Abstract
Purpose:
The Rotarex® catheter system is an effective tool for endovascular therapy of acute occluded arteries of the lower extremities, especially for the femoral artery. The authors report the use of the Rotarex catheter system for retrograde percutaneous thrombectomy of an occluded subclavian artery.
Case presentation:
A 79-year-old male patient was referred because of acute pain and paleness of his left arm. Ultrasound examination and computed tomography angiography proved an occlusion of the left subclavian artery from the origin of the vessel. A retrograde recanalization was attempted using the 6F Rotarex catheter and combined with initiation of a local low-dose lytic therapy. A normal blood flow to the left arm was restored. Follow-up examination 3 months later showed a normal perfusion situation of the left upper extremity.
Conclusion:
The Rotarex catheter system is an effective tool for endovascular therapy of acute occluded arteries and efficacy is not restricted to the lower extremities.
Introduction
Subclavian artery thrombosis is a condition in which the blood flow through the vessel is obstructed. Typical symptoms occur secondary to lack of blood flow to the affected extremity. In situations in which the occlusion is secondary to atherosclerosis, acute and subacute thrombosis of the artery is generally minimally symptomatic.Citation1 On the other hand, symptoms of acute embolic occlusion of the subclavian artery are commonly associated with claudication or rest pain on the affected side. Therapeutic intervention is indicated in any symptomatic patient. Surgical treatment (Fogarty balloon thrombectomy, subclavian bypass operation) and local lysis infiltration have been the treatments of choice over recent decades.
Nowadays, modern endovascular thrombectomy devices that use different methods of thrombus fragmentation and transportation are commercially available. Some of these devices use the vortex principle to fragment the thrombus (eg, the Amplatz and the AngioJet® thrombectomy catheters) or the Venturi effect (eg, the Hydrolyser® thrombectomy catheter). One of the most promising devices, which combines clot fragmentation and removal of the fragmented material using Archimedes’ principle, is the Rotarex® catheter (Straub Medical AG, Wangs, Switzerland). It prevents peripheral embolization of the fragmented thrombus by negative pressure. Today the effect of the Rotarex device in lower extremity arteries for recanalization of acute occluded arteries is accepted, but different case reports describe interventional settings in which the system has also been used in other vascular regions.Citation2–Citation4 The authors report the retrograde use of this device via the brachial artery in a patient with acute thrombotic occlusion of the left subclavian artery, which was occluded from the origin of the vessel.
Case presentation
A 79-year-old male patient with history of a stroke was referred to the authors’ cardiovascular clinic because of an acute left arm ischemia. The pain in his left arm occurred 1 day before admission. The pain was not present during rest but it occurred with slight movement of the extremity. No cardiac history was reported previously. On physical examination the left fingers were pale and no pulse was palpable beyond the left axilla. Systolic blood pressure of the left arm was 40 mmHg; on the right side it was 125 mmHg. Doppler examination of the left arm showed a typical post-stenotic flow of the brachial artery and minimal flow of the radial and ulnar arteries. Duplex ultrasound demonstrated a thrombotic occlusion of the visible left subclavian artery and part of the axillary artery. The brachial artery was free of thrombus formation.
A computed tomography (CT) angiogram was performed that proved the thrombotic occlusion of the left subclavian artery beginning at the origin of the vessel (); the CT scan also proved the thrombotic occlusion of the proximal part of the axillary artery. The vertebral artery was involved in the thrombotic process, showing only a low retrograde Doppler signal in ultrasound examination. In the authors’ view, the reason for this thrombotic occlusion seemed to be a thrombotic formation based on a stenosis of the proximal part of the subclavian artery. Transthoracic and transesophageal echocardiography could not identify a cardiac source of the embolic event. The electrocardiogram was monitored over a 24-hour period without documented arrhythmias.
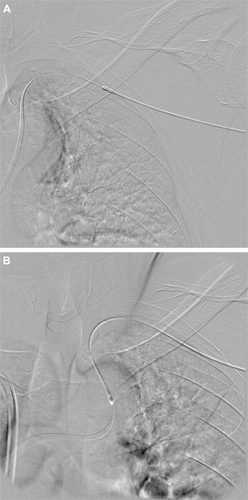
Figure 1 (A) Computed tomography angiogram of the left subclavian artery with thrombotic occlusion from the origin of the artery and (B) retrograde contrast injection through the introducer sheath demonstrates the end of the thrombotic occlusion.
