Abstract
With an estimated prevalence of 5.8 million in the USA and over 23 million people worldwide, heart failure (HF) is growing in epidemic proportions. Despite the use of guideline-directed medical therapies such as angiotensin-converting enzyme inhibitors, beta-adrenergic blockers, angiotensin receptor blockers, and mineralocorticoid receptor antagonists for chronic systolic HF for almost two decades, HF remains a leading cause of morbidity, mortality, and health care expenditures. The Prospective Comparison of Angiotensin Receptor-Neprilysin Inhibitor with Angiotensin-Converting Enzyme Inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure (PARADIGM-HF) trial provided compelling evidence for the cardiovascular and mortality benefit of sacubitril/valsartan when compared to enalapril in patients with heart failure and reduced ejection fraction (HFrEF). Sacubitril/valsartan performed better than enalapril across various HFrEF patient characteristics and showed substantial benefit in patients with other common comorbidities. Following the trial, the US Food and Drug Administration approved this drug for the treatment of HF. Various international HF consensus guidelines endorse sacubitril/valsartan as a class I recommendation for the management of symptomatic HFrEF. Although this high-quality clinical study is the largest and the most globally represented trial in HFrEF patients, concerns have been raised regarding the generalizability of the trial results in real-world HF population. The gaps in US Food and Drug Administration labeling and guideline recommendations might lead to this medication being used in a larger population than it was studied in. In this review, we will discuss the current role of sacubitril/valsartan in the management of HF, concerns related to PARADIGM-HF and answers, shortcomings of this novel drug, effects on patient characteristics, real-world eligibility, and the role of ongoing and further investigations to clarify the profile of sacubitril/valsartan in the management of HF.
Introduction
Heart failure (HF) is associated with significant morbidity, mortality, and health care expenditure. HF is classified based on left ventricular ejection fraction (LVEF) into HF with reduced EF (HFrEF) with an LVEF <40% and HF with preserved EF (HFpEF) with an LVEF ≥50%.Citation1 An EF between 40% and 49% is considered an intermediate zone and is termed as HF with borderline EF or HF with mid-range EF. Epidemiologic data indicate that HFpEF and HFrEF contribute equally to the total HF population.Citation1 HFpEF patients have a similar post-discharge mortality risk and equally high rates of rehospitalization, compared to patients with HFrEF.Citation2 With an estimated prevalence of 5.8 million in the USA and over 23 million people worldwide, HF is growing in epidemic proportions.Citation3 The cost of HF in the USA was around $30 billion in 2012, a number that is projected to increase to around $70 billion by the year 2030.Citation4
Acute decompensated HF (ADHF) is the clinical syndrome of new onset or worsening HF symptoms and signs requiring urgent treatment.Citation5 In the USA, ADHF exacerbations result in around one million hospitalizations yearly and contribute largely to the overall HF health care expenditure.Citation4 Hospitalization for ADHF serves as a poor prognostic indicator with ~30% and 50% readmission rates at 1 and 6 months, respectively, and a 1-year all-cause mortality as high as 30%.Citation6,Citation7 The estimated survival rate after the diagnosis of HF is 50% at 5 years and 10% at 10 years.Citation8 Despite the use of guideline-directed medical therapies such as angiotensin-converting enzyme inhibitors (ACEIs), beta-adrenergic blockers, angiotensin receptor blockers (ARBs), and mineralocorticoid receptor antagonists (MRAs) as cornerstone medical therapies for chronic systolic HF for almost two decades, HF remains a leading cause of morbidity, mortality, and health care expenditures in the USA and worldwide.
Advances in our understanding of the renin–angiotensin–aldosterone (RAAS) pathway and natriuretic peptide system, lessons learned from randomized trials of natriuretic peptide system augmentation, and pharmaco-innovation led to the creation and validation of combination sacubitril/valsartan (Entresto™ [LCZ696]; Novartis) for the treatment of HFrEF. The Prospective Comparison of Angiotensin Receptor-Neprilysin Inhibitor with Angiotensin-Converting Enzyme Inhibitor to Determine Impact on Global Mortality and Morbidity in Heart Failure (PARADIGM-HF) trial provided compelling evidence for the cardiovascular (CV) and mortality benefit of sacubitril/valsartan when compared to enalapril (an ACEI) in patients with HFrEF.Citation9 Numerous post hoc analyses of the original trial extended the benefits of this innovative medication across a multitude of clinical characteristics.Citation10 Following the trial, the US Food and Drug Administration (FDA) approved this drug for the treatment of HF. International HF consensus guidelines now endorse sacubitril/valsartan as a class I recommendation for the management of HFrEF.Citation11–Citation13 In this review, we will discuss the current role of sacubitril/valsartan in the management of HF, shortcomings of this novel drug, effects on patient characteristics, real-world eligibility, and the role of ongoing and further investigations to clarify the profile of sacubitril/valsartan in the management of HF.
The PARADIGM-HF trial
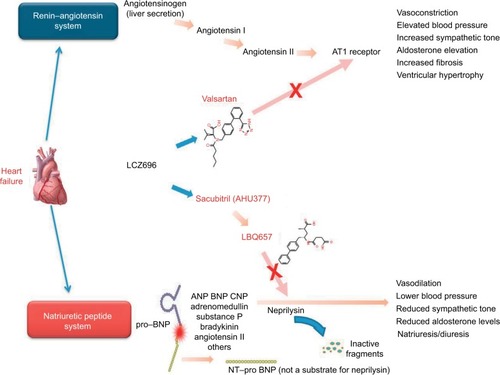
LCZ696 is a novel, orally active, first-in-class angiotensin receptor-neprilysin inhibitor (ARNI), which is a 1:1 combination of valsartan (an ARB) and the neprilysin inhibitor (NEPI) sacubitril.Citation14 Sacubitril (AHU377) is a prodrug, which upon ingestion is rapidly metabolized to an active NEPI moiety LBQ657.Citation14 The mechanism of action and the effects of LCZ696 on the CV system in HF are explained in .Citation15 Preclinical trials of this combination provided evidence for simultaneous neprilysin inhibition and angiotensin receptor blockade.Citation10 Favorable safety and efficacy data of this combination from a Phase III randomized controlled trial in hypertensive HFpEF patients paved the way for the larger PARADIGM-HF trial.Citation9
Figure 1 Mechanism of action of sacubitril/valsartan in heart failure.
