Abstract
Bleeding related to inadvertent femoral catheter insertion is an infrequent but morbid complication. We report two cases of acute life-threatening bleeding after attempts at femoral vein catheterization. Both patients were morbidly obese, had multiple comorbidities, and were at high risk for surgical intervention. Aggressive resuscitation failed to stabilize the patients. Emergency digital subtraction angiography diagnosed the site of the femoral artery bleeding. In one patient, the site of injury was the right profunda femoris artery. Both bleeding sites were controlled successfully with endovascular covered stent placement, without complication. Although prior publications have reported the concept of endovascular repair in femoral artery injuries, to the best of the author’s knowledge, covering the profunda femoris artery with no complications has not been described previously. In critically ill patients with life-threatening hemorrhage following inadvertent femoral catheterization, management with endovascular covered stents is safe and effective.
Introduction
Femoral vein catheterization is often carried out during resuscitation and in critical care units to provide venous access and nutritional support or to manage perioperative fluids. It is usually achieved via a blind approach, localizing the femoral pulse manually using external landmarks. However, this approach can be challenging in patients who are obese or have severe shock, as the femoral pulse could be absent, weak, or too deep to palpate. Inadvertent femoral catheter insertion can cause hemorrhage, pseudoaneurysm, arteriovenous fistulation, arterial dissection, or neurological injury.Citation1,Citation2 Operative repair has been the traditional treatment. However, for active bleeding in obese patients with abnormal coagulation and a high risk to conventional anesthesia, endovascular treatment could be seen as a safe and effective therapeutic alternative.Citation1–Citation3
Case 1
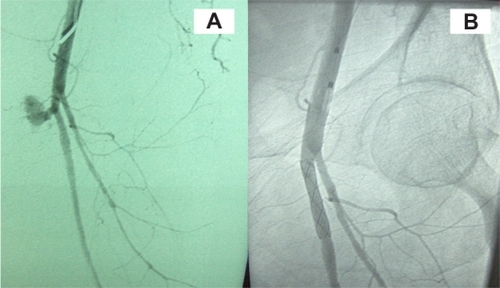
A 66-year-old female who was morbidly obese and known to have diabetes mellitus, hypertension, and renal impairment was admitted to the intensive care unit (ICU) with acute biliary pancreatitis and active rectal bleeding due to colonic polyps. After admission, she developed massive per-rectum bleeding with hypovolemic shock. The patient’s pulse was weak and her blood pressure could not be measured accurately using a pressure cuff. Her peripheral veins were difficult to cannulate because of her obesity and the hypovolemic shock. During resuscitation, several attempts to insert a large-bore catheter (8.5 Fr high flow fluid administration set) in the right femoral vein failed, and the procedure was aborted. A firm pressure dressing was applied to the puncture site. A left jugular catheter was successfully inserted, and fluid and blood resuscitation started. The patient was stabilized; however, she continued to be in a critical condition and developed coagulopathy. A few hours later, the patient developed a groin hematoma, which was rapidly progressing in size. An urgent color duplex ultrasound scan showed an 8 cm × 10 cm femoral pseudoaneurysm that was actively bleeding. Laboratory studies showed a fall in hemoglobin from 9 to 5 g/dL. The patient developed hypovolemic shock, and resuscitation was difficult. The right groin hematoma continued to increase in size. As the patient was at high risk for conventional anesthesia due to her comorbidities, endovascular therapy was planned instead of surgery. Under local anesthesia, an angiography was performed via a left femoral approach. There was evidence of active bleeding from the right superficial femoral artery just beyond the common femoral bifurcation (). An 8 mm × 40 mm self-expanding polytetrafluoroethylene (PTFE)-covered stent (Fluency; C.R. Bard, Inc., Murray Hill, NJ, USA) was deployed, and bleeding was successfully controlled (). No complications related to the procedure were observed. The patient went back to the ICU when she was stabilized.
