Abstract
Background:
The purpose of this observational study was to test the diagnostic performance of the Elecsys® troponin T high-sensitive system combined with copeptin measurement for early exclusion of acute myocardial infarction (MI) in clinical practice.
Methods:
Troponin T high-sensitive (diagnostic cutoff: <14 pg/mL) and copeptin (diagnostic cutoff: <14 pmol/L) levels were determined at admission in addition to other routine laboratory parameters in patients with suspected acute MI presenting to the emergency department of a general hospital over a period of five months.
Results:
Data from 142 consecutive patients (mean age 71.2 ± 13.5 years, 76 men) were analyzed. Final diagnoses were acute MI in 13 patients (nine ST elevation MI, four non-ST elevation MI, 9.2%) unstable angina pectoris in three (2.1%), cardiac symptoms not primarily associated with myocardial ischemia in 79 (55.6%), and noncardiac disease in 47 patients (33.1%). The patients with acute MI were younger and had higher troponin T high-sensitive and copeptin values than patients without acute MI. Seventeen patients had very high copeptin values (>150 pmol/L), one of whom had a level of >700 pmol/L and died of pulmonary embolism. A troponin T high-sensitive level of <14 pg/mL in combination with copeptin <14 pmol/L at initial presentation ruled out acute MI in 45 of the 142 patients (31.7%), each with a sensitivity and negative predictive value of 100%.
Conclusion:
According to this early experience, a single determination of troponin T high-sensitive and copeptin may enable early and accurate exclusion of acute MI in one third of patients, even in an emergency department of a general hospital.
Introduction
According to a World Health Organization report dated January 2011,Citation1 an estimated 7.2 million deaths per year worldwide are due to acute myocardial infarction (MI) or other ischemic disorders of the heart. Rapid detection and diagnostic accuracy is crucial to ensure early effective treatment of this life-threatening disease, which is associated with myocardial cell death due to ischemia, and most often a consequence of acute thrombus formation. Thus, both reliable confirmation of the diagnosis and accurate exclusion of acute MI is of great importance for establishing a rational management system for patients with suspected acute MI in the emergency department which, in turn, would result in optimal utilization of available resources. Confirmation of acute MI requires detection of myocardial necrosis associated with the release of troponin. Serum troponin, a very sensitive marker, has been determined using the assays for conventional troponin T and I for several years now. However, recently, a new highly sensitive assay for detecting serum troponin has been developed. The introduction of this new assay offers the opportunity for improved diagnostic accuracy and early detection of acute MI.Citation2 Although it is capable of detecting myocardial necrosis earlier than conventional troponin assay,Citation2 there remains a troponin-blind interval after onset of chest pain due to the delayed release of troponin following a cardiac injury.Citation3 Therefore, there is a need for a biomarker that is released immediately in the event of endogenous stress, such as onset of chest pain due to acute myocardial ischemia.
In this setting, one of the major hypothalamic stress hormones, arginine vasopressin, comes into play. However, due to its unstable nature and rapid clearance from plasma, measurements of arginine vasopressin are rarely reproducible.Citation4–Citation6 Copeptin, a glycosylated peptide precursor of arginine vasopressin, is more stable and easier to measure. Its levels adequately represent the production of arginine vasopressin.Citation7 In recent years, the prognostic accuracy of copeptin as a stress hormone has been demonstrated in sepsis,Citation8,Citation9 pneumonia and lower respiratory tract infections,Citation10,Citation11 heart disease,Citation12–Citation14 and stroke.Citation15,Citation16 According to the pathophysiological findings,Citation17,Citation18 the arginine vasopressin system can also be counted amongst the neurohumoral pathways, in addition to the renin-angiotensin-aldosterone and sympathetic nervous systems. If the organism is exposed to endogenous stress, such as acute MI, the arginine vasopressin system is activated and copeptin is released. In patients with acute MI, copeptin levels are highest within 3–4 hours of onset of chest pain,Citation19,Citation20 peak on day 1, decrease slightly on day 2, and then reach a plateau 3–5 days after acute MI.Citation13
Rapid and accurate exclusion of acute MI might be possible in up to two thirds of patients with typical chest pain by the combined determination of conventional troponin T and copeptin, a new biomarker, according to two recent studies.Citation19,Citation20 The aim of the present observational study was to assess whether combined determination using the new Elecsys® troponin T high-sensitive system,Citation21,Citation22 which meets the current European Society of Cardiology/American College of Cardiology criteria for detection of myocardial necrosis, and copeptin, which provides additional diagnostic information compared with determination of troponin T high-sensitive alone, is useful for the evaluation of patients with symptoms suggestive of acute MI in an emergency department of a general hospital.