Abbreviations: ANP, atrial natriuretic peptide; AT1, angiotensin type I; BNP, brain (or B-type) natriuretic peptide; CNP, C-type natriuretic peptide; NT-proBNP, N-terminal pro-BNP.
The PARADIGM-HF was a Phase III double-blind controlled trial that randomized 8,442 patients with New York Heart Association (NYHA) class II–IV HF and an LVEF of ≤40% (later amended to ≤35%) to receive twice daily dosing of either 200 mg of LCZ696 or 10 mg of enalapril in addition to standard medical therapy for HF ().Citation9 Patients were eligible for the study if they had elevated plasma B-type natriuretic peptide (BNP) level ≥150 pg/mL (or ≥100 pg/mL if hospitalized for HF in previous 12 months) or elevated N-terminal pro-BNP (NT-proBNP) level ≥600 pg/mL (or ≥400 pg/mL if hospitalized for HF in previous 12 months). At 27-month follow-up, LCZ696 was associated with a 20% decrease in the composite primary endpoint of death from CV causes or hospitalization for HF, compared to enalapril. Additionally, LCZ696 reduced death from any CV cause by 20%, first hospitalization for worsening HF by 21%, all-cause mortality by 16%, and improved the symptoms and quality of life as measured on the Kansas City Cardiomyopathy Questionnaire ().Citation9,Citation16 Numerous post hoc analyses have demonstrated the superiority of sacubitril/valsartan over enalapril, irrespective of age, systolic blood pressure (SBP), LVEF, baseline HF risk scores, and glycemic status.Citation10
Table 1 The PARADIGM-HF trialCitation9,Citation16
LCZ696 exhibited additional clinical benefit over enalapril in HF patients by attenuating progression of the HF disease process. Fewer LCZ696-treated patients required intensification of medical treatment for HF or an emergency department visit for worsening HF.Citation17 Patients in the LCZ696 group had 23% fewer hospitalizations for worsening HF evident within the first 30 days of randomization and were less likely to have implantation of an HF device or cardiac transplantation.Citation17 Patients taking sacubitril/valsartan had early and sustained reduction in biomarkers of myocardial wall stress and injury (NT-proBNP and troponin) and increased plasma BNP levels versus enala-pril.Citation17 Putative placebo analysis of LCZ696 using results from previous landmark placebo-controlled trials of RAAS blockade in HF showed significantly greater reductions in CV death, HF hospitalization, and all-cause mortality with LCZ696.Citation18 Findings from the PARADIGM-HF trial and subsequent secondary analyses incited a lot of excitement in the HF community, as the discovery of sacubitril/valsartan proves momentous in the relatively stagnant field of HF pharmacotherapy.
International consensus recommendation for sacubitril/valsartan in HF
Following the trial, the USA FDA reviewed LCZ696 under its priority review program with a fast-track designation and approved this drug for the treatment of all NYHA II–IV HFrEF patients in July 2015.Citation19 The USA FDA labeling is overarching, recommending the medication for all NYHA function class II–IV HFrEF patients with serum potassium ≤5.2 mmol/L, and no contraindication or intolerance to ACEI/ARB. The same year, the European Medical Agency approved the use of sacubitril/valsartan in adult patients for treatment of symptomatic chronic HFrEF.Citation20
In their 2016 focused update on HF guidelines, the American College of Cardiology, the American Heart Association, and the Heart Failure Society of America recommended replacing an ACEI or ARB with an ARNI in patients with chronic symptomatic HFrEF, NYHA class II or III, currently tolerating an ACEI or ARB, to further reduce morbidity and mortality (class I recommendation).Citation11 The guideline also recommended against concomitant use of ARNI with ACEI or within 36 hours of last ACEI dose, as it can precipitate angioedema (class III recommendation).Citation11
The Canadian Cardiovascular Society was the first to incorporate the use of sacubitril/valsartan in HF patients.Citation12 In their 2014 update on Heart Failure Management Guidelines, the Canadian guidelines recommend the use of LCZ696 in place of an ACEI or an ARB in patients with mild to moderate HF, LVEF <40%, an elevated natriuretic peptide level or hospitalization for HF in the past 12 months, a serum potassium <5.2 mmol/L, an estimated glomerular filtration rate (eGFR) ≥30 mL/min, and treated with appropriate doses of guideline-directed medical therapy, with close surveillance of serum potassium and creatinine (Conditional Recommendation; High-Quality Evidence).Citation12 The Canadian HF guidelines limit the use of ARNI in patients who met the PARADIGM trial entry criteria.
The 2016 European Society of Cardiology (ESC) HF guidelines recommend the use of sacubitril/valsartan as an ACEI replacement to further reduce the risk of death and HF hospitalization in ambulatory patients with HFrEF (LVEF <35%) who remain symptomatic despite optimal treatment with ACEI, a beta-blocker, and an MRA (class IB recommendation).Citation13 In contrast to the American College of Cardiology, the American Heart Association, and the Heart Failure Society of America HF guidelines, the ESC guidelines specify having an LVEF cutoff of 35% prior to initiation of sacubitril/valsartan. The ESC guidelines also require the patient to be tried on an MRA before initiating an ARNI.