Case 2
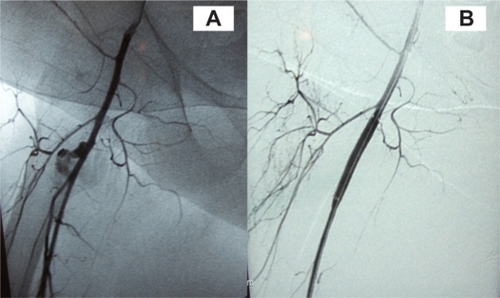
A 60-year-old female with morbid obesity was admitted to the ICU with septic shock due to peritonitis. She was known to have end-stage renal disease on peritoneal dialysis, diabetes, and hypertension. Several attempts to insert a right femoral dialysis access failed. The patient developed a groin hematoma with a drop in her hemoglobin. An ultrasound confirmed active bleeding from the right femoral artery, and the patient was prepared for surgical repair. However, before transfer to the operating room, the patient collapsed with hypotension and an increase in the right groin hematoma. Her hemoglobin dropped from 8 to 4 g/dL and she developed coagulopathy. She was resuscitated and transferred to the angiography suite where an angiogram confirmed the site of active bleeding to be from the deep femoral artery (). An 8 mm × 40 mm self-expanding PTFE-covered stent (Fluency; C.R. Bard, Inc.) was deployed in the common femoral artery, extending to the superficial femoral artery and occluding the deep femoral artery (). An angiogram showed patent superficial femoral, popliteal, and distal vessels. No complications related to the procedure were observed.
Discussion
Central venous catheter (CVC) placement is an essential part of clinical management of many conditions in hospitalized patients. CVCs are inserted for several reasons, including hemodynamic monitoring, fluid replacement, hemodialysis, total parenteral nutrition, management of perioperative fluids, and delivery of blood products and drugs such as vasopressors, chemotherapy, and antibiotics.Citation4 In addition, they are a vital tool for critically ill patients who require aggressive fluid management and intensive care.Citation5,Citation6 The common femoral vein is a common access site for CVC placement. Their insertion is usually achieved via a blind, external landmark-guided technique, through manual localization of the femoral artery. Iatrogenic arterial injury at the puncture site is a potential complication of CVC placement. It can present acutely with life-threatening blood loss or can insidiously lead to a pseudoaneurysm formation.Citation7 Femoral catheterization has a higher incidence of mechanical complications than the subclavian or internal jugular access,Citation8 with femoral or retroperitoneal hematoma the most frequent major complication, occurring in up to 1.3% of cases.Citation1 Other complications include hematoma, pseudoaneurysm, arteriovenous fistula, arterial dissection, thrombosis, distal embolization, nerve damage, abscess, and lymphocele.Citation2 There are possible factors that influence the risk of these complications. They include a faulty puncture technique, ie, low or high puncture sites, either puncture above the inguinal ligament or puncture of the superficial femoral artery or deep femoral artery;Citation9 poor postprocedural compression; length of procedure; multiple attempts; larger devices; and more aggressive anticoagulation during and following the procedure.Citation10,Citation11 Experience has been reported to be another factor.Citation12 Patient-specific risk factors include advanced age, female gender, obesity, coagulopathy, peripheral arterial disease with heavy arterial calcification of the femoral and iliac arteries, hypertension, hemodialysis, hostile groin (excessive scarring following surgery or repeated angiography, or graft material), high division of femoral artery, and nonflexible hip.Citation13,Citation14 The presence of pain or swelling in the groin after catheterization is the most common presentation of a femoral artery injury. Hemodynamic instability and a fall in hemoglobin suggest a life-threatening rupture, which may be occult if retroperitoneal.Citation10
Reports of the advantages of ultrasonography over the anatomic landmark method support the findings of risk reduction and improved cannulation success for all access sites.Citation9,Citation15 The diagnostic examination of choice is duplex ultrasound, which can detect iatrogenic injuries of the femoral artery at the groin with 94% and 97% reported sensitivity and specificity, respectively.Citation16 Management of access site complications may include conservative therapy, percutaneous intervention, and/or vascular surgery.Citation17 Ultrasound-guided compression can be used in minor injuries and stable patients; however, it has major limitations, including patient intolerance for those with compression pain, obese patients, and those who are receiving anticoagulants.Citation16,Citation18 Percutaneous ultrasound-guided thrombin injection is currently the method of choice in many centers for femoral pseudoaneurysms, with a 91% to 100% success rate in large series.Citation9 In obese patients with coagulopathy and hemodynamic instability, these methods are less successful in controlling active bleeding, and urgent surgical vascular repair is indicated.Citation5 The success of surgical repair of iatrogenic femoral access lesions is nearly 100%. However, it may be complicated by several factors, such as anatomical accessibility if the vascular lesion lies deep in the pelvis, and patients’ comorbid conditions, which may augment related morbidity to 25% and mortality to 3.5%.Citation5 In addition, the existing hematoma and local tissue injuries frequently found in such iatrogenically traumatized areas predispose to poor wound healing and postoperative infection, especially if interposition of a synthetic graft is needed.
