Abstract
Purpose
The aim of this study was to evaluate the diagnostic accuracy of dual-source computed tomography (DSCT) in coronary artery disease, and to test the possibility of using this technique for coronary risk stratification.
Background
With the advent of DSCT, it is possible to image coronary plaque noninvasively. However, the accuracy of this method in terms of sensitivity and specificity has not been determined. Furthermore, noninvasive determination of plaque composition and plaque burden may be important for improving coronary risk stratification.
Methods
Forty-six patients with known coronary artery disease underwent DSCT quantitative coronary angiography (QCA), and intravascular ultrasound (IVUS) were included in the study. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of DSCT was calculated against QCA and IVUS. Plaque analysis software in a DSCT workstation was used to detect plaque characteristics associated with the Hounsfield unit (Hu) value compared with IVUS. Coronary artery plaques were classified into three types of lesions based on DSCT, and the relationship between different coronary lesions and clinical diagnosis was determined.
Results
DSCT angiography was performed in 46 patients, and a diagnostic-quality CT image was obtained in 44 patients. Coronary angiography was performed in 138 vessels and IVUS in 102 vessels of all 46 patients. Sensitivity, specificity, PPV, and NPV of DSCT compared with QCA was 100%, 98%, 92%, and 100%, respectively. The same corresponding index of DSCT compared with IVUS was 100%, 99%, 95%, and 100%, respectively. Quantitative coronary stenosis analysis revealed a good correlation between DSCT and QCA (r = 0.85, P < 0.05, 95% confidence interval [CI] 0.60–0.87). There was also a good correlation between DSCT and IVUS (r = 0.81, P < 0.05, 95% CI 0.56–0.82). In comparison with IVUS, DSCT predicted plaque characteristics more accurately. The coefficient correlation (r) of luminal cross-sectional area and external elastic membrane cross-sectional area between DSCT and IVUS was 0.82 (P < 0.01, CI 0.67–0.89) and 0.78 (P < 0.01, CI 0.67–0.86), respectively. Three different types of plaque were identified on IVUS. Fatty plaque had a 45 ± 14 Hu value, fibrous plaque 90 ± 20, and calcified plaque 530 ± 185, respectively, on DSCT. The relationship between clinical diagnosis and coronary plaque on DSCT indicated that lesions in patients with unstable angina pectoris or ST elevation myocardial infarction were mainly discrete soft plaques, but there was no significant difference in the distributive characteristics of the lesions in patients with non-ST elevation myocardial infarction and stable angina pectoris patients.
Conclusions
DSCT is a noninvasive tool that allows accurate evaluation of plaque characteristics, diagnosis of coronary artery disease, and stratification of coronary risk according to different coronary plaque type.
Introduction
Conventional quantitative coronary angiography (QCA) is considered the gold standard for evaluation of the vascular lumen, and provides excellent results in demonstrating stenotic lesions in coronary artery disease and for coronary risk stratification. However, QCA is an invasive procedure with a small risk of fatal events, making widespread application difficult, and does not allow direct visualization and evaluation of the artery wall. The characterization of coronary plaques without significant luminal narrowing is also not feasible with QCA. Intravascular ultrasound (IVUS) provides a quantitative measurement of atherosclerotic plaque, as well as quantitative assessment of plaque composition, which is used to guide provisional stenting. However, IVUS cannot be used for routine evaluation of plaque characteristics because of its invasiveness and the related increased risk, additional time required, and cost. With development of high speed spiral computed tomography (CT), it has become possible to use CT noninvasively for coronary plaque evaluation and coronary risk stratification.Citation1–Citation3 Dual-source computed tomography (DSCT) can visualize not only the vessel lumen but also the wall, allowing noninvasive assessment of the presence and, potentially, the size of noncalcified coronary plaque. It has been documented that DSCT has extremely high sensitivity and specificity for evaluation of coronary artery stenosis. Nevertheless, DSCT also has some limitations in terms of the most recent generation scanners. For example, the presence of dense calcification in coronary vessels prevents assessment of the degree of luminal obstruction within the calcified zone. Other limitations include the need for a regular heart rhythm and a relatively low heart rate. However, these limitations might be overcome by using the newest generation of CT equipment. This study evaluated the diagnostic accuracy of DSCT and its coronary risk stratification ability compared with invasive coronary angiography and IVUS.