Concerns with PARADIGM-HF and answers
Current recommendations for the use of sacubitril/valsartan in HFrEF patients are based on the results of one trial, the PARADIGM-HF. Although this study is the largest and a globally represented high-quality clinical trial in HFrEF patients that evaluated key outcomes, it is not exempt from criticism. Since the publication of the original trial results in 2014, several physicians and researchers have raised apprehensions regarding the generalizability of the trial results with regards to the study design, the effect of target medication doses achieved on clinical outcomes, study population representativeness of the real-world HFrEF patients, and the effect of ethnic and geographic variations on outcomes.Citation16
PARADIGM-HF was initiated without a Phase II safety trial, and hence, the investigators employed steps to test the tolerability of LCZ696 before randomization with a run-in phase for enalapril and then for LCZ696.Citation10 More than 10% of the original study population dropped out during the LCZ696 run-in phase.Citation9 Concern existed regarding randomizing only the patients who tolerated LCZ696 during the run-in phase of the trial, as such a design can exclude patients who are intolerant to the drug and can affect study outcomes and external validity. However, a post hoc analysis of the trial data showed that run-in noncompletion did not affect the magnitude of the treatment benefit of LCZ696 over enalapril.Citation21,Citation22 Low blood pressure, low eGFR, and more advanced HF (higher NTproBNP level) were associated with higher risk for run-in noncompletion, suggesting that these patients should undergo closer monitoring during the uptitration of LCZ696 or the conversion of patients from enalapril to LCZ696.Citation21,Citation22
The mean target dose achieved for enalapril (18.9 mg/day) was lower than the maximum recommended dose in HF, whereas the maximum recommended target dose was achieved for sacubitril/valsartan.Citation16 This raises the concern as to whether the maximal dose of valsartan produced more RAAS blockade leading to better clinical outcomes when compared to a moderate dose of enalapril, as no trials showed head-to-head comparison of the study doses of valsartan and enalapril as used in the PARADIGM-HF.Citation16 The mean target dose for enalapril achieved in most placebo-controlled landmark HF trials providing significant CV benefit was also <20 mg/day (16.6 mg/day in the Studies of Left Ventricular Dysfunction and 18.4 mg/day in the Cooperative North Scandinavian Enalapril Survival Study).Citation21 It is important to note that in routine clinical practice, <30% HF patients achieved the target dose of enalapril due to complications including hypotension and hyperkalemia.Citation21 Although LCZ696-treated patients had greater risk of developing symptomatic hypotension (14% versus 9%, p<0.001; ), it did not result in significantly more medication discontinuation than enalapril patients, suggesting better tolerance with LCZ696.Citation9,Citation21
Black patients have been less represented in HF trials, although they have poorer outcomes. The lower proportion of black patients in the PARADIGM-HF trial (5%) may have limited the ability of this trial to detect a significant difference in the frequency of angioedema with LCZ696.Citation16 This is particularly concerning, as black patients had significantly more instances of angioedema compared to enalapril in the Omapatrilat Cardiovascular Treatment versus Enalapril trial.Citation16 Future studies should shed light on this association.
Profile of sacubitril/valsartan in HF and patient selection perspectives
In this section, we will discuss the profile of sacubitril/valsartan in HF with regards to patient characteristics and future perspectives for its use, with a mention of currently undergoing clinical trials. Registry data on HFrEF patients from Acute Decompensated Heart Failure National Registry (ADHERE) and Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure (OPTIMIZE-HF) were used to provide comparisons with PARADIGM-HF patient population in available baseline demographic characters ().Citation9,Citation23,Citation24
Table 2 Baseline patient characteristics in various reduced ejection fraction heart failure patient study groups
OPTIMIZE-HF is a large US national registry and performance improvement program for patients hospitalized for HF.Citation23 ADHERE is a large multicenter registry designed to compile a large clinical database on the clinical characteristics, management, and outcomes of patients hospitalized for HF across the USA.Citation24 When compared to the HFrEF population in these registries, the PARADIGM-HF study population is relatively younger and male dominant. Additionally, the population has less black subjects, higher mean LVEF, lower SBP at randomization, excluded chronic kidney disease (CKD) stage 4 and 5 (eGFR <30 mL/min/1.73 m2) patients, and most patients in NYHA functional class II, with almost no NYHA class IV patients. ADHERE and OPTIMIZE-HF represent real-world US HF patients; hence, these differences in patient characteristics have the potential to affect clinical outcomes in real-world HFrEF patients.
Age
Similar to the real-world HF population, mortality and HF hospitalization rate increased with age in PARADIGM-HF.Citation9 The median patient age in the trial was 63.8 years, which is lower than the real-world HFrEF population and those in ADHERE (mean 70 years) and OPTIMIZE-HF (mean 70 years) registry ().Citation9,Citation23,Citation24 This difference could have important clinical considerations with regards to better outcomes noticed in this relatively younger ambulatory HFrEF cohort. It is interesting to note that the clinical benefit observed in the sacubitril/valsartan group was consistent across prespecified age groups including patients <55 and >75 years, when compared to enalapril.Citation25 HF is a progressive disease and advances in severity with age, so initiation of sacubitril/valsartan at a younger age in HFrEF patients who have a less-advanced disease stage will provide more clinical and survival benefit.
Sex
The study population in PARADIGM-HF is predominantly male (78%) with a rate higher than that observed for HFrEF patients in the ADHERE (60%) and OPTIMIZE-HF registries (62%) ().Citation9 This proportion is higher when compared to real-world HF patients in whom HFrEF is almost equally prevalent sex-wise. However, in prespecified subgroup analysis of the PARADIGM-HF, the clinical benefit of sacubitril/valsartan was not affected by sex.Citation9 ARNI can be used without reservation in HFrEF patients of either sex.