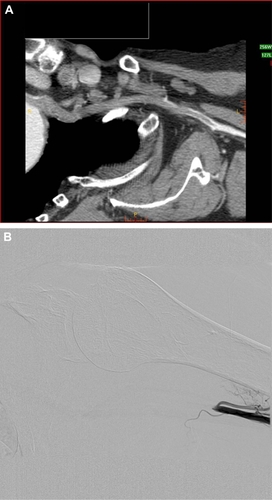
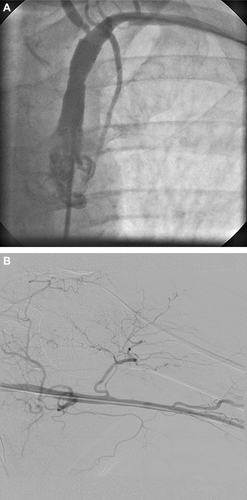
Because of the involved origin of the left subclavian artery, it was decided that a retrograde attempt to reopen the thrombotic occlusion would be performed. The puncture of the not-palpable brachial artery was easily achieved by using ultraound guidance. Five thousand units of heparin were administered after insertion of a 6F Terumo sheath (Terumo Europe NV, Leuven, Belgium). Contrast dye was then injected retrograde through the introducer sheath and the end of the thrombotic occlusion was documented (). For the next step, a 0.018-inch guide wire (Cruiser-18; Biotronik, Buelach, Switzerland) was advanced retrograde through the occluded subclavian artery; it found the way easily into the descending aorta. Using a 5F pigtail catheter (Medtronic GmbH, Meerbusch, Germany), which was advanced proximally of the occlusion, the anatomic situation was documented and overlay images were prepared for a rotational thrombectomy. A 6F Rotarex device was then passed over the 0.018-inch guide wire and through the occlusion four times (). After this procedure most of the thrombotic material was removed, but still some thrombotic formations were documented in the subclavian and axillary arteries. By this time a 70% stenosis of the proximal subclavian artery was visible as the probable underlying reason for the thrombotic occlusion.
A self-expandable nitinol stent (LifeStent® 6 × 30 mm; C.R. Bard GmbH, Karlsruhe, Germany) was then implanted in the stenosis without any problems and it showed a good result after the implantation and post dilatation. After removing most of the thrombotic material, a systolic blood pressure of 90 mmHg at the tip of the introducer sheath was documented. Because of the remaining thrombotic material that was also present near the origin of the subclavian artery, a decision was made in this situation to perform an additional local low-dose lytic therapy. A lysis catheter (C.R. Bard GmbH, Karlsruhe, Germany) was advanced into the subclavian artery and 5 mg bolus of recombinant tissue plasminogen activator (r-tPA) (Actilyse®; Boehringer Ingelheim GmbH, Ingelheim am Rhein, Germany) was locally injected, followed by continuous administration of 2 mg/hr of r-tPA for 20 hours.
The following day, an angiogram performed through the femoral artery documented completely recanalized subclavian and axillary arteries without any remaining thrombus and the patent nitinol stent at the origin of the subclavian artery (). The patient was discharged from the intensive care unit. Doppler pressure measurement showed only a slight difference of 15 mmHg in brachial, radial, and ulnar pressures. The reason for the slight difference in blood pressure between the right and left brachial artery remained unclear. No further invasive diagnostic procedures such as intravascular ultrasound were performed because there was no expected benefit for the clinical result of the patient, who remained asymptomatic after the recanalization procedure. The patient was started on dual antiplatelet therapy immediately after the intervention. Follow-up examinations after 3 months documented a persistence of the Doppler pressures.
Discussion
Acute and subacute ischemia of the extremities is still one of the most frequent reasons for amputation. There are different endovascular options for reperfusion therapy including balloon thrombectomy, local lysis, and rotational thrombectomy. Balloon thrombectomy, the standard surgical treatment, has proven an effective tool for the treatment of acute vascular obstructions. Nevertheless, technical problems and complications can occur. Localized lysis, on the other hand, can be time-consuming and expensive, requiring intensive care monitoring and angiograms after lytic therapy. Over recent years, considerable advances have been made in endovascular interventions for the treatment of acute and subacute ischemia. The authors used the Rotarex rotational thrombectomy device for reopening the subclavian artery in combination with local low-dose lytic therapy. The combination of rotational thrombectomy and localized lysis in this case restored complete perfusion in the left arm.