Methods
Patients
A total of 150 consecutive patients with chest pain or other symptoms suggestive of acute MI presenting to the emergency department of the Saale-Unstrut Hospital Naumburg (Germany) between January and June 2010, were initially recruited for the study. Patients with end-stage renal disease undergoing dialysis were excluded. All patients included in the study gave their written informed consent.
Routine examinations at admission
Routine clinical examinations, including standard 12-lead electrocardiography (ECG), blood pressure measurement, pulse oximetry monitoring, and chest radiography were performed in all patients. Benchmark blood parameters and specific myocardial markers, such as creatine kinase MB fraction, and troponin T high-sensitive were determined at presentation, then at 6–9 hoursCitation24 after admission, according to the clinical situation. Additionally, for the first time, the new biomarker copeptin was measured at presentation. Diagnostic procedures and treatment in all patients were performed according to a standardized inhouse protocol. In unclear cases, a consensus between the attending physician and consultant colleagues was reached.
Definition of acute MI
According to the current recommendations,Citation23,Citation25 a diagnosis of acute MI is confirmed when myocardial necrosis in combination with typical clinical symptoms of ischemia and ECG changes, such as new ST-T wave changes, new left bundle branch block, or development of new pathologic Q waves,Citation25 can be accurately detected. In the present study, the diagnosis of acute MI was based on the consensus definition from 2007,Citation25 requiring the detection of myocardial necrosis with a troponin T concentration from at least one measurement exceeding the 99th percentile with a coefficient of variation of <10% and dynamic changes, with a typical increase and/or decrease of the serum level.Citation25,Citation26 In order to fulfill these strict criteria, a high-sensitivity assay for troponin T (Elecsys® troponin T high-sensitive; cobas® e 601, Roche Diagnostics, Mannheim, Germany)Citation21,Citation22 as well as a fourth-generationCitation27 troponin T assay (Roche Diagnostics) were used.
Laboratory investigations
All myocardial markers, including creatine kinase and its MB fraction, were analyzed according to the manufacturer’s instructions. A troponin T high-sensitive value of <14 pg/mL was defined as the cutoff level, representing the 99th percentile of the upper limit in a healthy reference population.Citation22
Blood samples for the measurement of the biomarker copeptin (BRAHMS AG, Henningsdorf, Germany), were stored in tubes with potassium ethylenediamine tetra-acetic acid, centrifuged, frozen at −80°C, and then analyzed as described previously.Citation7 For copeptin, a cutoff value of <14 pmol/L was specified for rapid exclusion of acute MI, as recommended by the manufacturer and used by Reichlin et alCitation19 in a recent study.
ECG analysis
The 12-lead ECGs at admission were analyzed by the attending physician as well as an internal medicine specialist or cardiologist, neither of whom were aware of the patient’s clinical and laboratory parameters. With respect to the changes indicating acute MI, all ECGs were analyzed on the basis of the current recommendations.Citation23,Citation25
Statistical analysis
Categorical data are presented as numbers or relative frequencies and continuous data as means ± standard deviation (SD) or medians with interquartile range (IQR). For comparison of continuous variables between groups and for categorical variables, the analysis of variance test and Fisher’s Exact test were employed, respectively. The Spearman rank correlation coefficient was used to assess the association between troponin T high-sensitive and copeptin. In order to examine the significance of the combination of troponin T high-sensitive and copeptin for the diagnosis of acute MI irrespective of other variables, the logistic regression was applied. A P value <0.05 was accepted as statistically significant. Sensitivity, specificity, positive predictive values, and negative predictive values for troponin T high-sensitive, copeptin, and the combination of both biomarkers were also calculated using the marker-specific cutoffs of <14 pg/mL or <14 pmol/L, respectively, as described above.