Race/ethnicity
As mentioned earlier, caution should be exercised when prescribing ARNI to black HFrEF patients, as available safety data about angioedema is limited in this underrepresented population in the PARADIGM-HF.Citation9,Citation16 The prospective comparison of ARNI with ACE inhibitor to determine the novel beneficial treatment value in Japanese HF patients (PARALLEL-HF) trial is now being conducted to assess the safety and efficacy of sacubitril–valsartan in Japanese HFrEF population. This is a multicenter, randomized, double-blind study with similar design, phases, inclusion and exclusion criteria as in PARADIGM-HF trial ().Citation26
Table 3 Currently undergoing trails of sacubitril/valsartan which will answer important clinical questions
Regional demographic variations
Significant regional differences in baseline demographics such as age, symptoms, comorbidities, background therapies, and event rates between patients enrolled from different geographic locations exist in the PARADIGM-HF cohort.Citation27 A post hoc analysis of the original trial demonstrated a consistent clinical benefit of sacubitril/valsartan across geographic regions, despite having significant baseline regional demographic variations.Citation27 These findings are encouraging for the global use of this novel pharmacotherapy in HFrEF patients to provide reduction in HF morbidity and mortality across the world.
NYHA functional class
Majority of the study population in the PARADIGM-HF consisted of NYHA class II patients (70%).Citation9 A nominally significant interaction between NYHA class at randomization and the effect of treatment was seen for the primary endpoint (better outcomes with NYHA class I–II; p=0.03; without adjustment for multiple comparisons), but not for the interaction between NYHA class and the effect on death from CV causes (p=0.76).Citation9 Although the interaction is nominal, it confers a greater CV benefit to sacubitril/valsartan when initiated early in the course of HFrEF. With almost 75% patients in the trial classified as either NYHA class I or II, the power of this group to identify an interaction if present may be increased. Nevertheless, initiation of sacubitril/valsartan early in the disease course of HFrEF is encouraged.
Type of HF
Sacubitril/valsartan is currently approved for use in chronic HFrEF patients. Having demonstrated safety in HFpEF population and efficacy in hypertensive patients in earlier trials, sacubitril/valsartan has the potential to show substantial clinical benefit in the HFpEF population, since hypertension is an important risk factor for HFpEF. The Phase III, randomized controlled, Prospective comparison of Angiotensin Receptor-neprilysin inhibitor with ARB Global Outcomes in HF with preserved ejection fraction (PARAGON-HF) trial is evaluating the effects of sacubitril/valsartan versus valsartan on the primary composite outcome of CV death and HF hospitalization in HFpEF patients and is expected to be completed in 2019 ().Citation28 The PARAGON-HF will also compare treatment benefit of sacubitril/valsartan versus valsartan on functional class, change in Kansas City Cardiomyopathy Questionnaire score, and time to deterioration in renal function.Citation28 The randomized, double-blind controlled study comparing LCZ696 to medical therapy for comorbidities in HFpEF patients (PARALLAX) is a 24-week, multicenter, parallel-group, active controlled study which will evaluate the effect of sacubitril/valsartan on NT-proBNP levels, symptoms, exercise function, and safety, compared to individualized medical management of comorbidities (with enalapril, valsartan, or placebo) in HFpEF patients ().Citation29
Etiology of HF
HFrEF has different etiologies depending on age, sex, geography, and race. Clinical outcomes and response to medical therapies in HFrEF patients will vary depending on etiology. In the PARADIGM-HF trial, 60% of the study population had ischemic cardiomyopathy (ICM), which is comparable to that observed in HFrEF patients in the ADHERE and the OPTIMIZE-HF registries ().Citation9,Citation23,Citation24 This raises concern of the benefit of sacubitril/valsartan in patients with non-ICM (NICM). A post hoc analysis of the PARADIGM-HF classified the study population based on etiology of HF into patients with ICM (60%) and NICM (40%).Citation30 NICM consisted of idiopathic HF (19%), hypertensive HF (11.5%), and other causes of HF (9.5%).Citation30 The investigators noted that patients with NICM were younger, more likely female, and had higher NT-proBNP levels than those with ICM.Citation30 With regards to primary composite endpoint and CV death, the benefit of sacubitril/valsartan over enalapril was consistent across the different etiology subgroups.Citation30 The authors concluded that sacubitril/valsartan is effective in both ICM and NICM including idiopathic and hypertensive causes of NICM. These findings have important considerations when using this ARNI in real-world HFrEF patients and suggest that the complex pathophysiologic interactions of ARNI with the RAAS are independent of the type of insult resulting in HF.
Left ventricular ejection fraction
In the PARADIGM-HF trial, the risk of all clinical outcomes increased with decreasing LVEF (mean 29.5%), and LVEF was noted to be a strong predictor of outcomes.Citation9 In a post hoc analysis, sacubitril/valsartan was effective across the LVEF spectrum and there was no evidence of heterogeneity for the primary endpoint, CV death, HF hospitalization, or all-cause mortality.Citation31 These findings suggest that the benefit of sacubitril/valsartan is not LVEF dependent and may have implications in its testing in HFpEF patients.
Intracardiac devices
Patients with cardiac devices were underrepresented in the PARADIGM-HF trial. Around 15% had implantable cardioverter-defibrillator and around 7% patients had cardiac resynchronization therapy.Citation9 Despite this limitation, the magnitude of clinical benefit of sacubitril/valsartan on sudden death did not differ in patients with or without an implantable cardioverter-defibrillator.Citation32 ARNI use will provide additional CV and survival benefit in symptomatic HFrEF patients, irrespective of them having an intracardiac device.