Methods
Study population
From March 2007 to March 2008, we studied 46 patients with known coronary artery disease who were scheduled for coronary angiography. The average age was 65 ± 5.7 years (36 men and 10 women). Exclusion criteria were renal insufficiency (serum creatinine >1.5 mg/dL), hyperthyroidism (basal thyroid-stimulating hormone <0.03 μL in combination with elevated thyroid hormone levels [T3 > 6.3 pmol/L, T4 > 24.32 pmol/L] in peripheral blood), known allergic reaction to iodinated contrast media (Omnipaque®), history of coronary bypass surgery, arrhythmia, severe peripheral vascular disease precluding use of a 8-F arterial sheath, or inability to follow breath-hold commands. The clinical diagnosis was classified into four types, ie, stable angina pectoris, unstable angina pectoris, ST segment elevation myocardial infarction (STEMI), and non-ST segment elevation myocardial infarction (NSTEMI). Informed consent was obtained from each patient before examination.
Dual-source CT scan protocol
All CT scans were performed on a DSCT scanner (Somatom Definition, Siemens Medical Solutions, Forchheim, Germany). For contrast-enhanced scans, vessel opacification was achieved by automated injection of Omnipaque 80 mL at a flow rate of 5 mL/sec using a power injector. Estimation of individual circulation time was of necessity based on the test bolus technique, using a 20 mL bolus and dynamic evaluation software (Dyn EvaTM, Syngo®, Siemens). Collimation was 2 × 32 × 0.6 mm, slice acquisition 64 × 0.6 mm using the z-flying focal spot technique, gantry rotation time 330 msec, pitch 0.20–0.43 adapted to heart rate, tube voltage 120 kV, and maximum tube current 400 mA per rotation. Beta-blockers (25 mg or 50 mg orally) were given to patients whose heart rate was more than 65 beats per minute to ensure temporal resolution.
Coronary angiography and intravascular ultrasound
Aspirin 300 mg and clopidogrel 300 mg were given orally eight hours before angiography. The femoral or radial artery was cannulated using the Seldinger technique. A 6 F Judkins catheter was used. Heparin 3000 U was administered. Coronary angiography was performed in five different projections to unveil the lesions maximally.
The IVUS imaging system (Galaxy®) used was a monorail catheter of 2.7 F with a 40 mHz single crystal mechanical rotary ultrasonic probe (Atlantic Boston Scientific Corporation). A 6 or 7 F guiding catheter of EBU3.5 (Medtronic Launcher®) or XB3.5 (Cordis®) or JR4 (Cordis®) was introduced. A guide wire with diameter of 0.014 inches was sent to the distal portion of target vessel. The automatic pullback velocity was 0.5 mm/sec.
Image analysis
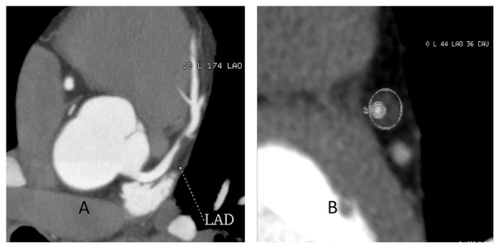
CT data were transferred to an offline workstation (Siemens, Germany), and assessed using the Circulation III package (Siemens, Germany) and Plaque Lens software (Siemens, Germany) for vessel or plaque analysis. The software is based on maximum intensity projections and multiplanar reconstructions. Images were displayed along and orthogonally to the center line of the coronary arteries. For additional orientation, thin-slab maximum intensity projections and three-dimensional volume renderings were also applied. Degree of coronary diameter stenosis (D%) was defined as referential diameter-luminal diameter/referential diameter. In turn, referential diameter was defined as the diameter located in the proximal normal vessel. Luminal cross-sectional area (L-CSA) and external elastic membrane cross-sectional area (EEM-CSA) were calculated (). A cross-section of the targeted lesion was acquired definitively and further L-CSA and EEM- CSA were also calculated by plaque analysis after manual definition of the border of the vessel lumen and EEM. The Hounsfield (Hu) value was acquired automatically by plaque analysis software.
Figure 1 Dual-source computed tomography of a 55-year-old male with typical angina. A) Maximum intensity projections of left anterior descending coronary artery showing significant stenosis due to soft plaque. B) Corresponding cross-section of the plaque in A and inner circle showing luminal cross-sectional area, and external circle showing external elastic membrane cross-sectional area.
