Am Coll Cardiol198686124512553782631
- Clofibrate and niacin in coronary heart diseaseJAMA197523143603811088963
- RubinsHBRobinsSJCollinsDGemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial Study GroupN Engl J Med1999341641041810438259
- KamannaVSGanjiSHKashyapMLThe mechanism and mitigation of niacin-induced flushingInt J Clin Pract20096391369137719691622
- DaltonTABerryRSHepatotoxicity associated with sustained-release niacinAm J Med19929311021041626557
- RennickAKalakecheRSeelLSheplerBNicotinic acid and nicotinamide: a review of their use for hyperphosphatemia in dialysis patientsPharmacotherapy201333668369023526664