ADHF and post-acute myocardial infarction patients
PARADIGM-HF excluded patients who had an acute coronary event within the last 3 months of randomization.Citation9 The benefit of initiating or uptitrating neurohormonal antagonist during an episode of ADHF is not clear.Citation33 However, it is well known that initiation of beta-blocker, ACEI, and an MRA after acute myocardial infarction (MI) with associated left ventricle systolic dysfunction reduces the rate of hospitalization for HF and mortality.Citation34–Citation36 In a post hoc analysis of the PARADIGM-HF trial, the benefit of sacubitril–valsartan in reducing CV mortality or hospitalization for HF was consistent in all patient subgroups, with no significant difference in patients with no prior HF hospitalization compared to those with recent HF hospitalization (<3 months from randomization).Citation37
Although available data do not support the use of this ARNI in ADHF patients and in post-acute MI patients, ongoing trials will shed more light. Comparison of Sacubitril/Valsartan versus Enalapril on Effect on NT-proBNP in Patients Stabilized from an Acute Heart Failure Episode (PIONEER-HF) is a multicenter, randomized, double-blind, 8-week study, with the aim being to evaluate the effect of sacubitril–valsartan versus enalapril on changes in NT-proBNP in HFrEF patients who have been stabilized following hospitalization for ADHF. The primary outcome is the percentage change in NT-proBNP from baseline to weeks 4 and 8 ().Citation38
The Comparison of Pre- and Post-discharge Initiation of LCZ696 Therapy in HFrEF Patients After an Acute Decompensation Event (TRANSITION) trial is a multicenter, randomized, open-label study, with an estimated enrollment of 1,000 patients, aiming to compare the initiation of sacubitril/valsartan after stabilization of patients with ADHF at any point prior to discharge with post-discharge initiation (up to 14 days). The primary outcome is the percentage of patients who are receiving sacubitril/valsartan 200 mg twice daily at 10 weeks after randomization ().Citation39 This trial will also evaluate the safety of initiation of sacubitril/valsartan in ADHF and the percentage of patients who permanently discontinued from treatment due to adverse events.Citation39
The Prospective ARNI versus ACE Inhibitor Trial to DetermIne Superiority in Reducing Heart Failure Events After MI (PARADISE-MI) trial is a Phase III, randomized controlled study conducted in post-acute MI patients without prior chronic HF, with LVEF<40%, and/or pulmonary congestion at the time of randomization. The PARADISE-MI trial will evaluate the benefit of sacubitril/valsartan versus ramipril in reducing the occurrence of the primary composite endpoint of CV death, HF hospitalization, and outpatient HF (time-to-first event analysis), as shown in .Citation40
CKD and hyperkalemia
HFrEF patients frequently have CKD with varying degrees of eGFRs. Worsening renal function and hyperkalemia can limit the successful use or uptitration of RAAS blockade agents in HF patients.Citation41 The PARADIGM-HF trial excluded patients with eGFR<30 mL/min/1.73 m2, thereby limiting safety data on its use in CKD stage 4 and 5 patients. Interestingly, it was observed that LCZ696-treated patients had significantly less instances of elevated serum creatinine ≥2.5 mg/dL (3.3% in the LCZ696 group versus 4.5% in the enalapril group, p=0.007) compared to enalapril-treated patients. The UK Heart and Renal Protection III (UK HARP-III) trial will compare LCZ696 against irbesartan (an ARB) in patients with proteinuric CKD (eGFR 20–60 mL/min/1.73 m2) to assess the short-term safety and efficacy of LCZ696 in this population with respect to changes in eGFR ().Citation42 If the results from the UK HARP-III trial favor LCZ696, longer duration studies to evaluate the effects of LCZ696 in delaying the progression of CKD to end-stage renal disease should be planned.
With regards to severe hyperkalemia, LCZ696-treated patients had lower instances of elevated serum potassium >6 mmol/L (4.3% in the LCZ696 group versus 5.6% in the enalapril group, p=0.007; ).Citation9 Moreover, among patients treated with an MRA, severe hyperkalemia was more likely with enalapril treatment than with LCZ696 (3.1 versus 2.2 per 100 patient-years, p=0.02), suggesting that LCZ696 might decrease the risk of hyperkalemia compared to enalapril, when added to MRA therapy in patients with HFrEF.Citation43 Although further safety data will be available from currently ongoing trials, sacubitril/valsartan therapy might facilitate the uptitration of other RAAS blocking agents with proven mortality benefit in HFrEF patients without increasing the incidence of dose-limiting adverse events.
Diabetes mellitus
In the PARADIGM-HF trial, it was observed that patients with diabetes and pre-diabetes had a higher risk of the primary composite outcome.Citation9 Sacubitril/valsartan reduced the risk of CV death and HF hospitalizations compared with enalapril, irrespective of the glycemic status.Citation44 A recently published post hoc analysis of the PARADIGM-HF trial found that sacubitril/valsartan decreased hemoglobin A1C levels by 0.26% during the first year of follow-up, compared to a 0.16% reduction with enalapril (p=0.0023).Citation45 Over 3 years, HbA1c levels remained persistently lower in patients treated with sacubitril/valsartan compared to enalapril, with an overall reduction of 0.14% (95% CI: 0.06–0.23, p=0.0055).Citation45 In addition, 29% fewer sacubitril/valsartan-treated patients initiated insulin therapy to achieve glycemic control (7% versus 10% patients, hazard ratio 0.71, 95% CI: 0.56–0.90; p=0.0052).Citation45 These results are interesting as they hypothesize an additional metabolic benefit and emphasize the extracardiac pleiotropic effects of sacubitril/valsartan in HFrEF patients in addition to its compelling CV efficacy.