We stratified coronary artery plaque into three types, ie, a discrete lesion, a diffuse lesion, or a diffuse lesion with extensive calcification (mixed lesion) based on DSCT. A discrete lesion was defined as involvement of not more than two noncalcified plaques. A diffuse lesion was defined when more than two noncalcified plaques were involved, although spotty calcifications were permitted. A mixed lesion was defined as a diffuse lesion with extensive calcification.
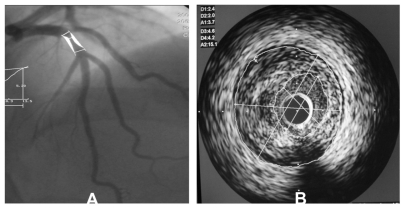
QCA data for coronary stenosis was analyzed using a quantitative analysis software package (Crealife Workstation, China). IVUS data were acquired by offline Sonos Intravascular image analysis software. The method used to calculate L-CSA and EEM-CSA based on IVUS is shown in . Once the area of vessel lumen and external elastic membrane was defined by the investigator, L-CSA and EEM- CSA were calculated automatically by the analysis software. The method used to calculate D% based on IVUS was the same as that based on DSCT.
Figure 2 A) Quantitative coronary angiography of a 45-year-old patient with typical angina showed significant stenosis in middle of the left anterior descending coronary artery and degree of coronary diameter stenosis is 65%. B) Corresponding intravascular ultrasound image of the plaque in the same patient, minimal luminal cross-sectional area is 3.7 mm2 and external elastic membrane cross-sectional area is 15.1 mm2.
Two blinded readers with more than three years’ experience in DSCT independently reviewed the CT on a workstation. The QCA and IVUS image was also reviewed by two blinded readers. The final data were accepted as the average value obtained by two readers. To ensure that the same coronary section was taken by DSCT, QCA, and IVUS, side branches or calcification spots was selected as a distal anatomic marker for reference.
Statistical analysis
Statistical analysis was performed using STATA 8.0 software. A P value less than 0.05 indicates statistical significance. Quantitative variables were expressed as the mean ± standard deviation, and categoric variables as frequencies or percentages. Bland–Altman analysis was used to display the systematic error and confidence interval (CI) between the measurements, whilst the correlation between two indices was assessed by calculation of Pearson’s correlation coefficient. Pearson χ2 test is used to calculate the relationship between clinical diagnosis and lesion anatomy.
Results
Clinical characteristics of patients
Clinical characteristics of the patients are shown in . DSCT angiography was performed in 46 patients one week before coronary angiography Diagnostic CT image quality was obtained in 44 patients, and in two patients only part of the coronary vessels could be visualized with good image quality. Therefore, they were not included in the accuracy analysis. In one patient, respiratory artifact was the reason for poor quality and in the other patient artifact was due to premature ventricular beats. Coronary angiography was performed in all 138 vessels, and IVUS was performed in 102 vessels. There were 42 vessels in the left anterior descending coronary artery, 35 in the left circumflex artery, and 25 in the right coronary artery. A diameter stenosis of 50% was considered significant. The American Heart Association 15-segment classification was used to evaluate coronary segmentation.
Table 1 Clinical characteristics of patients
Accuracy of DSCT for detection of coronary artery stenosis
QCA was performed in 620 segments and in 44 patients in whom DSCT quality was able to be evaluated. One hundred and twelve segments showed significant stenosis and 508 segments were free of lesions. By DSCT, 122 segments showed significant stenosis and 498 segments did not show any significant stenosis. Therefore, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of DSCT was 100%, 98%, 92% and 100%, respectively, in comparison with QCA. IVUS was performed in 420 segments in 44 patients. Eighty segments showed significant stenosis and 320 segments did not have any significant stenosis. By DSCT, 84 segments showed significant stenosis and 316 segments did not. Therefore, the sensitivity, specificity, PPV, and NPV of DSCT compared with IVUS was 100%, 99%, 95%, and 100%, respectively ().
Table 2 Diagnostic accuracy of dual-stage computed tomography
Stenosis and plaque quantification
Quantitative analysis of the stenosis revealed a good correlation between DSCT and QCA (Spearman’s correlation coefficient r = 0.85, P < 0.05, 95% CI 0.60–0.87). It also showed a good correlation between DSCT and IVUS (Spearman’s correlation coefficient r = 0.81, P < 0.05, 95% CI 0.56–0.82). Plaque analysis software in a DSCT work-station was used to detect noncalcified plaques. L-CSA and EEM-CSA in the same lesion were evaluated by DSCT and IVUS. This showed a good correlation between DSCT and IVUS, with a coefficient correlation between the two indices of 0.82 (P < 0.01, CI 0.67–0.89) and 0.78 (P < 0.01, CI 0.67–0.86), respectively ().