Endovascular treatment with covered self-expanding stent-grafts has been reported as an effective method in the management of acute arterial bleeding.Citation8,Citation11,Citation14,Citation15 It is performed under local anesthesia, which avoids the need for general or locoregional anesthesia in unstable, high-risk patients. There are several limitations to this procedure, including cost, unfavorable vessel anatomy, and the potential fracture of the stent at a site of mobility near the hip. The risk of covering the deep femoral artery is considered a limitation of the procedure, particularly in patients with severe peripheral arterial disease.Citation11,Citation13 However, in life-threatening situations where an endovascular approach is the only option, saving the patient’s life is a priority over limb perfusion. In our case, the site of injury was the deep femoral artery, which was covered with no effect on the lower limb perfusion, as the superficial femoral artery and distal vessels were patent.
Although there are no long-term studies available at this point comparing different management methods of femoral artery inadvertent injuries, an endovascular approach, with its minimally invasive nature, and short and relatively painless recovery period, appears to be a significant and effective alternative to surgical treatment, especially in high-risk patients.
Conclusion
This study suggests that endovascular therapy with stent-graft is a safe, effective, and life-saving procedure in the management of active life-threatening femoral artery bleeding when traditional open surgery is contraindicated.
Disclosure
The author reports no conflicts of interest in this work.
References
- MerrerJde JongheBGolliotFControlled trial catheterization in critically ill patients: a randomized complications of femoral and subclavian venousJAMA2001286670070711495620
- PikwerAAcostaSKölbelTMalinaMSonessonBAkesonJManagement of inadvertent arterial catheterisation associated with central venous access proceduresEur J Vasc Endovasc Surg200938670771419800822
- GabrielMPawlaczykKWaliszewskiKKrasińskiZMajewskiWLocation of femoral artery puncture site and the risk of postcatheterization pseudoaneurysm formationInt J Cardiol2007120216717117250906
- TercanFOzkanUOguzkurtLUS-guided placement of central vein catheters in patients with disorders of hemostasisEur J Radiology200865253256
- TanaPLGibsonMCentral venous catheters: the role of radiologyClin Radiol200661132216356812
- KapadiaSParakhRGroverTAgarwalSYadavAEndovascular covered stent for management of arterial pseudoaneurysms after central venous accessJ Cardiothorac Vasc Anesth20072119910217289491
- AratATurkbeyBCilBECanyigitMCekirgeSEmergent treatment of an Iatrogenic arterial injury at femoral puncture site With Symbiot® self-expanding PTFE-covered coronary stent-graftAustralas Radiol200751B331B33317991099
- KusminskyREComplications of central venous catheterizationJ Am Coll Surg2007204468169617382229
- WebberGWJangJGustavsonSOlinJWContemporary management of postcatheterization pseudoaneurysmsCirculation20071152666267417515479
- AhmadFTurnerySATorriePGibsonMIatrogenic femoral artery pseudoaneurysms. A review of current methods of diagnosis and treatmentClin Radiol2008631310131618996260
- SamalAKWhiteCJPercutaneous management of access site complicationsCatheter Cardiovasc Interv200257122312203921
- BallsALoVecchioFStapczynskiSCentral line emergency access registry: a multi-center study to determine resident competency with central venous catheter insertionAnn Emerg Med200750S115
- TsetisDEndovascular treatment of complications of femoral arterial accessCardiovasc Intervent Radiol20103345746820162284
- HeisHABani-HaniKEElheisMAYaghanRJBani-HaniBKPostcatheterization femoral artery pseudoaneurysms: therapeutic options. A case-controlled studyInt J Surg2008621421918455971
- PikwerAAcostaSKölbelTMalinaMSonessonBAkesonJManagement of inadvertent arterial catheterisation associated with central venous access proceduresEur J Vasc Endovasc Surg20093870771419800822
- DemirbasOBatyralievTEksiZPershukovIFemoral pseudoaneurysm due to diagnostic or interventional angiographic proceduresAngiology20055655316193193
- GuilbertMCElkouriSBraccoDArterial trauma during central venous catheter insertion: case series, review and proposed algorithmJ Vasc Surg200848491892518703308
- HillGAlbayatiSThomsonIMacfarlaneJDuttonSvan RijAMIatrogenic pseudoaneurysms: optimal management and treatment optionsJ Vasc Ultrasound2007313131135