Eligibility of the real-world HF patients for sacubitril/valsartan use
The US FDA labeling for sacubitril/valsartan is very broad, recommending this medication for all NYHA function class II–IV HFrEF patients with serum potassium ≤5.2 mmol/L and no contraindication or intolerance to ACEI/ARB.Citation19 Differences exist between international consensus guidelines for ARNI indications in HFrEF, which might affect real-world patient groups who will be prescribed this drug. Also, concerns exist regarding the generalizability of the results of PARADIGM-HF to the entire real-world HFrEF patients, as the PARADIGM-HF study population represents only a minority of the real-world HFrEF population. Several researchers investigated the differences in eligibility of sacubitril/valsartan initiation in the real-world HFrEF population based on FDA labeling versus PARADIGM-HF enrollment criteria.
Parikh et al evaluated patient population from the Get With The Guidelines-Heart Failure (GWTG-HF) registry to characterize patients’ eligibility and potential barriers for sacubitril/valsartan initiation according to the criteria set forth in FDA labeling and PARADIGM-HF.Citation46 The GWTG-HF registry is composed of patients who were admitted for worsening HF or developed significant HF symptoms during a hospitalization.Citation46 Among 28,932 hospitalizations of HFrEF patients, 20,083 (69%) patients were eligible for sacubitril/valsartan initiation based on FDA labeling and 11,018 (38%) based on PARADIGM-HF criteria (including natriuretic peptide cutoffs), as shown in .Citation46 Of the 20,083 who were eligible based on FDA criteria, only 55% would have been eligible for sacubitril/valsartan initiation based on PARADIGM-HF criteria. Based on ESC guidelines, this number would go down further, as only 41% patients in the PARADIGM-HF eligible group were on an MRA. The most common reasons for ineligibility (using PARADIGM-HF criteria) were: LVEF >35%, discharge SBP <100 mmHg, and not being on ACEI/ARB therapy.Citation21 Patients eligible for sacubitril/valsartan based on PARADIGM-HF criteria had significantly lower 30-day and 1-year mortality rates, compared to those who were excluded based on FDA-labeling or PARADIGM-HF entry criteria.Citation46
Table 4 Studies evaluating the real-world eligibility of sacubitril/valsartan in HFrEF patients
Perez et al performed a single-center chart review of 210 NYHA class II–IV patients admitted to their HF service and had post-discharge follow-up, to determine the eligibility of sacubitril/valsartan initiation using FDA approval criteria and PARADIGM-HF trial enrollment criteria.Citation47 Of the 149 (71% total) patients who were eligible based on FDA labeling, only 54 (26% total) were eligible based on PARADIGM-HF enrollment criteria ().Citation47 The authors found that the patients who did not meet PARADIGM-HF enrollment criteria were sicker with higher NYHA functional class, lower SBP, greater NT-proBNP level, lower eGFR, and they were less likely to be on ACEI, beta-blocker, and an MRA.Citation47 These findings reiterate the significant evidence gap with regards to FDA labeling of sacubitril/valsartan and proves concerning for the safety of sacubitril/valsartan as it can be used now in real-world HF population which was not represented in the PARADIGM-HF trial.
The above-mentioned analyses are primarily in hospitalized patients, whereas PARADIGM-HF enrolled ambulatory patients. European investigators analyzed registry data to establish the eligibility of ambulatory patients with HFrEF for treatment with sacubitril/valsartan. Simpson et al analyzed the Swedish Heart Failure Registry (SwedeHF) to determine the eligibility of patients with HFrEF for treatment with sacubitril/valsartan, according to the criteria used in PARADIGM-HF ().Citation48 They identified 12,914 ambulatory patients with symptomatic (NYHA class II–IV) HFrEF (LVEF <40%), of which 6,452 were treated with at least enalapril 10 mg daily or equivalent.Citation48 Of these 6,452 patients treated with enalapril 10 mg daily or equivalent, 5,015 (77.7%) were eligible for treatment with sacubitril–valsartan using PARADIGM-HF inclusion criteria and the most common reason for ineligibility was low natriuretic peptide level (17.6%).Citation48 Very few ambulatory symptomatic HFrEF patients on enalapril were ineligible due to a low eGFR of <30 mL/min/1.73 m2 (87/6,452; 1.3%) or serum potassium >5.2 mmol/L (51/6,452; 0.7%).Citation48 Based on these findings, 38.8% of the ambulatory SwedeHF patients with symptomatic HFrEF were eligible for sacubitril/valsartan initiation. The findings from this study make sense in a broader perspective, as ambulatory HF patients are less sick than hospitalized patients and have lower natriuretic peptide levels, higher eGFR, and lower serum potassium levels.
These findings are in contrast with those reported by Pellicori et al who studied patient population in a community HF referral clinic in the UK between 2001 and 2014.Citation49 They identified 1,396 chronic HFrEF patients with LVEF ≤40% and available NT-proBNP measurements ().Citation49 Of the 379 patients (27% of total) who were on target dose of ACEI/ARB, only 172 patients (45% of 379) were eligible for sacubitril–valsartan initiation based on PARADIGM-HF enrollment criteria.Citation49 Lack of symptoms and low NT-proBNP <600 ng/L levels were the most common reasons for ineligibility.Citation49 A further 122 patients became eligible during follow-up. Based on this study, in a community-based chronic HFrEF population, only 21% (294/1,396) were eligible for sacubitril/valsartan initiation based on PARADIGM-HF enrollment criteria, a number that increased to 60% (701/1,396) when background medications were ignored.Citation49 However, it should be remembered that being on an ACEI/ARB is a requirement prior to ARNI initiation. It is also important to note that this study is based on a single referral HF clinic, whereas the SwedeHF included a broader HFrEF population, which can explain the difference in the proportions of ambulatory patients who were eligible for sacubitril/valsartan initiation.