Results
Baseline patient characteristics
Of the 150 patients initially included in the study, eight were excluded due either to missing laboratory values for troponin T high-sensitive or copeptin levels, so that data from 142 patients (mean age 71.2 ± 13.5 years, 76 men) were analyzed. Acute MI (ST elevation MI, n = 9; non-ST elevation MI, n = 4) was diagnosed in 9.2% (13/142) of patients. The remaining 129 patients were diagnosed as follows: unstable angina in 2.1% (3/142), cardiac disease not primarily associated with coronary artery disease (including four patients with pulmonary embolism) in 55.6% (79/142), and noncardiac disease in 33.1% (47/142). Baseline clinical characteristics are summarized in .
Table 1 Clinical baseline characteristics of patients
Highly sensitive troponin T measurements
In all patients, the median troponin T high-sensitive level was 14 (IQR 6.3–41.75) pg/mL. For the intra-assay coefficient of variation, a value of 3.4% was calculated. At initial presentation, 49% (70/142) of the patients met the cutoff level of troponin T high-sensitive of <14 pg/mL. Only one (7.7%) of the 13 patients with acute MI had a troponin T high-sensitive concentration of <14 pg/mL at admission. This patient came to the emergency department within four hours of onset of chest pain. In contrast, 69 of the 129 patients (53.5%) without acute MI showed a troponin T high-sensitive level of <14 pg/mL.
Patients with acute MI showed higher values (P < 0.0001) for troponin T high-sensitive (median 135.0 pg/mL, IQR 41.9–440.0 pg/mL) than those with unstable angina pectoris (median 3.0 pg/mL, IQR 3.0–5.6 pg/mL), other cardiac but not primarily ischemia-related disease (median 22.0 pg/mL, IQR 10.1–52.8 pg/mL), or noncardiac disease (median 7.0 pg/mL, IQR 3.8–12.5 pg/mL, ).
Figure 1 Box plots (median, interquartile range) of TropT hs (A) and copeptin (B) in the four patient groups with AMI (n = 13), UAP (n = 3), cardiac disease, but not primarily due to myocardial ischemia (n = 79), or noncardiac diseases (n = 47) at the time point of presentation to the emergency department.
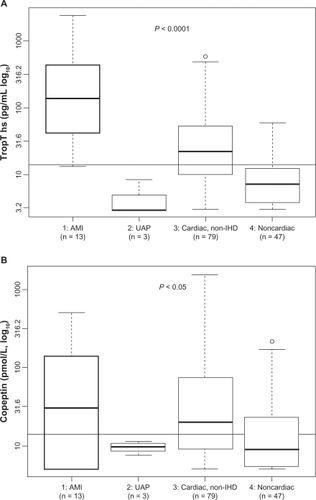
Copeptin measurements
The median copeptin level in the study population was 15.70 pmol/L (IQR 7.28–62.90 pmol/L). The intra-assay coefficient of variation showed a value of 5.9%. In 45.8% (n = 65) of the 142 patients, the cutoff level of <14 pmol/L was found at admission. Of the patients diagnosed with acute MI, 30.8% (4/13) had a copeptin level of <14 pmol/L. Two of the four patients with ST elevation MI presented 5–8 days after initial onset of chest pain, one patient had a prolonged reinfarction after acute coronary intervention one week earlier, and one patient had non-ST elevation MI and sustained angina changing between resolution and recurrence for two days after onset of chest pain. The copeptin level was <14 pmol/L in 47.3% of patients (61/129) without acute MI. Values for copeptin in acute MI patients (median 30.4 pmol/L, IQR 5.0–139.0 pmol/L) differed significantly (P < 0.05) from those in patients with unstable angina pectoris (median 9.7 pmol/L, IQR 8.6–10.6 pmol/L), other nonischemic cardiac disease (median 19.6 pmol/L, IQR 9.2–72.8 pmol/L), or noncardiac disease (median 8.9 pmol/L, IQR 5.4–23.2 pmol/L, ).
Association between highly sensitive troponin T and copeptin
There was a positive correlation between troponin T high-sensitive and copeptin levels at the time of initial presentation (r = 0.41; P < 0.001).