Table 3 Coefficient correlation (γ)
Plaque analysis software in a DSCT station was used to determine the Hu value of different plaques compared with IVUS. We classified plaque into three different types according to IVUS, including fatty plaque, fibrous plaque, and calcified plaque. Hu values for fatty, fibrous, and calcified plaques were 45 ± 14, 90 ± 20, and 530 ± 185, respectively. These differences between the three kinds of plaque were statistically significant (P < 0.05).
Relationship between clinical diagnosis and lesion anatomy
The differential diagnoses of the coronary lesions are shown in . The distribution of coronary lesions according to the four different clinical diagnoses were not significantly different statistically (P = 0.15). However, patients with unstable angina pectoris and those with STEMI had significantly more discrete lesions (P = 0.0007 and 0.01, respectively). For NSTEMI and stable angina pectoris patients, there was no significant difference (P > 0.05).
Table 4 Different diagnosis and lesions based on dual-stage computed tomography
Discussion
It was only a year ago in China that people began to accept the fact that DSCT can be used for coronary imaging.Citation4 Before that, there had been a lot of uncertainty, dispute, and even frank resistance to this new technique. People insist that coronary angiography is the gold standard. In this paper, we have clearly demonstrated that DSCT is reasonably accurate in diagnosing coronary heart disease. Compared with QCA, the sensitivity of DSCT is 100%, specificity is 98%, and NPV is 100%. Compared with IVUS, the results were almost the same. The high accuracy results were mainly due to the fact that the patients were highly selected, and may not reflect the real world situation. The diagnosis was already known and we only wanted to know if the results of DSCT correlate well with QCA and IVUS. There have been many studies comparing DSCT with QCA and IVUS, with conflicting results.Citation5,Citation6 The reason for this is clear, ie, the sensitivity and specificity depend on the prevalence of coronary heart disease. The prevalence is higher and the specificity is poorer because the study was done in highly selected patients. To enter the study, the patients had to undergo both IVUS and QCA. Therefore, many factors which may affect image quality were eliminated before the study, for example, artifact and severe calcification.
Once the validation was completed we could proceed to analyze the images quantitatively by tracing the DSCT images. L-CSA and EEM-CSA were used to calculate stenosis. A strength of this study was the demonstration that DSCT can quantitate stenosis and plaque, much like IVUS. The correlation between DSCT and IVUS were excellent, with r = 0.82 (P < 0.01, CI 0.67–0.89).
The advantage of DSCT was its ability to analyze plaque.Citation7 The CT density value can help characterize the nature of plaque. According to the CT density hypothesis, the lower the Hu unit is, the more unstable the plaque. We classified plaque into three different types, according to Hu value, as fatty, fibrous, or calcified plaque. There were very good correlation between Hu value and IVUS, including for fatty plaque, fibrous plaque, and calcified plaque. Hu values for fatty, fibrous and calcified plaque were, respectively, 45 ± 14, 90 ± 20, and 530 ± 185, with the difference being statistically significant for the three kinds of plaque (P < 0.05). Motoyama et alCitation8 used a cutoff value of <30 Hu or 30 Hu _NCP _150 to diagnoses soft plaque or fibrous plaque. There was a good correlation between Hu value and clinical diagnosis. For stable angina the range was 30 Hu _NCP _150. In acute coronary syndromes, however, the range was <30 Hu. We divided our patients into STEMI, NSTEMI, unstable angina, and stable angina. Even with the same clinical diagnosis, different anatomic entities could be detected by DSCT. Discrete lesions detected by DSCT were found more in patients with unstable angina pectoris or a STEMI, while diffuse and mixed lesions were detected more often in patients with an NSTEMI or stable angina. This finding is in accordance with the unstable plaque hypothesis. A large, soft, and expansive plaque represents a vulnerable one. In patients with diffuse and calcified lesions there were a lot of episodes of NSTEMI and stable angina. The course of the disease is protracted but less risky than when associated with new-onset unstable angina pectoris. In view of the broad range of disease entities involved, it is necessary to incorporate the anatomic diagnosis into a clinical diagnosis.Citation9 The treatment strategy would also be different. We hypothesized that, for discrete soft plaques, stenting would be the best choice in terms of long-term results, whereas a medical or surgical strategy would be a reasonable choice for diffuse or calcified lesions.