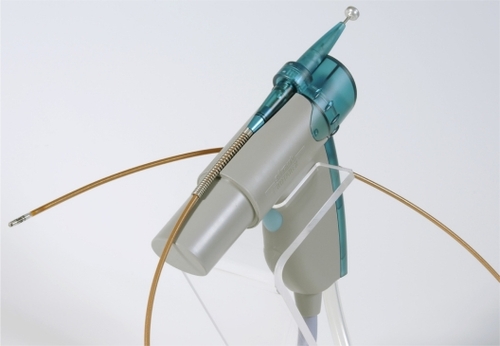
The Rotarex catheter () consists of three modules. A control console is connected to the electric motor that rotates the thrombectomy catheter via an electromagnetic clutch. Within the catheter, a coated steel spiral rotates at 40.000 rpm, which produces a vacuum. This vacuum draws the thrombotic material into two lateral openings of the catheter and fragments it. The fragmented thrombotic material is then transported, via the rotating spiral, into an external collection bag. The Rotarex catheter should be slowly advanced into the occlusion with some short retractions. Some contraindications must be ruled out before the use of the Rotarex catheter. A subintimal position of the guide wire could lead to a perforation of the vessel when using the device in this situation. A vessel diameter below 4 mm is a contraindication for use of the device because of possible vessel damage. Also, the Rotarex catheter should never be used without guide wire. The challenge in this particular case was the total occlusion of the subclavian artery from the origin. After advancing the guide wire retrograde through the occlusion into the aorta, the Rotarex catheter was pushed near the origin and a pullback maneuver was performed. After 5 minutes and four passages there was an acceptable antegrade flow with a blood pressure of 90 – 100 mmHg at the tip of the 6F introducer sheath. Because of the remaining thrombus near the origin of the vessel, it was decided that a lysis catheter would be placed to install a low-dose lysis. The advantage of the combination therapy of rotational thrombectomy and local low-dose lysis in this setting is the minimization of bleeding complications. The patient was started on dual antiplatelet therapy for 4 weeks following the stent implantation.
Explanations for the thromboembolic complication other than the stenosis of the subclavian artery were not found. As in this case, the most probable cause of acute occlusion of the subclavian artery is the underlying atherosclerotic plaque, with rupture of the plaque and local thrombus formation. Most of the other common reasons could be ruled out, such as thoracic outlet syndrome induced by chronic extra-arterial compression from costoclavicular syndrome or cervical rib syndrome.Citation5–Citation7 There were no signs of rheumatic disorders, including arteritis such as Takayasu disease, giant cell arteritis, and polymyalgia rheumatica, which could also lead to an occlusion of the subclavian vessel.Citation8 No aneurysm of the subclavian artery was documented as an underlying reason for the thrombotic occlusion.Citation9 Follow-up examination 3 months later demonstrated an open subclavian artery with just a slight difference of 10 mmHg between both arms in Doppler pressure examination.
Conclusion
In summary, compared with the established therapies, the rotational thrombectomy principle of using the Rotarex catheter system together with optional local low-dose lysis in an acute occluded subclavian artery is a promising therapeutic option.
Disclosure
The authors report no conflicts of interest in this work.
References
- EyersPEarnshawJJAcute non-traumatic arm ischaemiaBr J Surg19988510134013469782011
- ZellerTFrankUBürgelinKSinnLHornBRoskammHAcute thrombotic subclavian artery occlusion treated with a new rotational thrombectomy deviceJ Endovasc Ther20029691792112546597
- LichtenbergMHailerBWiedereröffnung eines akut thrombotisch verschlossenen Aortenstentgrafts unter Einsatz der RotationsthrombektomieZeitschrift für Gefässmedizin2010721621
- LichtenbergMPercutaneous mechanical thrombectomy by means of rotational thrombectomy: current study situation [Perkutane mechanische Thrombektomie mittels Rotationsthrombektomie: Aktuelle Studienlage]Med Klin (Munich)20101051070571020981589
- ThompsonRWPetrinecDToursarkissianBSurgical treatment of thoracic outlet compression syndromes: II. Supraclavicular exploration and vascular reconstructionAnn Vasc Surg19971144424519237004
- FugateMWRotellini-ColtvetLFreischlagJACurrent management of thoracic outlet syndromeCurr Treat Options Cardiovasc Med200911217618319289030
- HoodDBKuehneJYellinAEWeaverFAVascular complications of thoracic outlet syndromeAm Surg199763109139179322672
- HalpinDPMoranKTJewellERArm ischemia secondary to giant cell arteritisAnn Vasc Surg1988243813843224072
- NehlerMRTaylorLMJrMonetaGLPorterJMUpper extremity ischemia from subclavian artery aneurysm caused by bony abnormalities of the thoracic outletArch Surg199713255275329161397