Combination of both biomarkers for early exclusion of acute MI
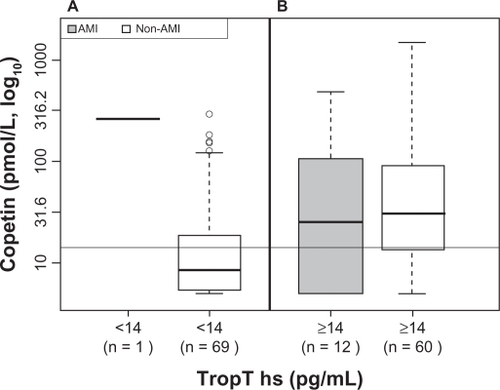
A value of <14 pg/mL for troponin T high-sensitive could be used for rapid exclusion of acute MI with a sensitivity of 92.3%, specificity of 53.5%, positive predictive value of 16.7%, and negative predictive value of 98.6%. The corresponding values for the biomarker copeptin were 69.2%, 47.3%,11.7%, and 93.9%, respectively. A troponin T high-sensitive level of <14 pg/mL in combination with a copeptin value of <14 pmol/L at initial presentation excluded acute MI with a sensitivity of 100%, specificity of 34.9%, positive predictive value of 13.4%, and negative predictive value of 100%, indicating that this combination has an even higher diagnostic accuracy than that of either troponin T high-sensitive or copeptin alone. In 45 (31.7%) of the 142 patients, acute MI could be accurately excluded by a single determination of troponin T high-sensitive and copeptin (). After adjusting for other baseline variables, both troponin T high-sensitive alone and the combination of troponin T high-sensitive and copeptin remained very significant diagnostic parameters for acute MI (P < 0.001 for troponin T high-sensitive alone and for the combination of troponin T high-sensitive and copeptin), while statistical significance was not reached for copeptin alone.
Figure 2 Box plots (median, interquartile range) of copeptin dependent on a TropT hs level of <14 pg/mL (A) and ≥14 pg/mL (B) in AMI and non-AMI patients showing that in non-AMI patients (n = 69) with a TropT hs level of <14 pg/mL, the median of copeptin was clearly below the diagnostic cutoff value of 14 pmol/L, and thereby illustrating that AMI was ruled out in all patients (n = 45) with a TropT hs value of <14 pg/mL in combination with a copeptin level of <14 pmol/L.
Patients with very high copeptin levels
Seventeen patients (12%) had copeptin levels of >150 pmol/L. Of these, only three patients were diagnosed with acute MI. Among the remaining 14 patients, three suffered acute pulmonary embolism, of whom one with a copeptin level of 730 pmol/L died whilst in hospital. The remaining 11 patients were diagnosed as follows: atrial tachycardia (n = 1); decompensated heart failure (n = 4); left-sided pneumonia, urinary tract infection, hypotension, and dehydration (n = 1); severe bilateral pneumonia, hypotension, and dehydration (n = 1); angina pectoris with profound hyperglycemia (n = 1); chest pain and faint of unknown origin (n = 1); and two patients had been resuscitated just before admission to hospital.
Limitations
The main limitation of this observational study was the small number of enrolled patients and therefore a low event rate. Another limitation is the fact that the study patients were recruited on a nonselected basis in an emergency department of a general hospital and not in a specialized chest pain unit where patient selection would occur.
Discussion
We have demonstrated for the first time that combined application of troponin T high-sensitive (using the 99th percentile as a diagnostic cutoff with a 10% coefficient of variationCitation23,Citation25) and copeptin may enable early accurate exclusion of acute MI. In the present observational study, acute MI could be ruled out with a negative predictive value of 100% in one third of patients who presented with symptoms suggestive of acute MI to the emergency department of a general hospital. Compared with troponin T high-sensitive alone, additional determination of copeptin at initial presentation led to a small diagnostic improvement in exclusion of acute MI in only one third of the patients. This finding is in line with data from Keller et alCitation20 who described a negative predictive value of up to 99% using the combination of a more sensitive troponin T (with the 99th percentile as a cutoff with 10% coefficient of variation) and copeptin for ruling out acute MI.