Zeymer et al compared PARADIGM-HF enrollment criteria with retrospective data from three German chronic HFrEF (LVEF <40%) registries/studies and reported that patients enrolled in PARADIGM-HF trial represented about 50% of the general population of patients with HFrEF in these registries.Citation50 It is interesting to note that only 5.3%–20.4% patients in the registries were treated with enalapril. Overall, it is evident that the patient population studied in the PARADIGM-HF does not represent the entire real-world HFrEF population largely because of the lack of symptoms (NYHA class I), not being on an ACEI/ARB, or low levels of natriuretic peptide. It is obvious from these findings that sacubitril/valsartan cannot be prescribed for the entire HFrEF population, given that a few major exclusions in the trial represent a significant number of real-world HFrEF population. It is also apparent that the differences in FDA labeling and consensus recommendations may result in this ARNI being used in a larger HFrEF population than it is evaluated in.
Conclusion
Although the PARADIGM-HF trial provided compelling evidence for the superiority of angiotensin receptor-NEP inhibition over enalapril in HFrEF patients, it is important to note that certain subgroups of patients who represent a significant proportion of the real-world HF population were underrepresented or excluded from the original trial. Real-world eligibility data suggest that only 20%–40% of the HFrEF patients will be eligible for sacubitril/valsartan initiation based on current guidelines. The differences in FDA labeling and international consensus recommendations may result in this ARNI being used in a larger HFrEF population than it is studied in or recommended for, raising important safety concerns. It is crucial to clarify this evidence gap to prevent unwarranted complications in HFrEF patients in whom sacubitril/valsartan will be prescribed. Variations in inter-consensus guidelines must be also clarified, as these differences might affect patient selection. Despite these reservations, sacubitril/valsartan is an important breakthrough for the management of HFrEF and should be used in appropriately selected patients to provide morbidity and mortality reduction. Available evidence suggests that sacubitril/valsar-tan might have a metabolic and nephroprotective benefit in HFrEF patients and proposes a significant CV benefit of this ARNI, irrespective of the type or etiology of HF. Ongoing trials testing this combination across various comorbidity profiles will expand the current indications of this game-changer medication in the management of HF.
Disclosure
The authors report no conflicts of interest in this work.
References
- RedfieldMMHeart Failure with preserved ejection fractionN Engl J Med2016375191868187727959663
- FonarowGCStoughWGAbrahamWTCharacteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF RegistryJ Am Coll Cardiol20075087687717707182
- BraunwaldEThe war against heart failure: the Lancet lectureLancet2015385997081282425467564
- MozaffarianDBenjaminEJGoASHeart disease and stroke statistics-2016 update: a report from the American Heart AssociationCirculation2016133438360
- GheorghiadeMPangPSAcute heart failure syndromesJ Am Coll Cardiol200953755757319215829
- RudigerAHarjolaVPMullerAAcute heart failure: clinical presentation, one-year mortality and prognostic factorsEur J Heart Fail20057466267015921809
- FonarowGCAbrahamWTAlbertNMAssociation between performance measures and clinical outcomes for patients hospitalized with heart failureJAMA20072971617017200476
- RogerVLEpidemiology of heart failureCirc Res2013113664665923989710
- McMurrayJJPackerMDesaiASAngiotensin-neprilysin inhibition versus enalapril in heart failureN Engl J Med201437111993100425176015
- YandrapalliSAronowWSMondalPThe evolution of natriuretic peptide augmentation in management of heart failure and the role of sacubitril/valsartanArch Med Sci20171351207121628883863
- YancyCWJessupMBozkurtB2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the heart failure society of AmericaCirculation20171366e137e16128455343
- MoeGWEzekowitzJAO’MearaEThe 2014 Canadian Cardiovascular Society heart failure management guidelines focus update: anemia, biomarkers, and recent therapeutic trial implicationsCan J Cardiol201531131625532421
- PonikowskiPVoorsAAAnkerSD2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Eur J Heart Fail201618889197527207191
- GuJNoeAChandraPPharmacokinetics and pharmacodynamics of LCZ696, a novel dual-acting angiotensin receptor – neprilysin inhibitor (ARNi)J Clin Pharmacol201050440141419934029
- VardenyOMillerRSolomonSDCombined neprilysin and renin-angiotensin system inhibition for the treatment of heart failureJACC Heart Fail20142666367025306450
- YandrapalliSAronowWSMondalPLimitations of sacubitril/valsartan in the management of heart failureAm J Ther2017242234239
- PackerMMcMurrayJJDesaiASAngiotensin receptor neprilysin inhibition compared with enalapril on the risk of clinical progression in surviving patients with heart failureCirculation20151311546125403646
- McMurrayJPackerMDesaiASA putative placebo analysis of the effects of LCZ696 on clinical outcomes in heart failureEur Heart J201536743443925416329
- FDA news release: FDA approves new drug to treat heart failureU.S. Food and Drug Administration2015 Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm453845.htmAccessed June 12, 2017
- Summary of the Risk Management Plan (RMP) for Entresto (Sacubitril/Valsartan)EMA2015 Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Risk-management-plan_summary/human/004062/WC500194315.pdfAccessed June 20, 2017
- VinereanuDSacubitril-valsartan for heart failure: from devil’s advocate to evidence-based medicineAm J Ther2017242109110