Cardiac imaging for coronary artery disease has made excellent progress since the advent of multislice spiral CT.Citation10,Citation11 Coronary CT angiography has gained more robustness and accuracy since the development of the more recent generations of CT scanners.Citation12 In contrast with earlier studies using MSCT systems with lower temporal resolution, dual-source technology has demonstrated good clinical robustness.Citation13,Citation14 In China, some recent studies have focused on the accuracy of DSCT compared with IVUS, but the results have not been consistent. Therefore, we carried out a study to confirm the diagnostic accuracy of DSCT. This is one of the first studies demonstrating that DSCT, unlike QCA and IVUS, allows evaluation of coronary stenosis and plaque characteristics simultaneously. This may be the first time that three different types of coronary plaque have been identified and related to different types of coronary artery disease.
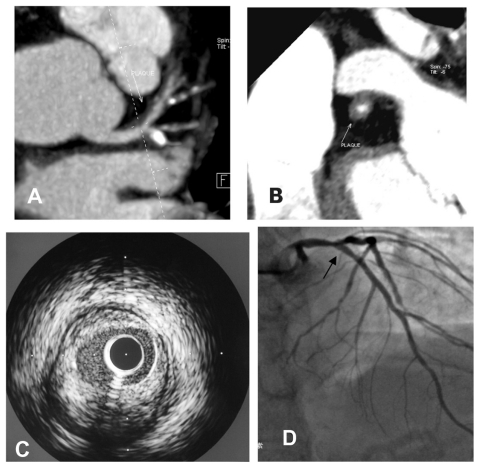
In earlier studies it was demonstrated that multislice spiral CT-derived stenosis qualification is difficult, especially in the presence of calcifications that sometimes lead to an overestimation of stenosis severity.Citation15–Citation17 However, in a recent scientific statement from the American Heart Association, multislice CT angiography gained a Class IIa recommendation as a first-line diagnostic test for patients with an intermediate likelihood for significant coronary stenosis.Citation18 In the present study, we therefore aimed to test the performance of DSCT in clinically relevant patients. Our results reveal that DSCT has good concordance compared with QCA in significant stenosis (>50%). It also showed good concordance with IVUS ( demonstrates a typical case).
Figure 3 Images from a 45-year-old male patient with typical angina. A) shows a noncalcified plaque located in the left main coronary artery leading to significant stenosis see on dual-source computed tomography. B) Corresponding crosssection of the same plaque on dual-source computed tomography. C) Intravascular ultrasound indicating that the major composition of this plaque was fibrosis. D) Coronary angiography indicating a significant stenosis located in the left main coronary artery near to bifurcation.
In our study, plaque analysis software in a DSCT work-station was used to detect the characteristics of noncalcified plaque. It showed good coherence between DSCT and IVUS. The coefficient correlations (r) of L-CSA and EEM-CSA are 0.82 and 0.78, respectively. This result is similar to those of other studies of the accuracy of DSCT in detecting plaque characteristics. It has been widely reported that DSCT can evaluate noncalcified plaque accurately. However, for widely calcified plaque, the accuracy of DSCT is still questionable.Citation19
Coronary risk stratification has an important role in the diagnosis and treatment of coronary artery disease. The best known is the Global Registry Of Acute Coronary Events (GRACE) system. However, there are still limitations because the real status of the coronary artery is not clear. Although coronary angiography can show us the coronary artery clearly and the degree of stenosis is very clear, the plaque characteristics on the wall of the coronary artery are uncertain. DSCT can provide us with all of this information. Recently, there have been some studies focusing on multislice CT characteristics of coronary lesions in acute coronary syndromes and contrasted them with those in stable angina pectoris.Citation20 The CT characteristics of plaque associated with acute coronary syndromes include positive vascular remodeling, low plaque density, and spotty calcification which is very different to stable angina pectoris.Citation21 It is logical to presume that plaques vulnerable to rupture harbor similar characteristics. In this study, we firstly classified coronary plaques into three types of lesion and tried to discover the relationship between coronary lesions and diagnosis to stratify coronary risk by DSCT. Our study revealed that lesions in patients with unstable angina pectoris and STEMI are associated with discrete plaque. For NSTEMI and stable angina pectoris patients, there is no obvious distribution of types of lesion. The above result is just a start, and more detailed studies will investigate the characteristics of these types of plaques and the clinical diagnosis using DSCT.