In comparison with two recent studiesCitation19,Citation20 reporting exclusion of acute MI using this algorithm in two thirds of patients with angina, the discrepancy in the present investigation is likely due to the small study population and the low number of events. Furthermore, our patients were recruited from the emergency department of a general hospital situated in a rural region, and hence did not have the same risk of acute MI as did the patients in the two abovementioned studies which recruited patients from the emergency departments of university or urban hospitals.Citation19,Citation20
The lack of correlation between ischemic symptoms and objectively assessable myocardial necrosis in the one acute MI patient with a troponin T high-sensitive value of <14 pg/mL presenting within four hours of onset of chest pain to the emergency department corresponds with the well known fact that early presenters often have a delay in a detectable increase in troponin concentration.Citation28 In contrast, copeptin levels of <14 pmol/L in three acute MI patients presenting on days 2–8 after onset of chest pain and in one patient with a prolonged reinfarction after coronary intervention for acute MI one week prior to the recurrent ischemic event are in line with observations from a previous studyCitation13 describing an increase in the copeptin level peaking on day 1 after onset of chest pain, followed by a decrease on day 2, after which the copeptin levels remained constant at days 3–5. From the pathophysiological point of view, falling copeptin levels just one day after the myocardial ischemic event may indicate adaptation to neurohumoral stress via activation of the arginine vasopressin systemCitation17,Citation18 following acute myocardial ischemia.Citation13
In both situations, the complementary biomarker was elevated, indicating that, especially in early and late presenters with acute MI, the combined application of the two biomarkers, troponin T high-sensitive and copeptin, may contribute to diagnostic accuracy and enable an estimation of the time interval elapsed since onset of chest pain and presentation to the emergency department.
With regard to the 17 patients with very high copeptin values of >150 pmol/L, the results of our study are in accordance with the known fact that copeptin is an endogenous stress hormone reaching markedly elevated levels in critically ill patients.Citation29,Citation30 In the present study, this phenomenon could be observed for cardiac diseases such as acute MI, decompensated heart failure, and atrial tachycardia, as well as in other serious diseases, including acute pulmonary embolism, febrile pneumonia, and acute illnesses associated with depression of the circulation. Taking into account that one patient with acute pulmonary embolism showing a copeptin level of >700 pmol/L at initial presentation died during the inhospital stay, our data confirm that a very high copeptin value may also reflect critical disease states other than acute MI,Citation29 and may be considered a significant predictor of outcome in certain cases, such as in patients with acute pulmonary embolism.
On the basis of this first clinical experience, it is not possible to make any definitive statements with regard to the diagnostic significance of the combined assessment of troponin T high-sensitive and copeptin for exclusion of acute MI. Further prospective, multicenter studies with serial measurements of both biomarkers and longer follow-up of patients are needed to confirm the diagnostic role of the combination of these two new biomarkers in patients with suspected acute MI.
Conclusion
Early measurement of the combination of troponin T high-sensitive and copeptin may revolutionize the diagnostic accuracy and therapeutic decision-making in patients with symptoms suggestive of acute MI. A single combined determination of troponin T high-sensitive and copeptin enables early exclusion of acute MI in one third of patients with a negative predictive value of 100%, even in an emergency department of a general hospital. Additionally, it allows estimation of the time interval between onset of chest pain and presentation with acute MI to the emergency department. This algorithm has the potential to contribute to rational allocation of available resources for patients presenting with chest pain to emergency departments.
Acknowledgements
We thank Mr Oliver Hartmann, biostatistician (BRAHMS AG, Henningsdorf, Germany), for his statistical advice and for performing the calculations.
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health OrganizationCardiovascular diseases (CVDs). Fact sheet No 317World Health Organization2011 Available from: www.who.int/mediacentre/factsheets/fs317/en/index.html. Accessed June 16, 2011.