- DesaiASSolomonSClaggettBFactors associated with non-completion during the run-in period before randomization and influence on the estimated benefit of LCZ696 in the PARADIGM-HF TrialCirc Heart Fail201696002735
- FonarowGCStoughWGAbrahamWTCharacteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF RegistryJ Am Coll Cardiol200750876877717707182
- YancyCWLopatinMStevensonLWClinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) DatabaseJ Am Coll Cardiol2006471768416386668
- JhundPSFuMBayramEEfficacy and safety of LCZ696 (sacubitril-valsartan) according to age: insights from PARADIGM-HFEur Heart J2015362576258426231885
- NovartisStudy of efficacy and safety of LCZ696 in Japanese patients with chronic heart failure and reduced ejection fraction (PARALLEL-HF) Available from: https://clinicaltrials.gov/ct2/show/NCT02468232. NLM identifier: NCT02468232Accessed August 10, 2017
- KristensenSLMartinezFJhundPSGeographic variations in the PARADIGM-HF heart failure trialEur Heart J201637413167317427354044
- NovartisEfficacy and safety of LCZ696 compared to valsartan, on morbidity and mortality in heart failure patients with preserved ejection fraction (PARAGON-HF) Available from: http://clinicaltrials.gov/ct2/show/NCT01920711. NLM identifier: NCT01920711Accessed June 11, 2017
- NovartisA randomized, double-blind controlled study comparing LCZ696 to medical therapy for comorbidities in HFpEF Patients (PARALLAX) Available from: http://clinicaltrials.gov/ct2/show/NCT03066804. NLM identifier: NCT03066804Accessed June 10, 2017
- SimpsonJJhundPSRouleauJEffect of sacubitril/valsartan compared with enalapril, according to etiology in PARADIGM-HFAbstract presented at: American College of Cardiology Scientific SessionsMarch 2017Washington, DC
- SolomonSPackerMZileMThe angiotensin receptor neprilysin inhibitor LCZ696 is effective across the spectrum of ejection fraction in heart failure with reduced ejection fractionJ Card Fail2015218S45S46
- DesaiASMcMurrayJJPackerMEffect of the angiotensin receptor-neprilysin inhibitor LCZ696 compared with enalapril on mode of death in heart failure patientsEur Heart J201536301990199726022006
- RiddellEVaderJMPotential expanded indications for neprilysin inhibitorsCurr Heart Fail Rep201714213414528281174
- JongPYusufSRousseauMFEffect of enalapril on 12-year survival and life expectancy in patients with left ventricular systolic dysfunction: a follow-up studyLancet200336193721843184812788569
- PfefferMABraunwaldEMoyéLAEffect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarctionN Engl J Med1992327106696771386652
- DargieHJEffect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomized trialLancet200135792661385139011356434
- SolomonSDClaggettBPackerMEfficacy of sacubitril/valsartan relative to a prior decompensation: the PARADIGM-HF trialJACC Heart Fail201641081682227395349
- NovartisComparison Of sacubitril/valsartan enalapril on effect on ntpRo-bnp in patients stabilized from an acute heart failure episode (PIONEER-HF) Available from: http://clinicaltrials.gov/ct2/show/NCT02554890. NLM identifier: NCT02554890Accessed June 10, 2017
- NovartisComparison of pre- and post-discharge Initiation of LCZ696 Therapy in HFrEF patients after an acute decompensation event (TRANSITION) Available from: http://clinicaltrials.gov/ct2/show/NCT02661217. NLM identifier: NCT02661217Accessed June 9, 2017
- NovartisProspective ARNI vs ACE inhibitor trial to determine superiority in reducing heart failure events after MI (PARADISE-MI) Available from: http://clinicaltrials.gov/ct2/show/NCT02924727. NLM identifier: NCT02924727Accessed June 9, 2017
- MaggioniAPAnkerSDDahlströmUAre hospitalized or ambulatory patients with heart failure treated in accordance with European Society of Cardiology guidelines? Evidence from 12,440 patients of the ESC heart failure long-term registryEur J Heart Fail201315101173118423978433
- NovartisUK Heart and Renal Protection (UK HARP-III) Available from: http://www.isrctn.com/ISRCTN11958993. NLM identifier: ISRCTN11958993Accessed June 10, 2017
- DesaiASVardenyOClaggettBReduced risk of hyperkalemia during treatment of heart failure with mineralocorticoid receptor antagonists by use of sacubitril/valsartan compared with enalapril: a secondary analysis of the PARADIGM-HF trialJAMA Cardiol201721798527842179
- KristensenSLPreissDJhundPSRisk related to pre-diabetes mellitus and diabetes mellitus in heart failure with reduced ejection fraction: insights from prospective comparison of ARNI with ACEI to determine impact on global mortality and morbidity in heart failure trialCirc Heart Fail201691e00256026754626
- SeferovicJClaggettBSeidelmannSEffect of sacubitril/valsartan versus enalapril on glycaemic control in patients with heart failure and diabetes: a post-hoc analysis from the PARADIGM-HF trialLancet Diabetes Endocrinol20175533334028330649
- ParikhKSLippmannSJGreinerMScope of sacubitril/valsartan eligibility after heart failure hospitalization: findings from the GWTG-HF Registry (Get With The Guidelines-Heart Failure)Circulation2017135212077208028533321
- PerezALKittipibulVTangWHWPatients not meeting PARADIGM-HF enrollment criteria are eligible for sacubitril/valsartan on the basis of FDA approval: the need to close the gapJACC Heart Fail20175646046328571599
- SimpsonJBensonLJhundPSAbstract 19155: “real world” eligibility for sacubitril/valsartan in unselected heart failure patients: data from the Swedish heart failure registryCirculation2016134A19155
- PellicoriPUrbinatiAShahPWhat proportion of patients with chronic heart failure are eligible for sacubitril-valsartan?Eur J Heart Fail201719676877828244205
- ZeymerUHochadelMAngermannCRepresentativeness of the PARADIGM heart failure population in real lifePresented at: American College of Cardiology Scientific SessionsMarch 2017Washington, DC