Disclosure
The authors report no conflicts of interest in this work.
References
- LeschkaSAlkadhiHPlassAAccuracy of MSCT coronary angiography with 64-slice technology: First experienceEur Heart J2005261482148715840624
- RaffGLGallagherMJO’NeillWWGoldsteinJADiagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomographyJ Am Coll Cardiol20054655255716053973
- SteinPDBeemathAKayaliFSkafESanchezJOlsonREMulti-detector computed tomography for the diagnosis of coronary artery disease: A systematic reviewAm J Med200611920321616490463
- WangMHSunAJQianJYMyocardial bridging detection by non-invasive multislice spiral computed tomography: Comparison with intravascular ultrasoundChin Med J (Engl)2008121172118208659
- LeberAWKnezAvon ZieglerFQuantification of obstructive and non-obstructive coronary lesions by 64-slice computed tomography: A comparative study with quantitative coronary angiography and intravascular ultrasoundJ Am Coll Cardiol20054614715415992649
- MeijboomWBvan MieghemCAMolletNR64-slice computed tomography coronary angiography in patients with high, intermediate, or low pretest probability of significant coronary artery diseaseJ Am Coll Cardiol2007501469147517919567
- KitagawaTYamamotoHOhhashiNComprehensive evaluation of noncalcified coronary plaque characteristics detected using 64-slice computed tomography in patients with proven or suspected coronary artery diseaseAm Heart J20071541191119818035094
- MotoyamaSKondoTSaraiMMultislice computed tomographic characteristics of coronary lesions in acute coronary syndromesJ Am Coll Cardiol20075031932617659199
- GaiLLiPJinQYangXCT-guided stenting of chronically occluded coronary arteryZhonghua Xin Xue Guan Bing Za Zhi200810331333 Chinese
- SchuijfJDShawLJWijnsWCardiac imaging in coronary artery disease: Differing modalitiesHeart2005911110111716020614
- HamonMBiondi-ZoccaiGGMalaguttiPDiagnostic performance of multislice spiral computed tomography of coronary arteries as compared with conventional invasive coronary angiography: A meta-analysisJ Am Coll Cardiol2006481896191017084268
- MartuscelliERomagnoliAD’EliseoAAccuracy of thin-slice computed tomography in the detection of coronary stenosisEur Heart J2004251043104815191775
- YeH-HHideakiKShigeruSQualitative and quantitative evaluation of coronary plaques with 64-slice computed tomography in comparison with intravascular ultrasoundZhonghua Xin Xue Guan Bing Za Zhi200735648651 Chinese17961433
- CaussinCLarchezCGhostineSComparison of coronary minimal lumen area quantification by sixty-four-slice computed tomography versus intravascular ultrasound for intermediate stenosisJ Am Coll Cardiol200698871876
- SunJZhangZLuBIdentification and quantification of coronary atherosclerotic plaques: A comparison of 64-MDCT and intravascular ultrasoundAJR Am J Roentgenol200819074875418287448
- LeberAWJohnsonTBeckerADiagnostic accuracy of dual-source multi-slice CT coronary angiography in patients with intermediate pretest likelihood for coronary artery diseaseEur Heart J2007282354236017644815
- JohnsonTRNikolaouKBuschSDiagnostic accuracy of dual-source computed tomography in the diagnosis of coronary artery diseaseInvest Radiol20074268469117984765
- FineJHopkinsCBRuffNNewtonFCComparison of accuracy of 64-slice cardiovascular computed tomography with coronary angiography in patients with suspected coronary artery diseaseAm J Cardiol20069717317416442357
- MinJKShawLJDevereuxRBPrognostic value of multidetector coronary computed tomographic angiography for prediction of all cause mortalityJ Am Coll Cardiol2007501161117017868808
- LiXMHuangCXWangTSZhuangSWZhouHTianBComparison of coronary plaque composition among patients with acute coronary syndrome and stable coronary artery diseaseChin Med J (Engl)200812153453918364141
- PundziuteGSchuijfJDJukemaJWEvaluation of plaque characteristics in acute coronary syndromes: Non-invasive assessment with multi-slice computed tomography and invasive evaluation with intravascular ultrasound radiofrequency data analysisEur Heart J2008292373238118682447