- DaubertMAJeremiasAThe utility of troponin measurement to detect moycardial infarction: review of the current findingsVasc Health Risk Manag2010669169920859540
- EggersKMOldgrenJNordenskjoldALindahlBDiagnostic value of serial measurement of cardiac markers in patients with chest pain: limited value of adding myoglobin to troponin I for exclusion of myocardial infarctionAm Heart J200414857458115459585
- EvansMJLiveseyJHEllisMJYandleTGEffect of anticoagulants and storage temperatures on stability of plasma and serum hormonesClin Biochem20013410711211311219
- LatendresseGRuizRJBioassay research methodology: measuring CRH in pregnancyBiol Res Nurs200810546218647760
- StruckJMorgenthalerNGBergmannACopeptin, a stable peptide derived from the vasopressin precursor, is elevated in serum of sepsis patientsPeptides2005262500250415922490
- MorgenthalerNGStruckJAlonsoCBergmannAAssay for the measurement of copeptin, a stable peptide derived from the precursor of vasopressinClin Chem20065211211916269513
- MorgenthalerNGMullerBStruckJBergmannARedlHChrist-CrainMCopeptin, a stable peptide of the arginine vasopressin precursor, is elevated in hemorrhagic and septic shockShock20072821922617515850
- LindnerKHStrohmengerHUEnsingerHHetzelWDAhnefeldFWGeorgieffMStress hormone response during and after cardiopulmonary resuscitationAnesthesiology1992776626681329579
- MullerBMorgenthalerNStolzDCirculating levels of copeptin, a novel biomarker, in lower respiratory tract infectionsEur J Clin Invest20073714515217217381
- StolzDChrist-CrainMMorgenthalerNGCopeptin, C-reactive protein, and procalcitonin as prognostic biomarkers in acute exacerbation of COPDChest20071311058106717426210
- StoiserBMortlDHulsmannMCopeptin, a fragment of the vasopressin precursor, as a novel predictor of outcome in heart failureEur J Clin Invest20063677177817032344
- KhanSQDhillonOSO’BrienRJC-terminal provasopressin (copeptin) as a novel and prognostic marker in acute myocardial infarction: Leicester Acute Myocardial Infarction Peptide (LAMP) studyCirculation20071152103211017420344
- TangWHFrancisGSMorrowDANational Academy of Clinical Biochemistry Laboratory Medicine practice guidelines: clinical utilization of cardiac biomarker testing in heart failureCirculation2007116e99e10917630410
- Lloyd-JonesDAdamsRCarnethonMHeart disease and stroke statistics – 2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics SubcommitteeCirculation2009119e21e18119075105
- WhiteleyWChongWLSenguptaASandercockPBlood markers for the prognosis of ischemic stroke: a systematic reviewStroke200940e380e38919286602
- GoldsmithSRVasopressin as vasopressorAm J Med198782121312193300305
- FukuzawaJHanedaTKikuchiKArginine vasopressin increases the rate of protein synthesis in isolated perfused adult rat heart via the V1 receptorMol Cell Biochem1999195939810395073
- ReichlinTHochholzerWStelzigCIncremental value of copeptin for rapid rule out of acute myocardial infarctionJ Am Coll Cardiol200954606819555842
- KellerTTzikasSZellerTCopeptin improves early diagnosis of acute myocardial infarctionJ Am Coll Cardiol2010552096210620447532
- KurzKGiannitsisEBeckerMHessGZdunekDKatusHAComparison of the new high sensitive cardiac troponin with myoglobin, h-FABP and cTnT for early identification of myocardial necrosis in the acute coronary syndromeClin Res Cardiol201110020921520852870
- SaengerAKBeyrauRBraunSMulticenter analytical evaluation of a high sensitivity troponin T assayClin Chim Acta201141274875421219893
- AlpertJSThygesenKAntmanEBassandJPMyocardial infarction redefined – a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarctionJ Am Coll Cardiol20003695996910987628
- MorrowDACannonCPJesseRLNational Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines: clinical characteristics and utilization of biochemical markers in acute coronary syndromesClin Chem20075355257417384001
- ThygesenKAlpertJSWhiteHDUniversal definition of myocardial infarctionJ Am Coll Cardiol2007502173219518036459
- AppleFSJesseRLNewbyLKWuAHChristensonRHNational Academy of Clinical Biochemistry and IFCC Committee for Standardization of Markers of Cardiac Damage Laboratory Medicine Practice Guidelines: analytical issues for biochemical markers of acute coronary syndromesCirculation2007115e352e35517384332
- TateJRTroponin revisited 2008: assay performanceClin Chem Lab Med2008461489150018842109
- MelansonSEFMorrowDAJaroilmPEarlier detection of myocardial injury in a preliminary evaluation using a new troponin I assay with improved sensitivityAm J Pathol2007128282286
- KatanMChrist-CrainMThe stress hormone copeptin: a new prognostic biomarker in acute illnessSwiss Med Wkly2010140w1310120872295
- VoorsAAvon HaehlingSAnkerSDC-terminal provasopressin (copeptin) is a strong prognostic marker in patients with heart failure after acute myocardial infarction: results from the OPTIMAAL studyEur Heart J2009301187119419346228