Abstract
Objective
To evaluate the accuracy of the ankle brachial index (ABI) measured with the SCVL® (“screening cardiovascular lab”; GenNov, Paris, France), an automated device with synchronized arm and ankle cuffs with an automatic ABI calculation.
Methods
Patients were consecutively included in a cardiovascular prevention unit if they presented with at least two cardiovascular risk factors. ABI measurements were made using the SCVL, following a synchronized assessment of brachial and ankle systolic pressure. These values were compared to the ABI obtained with the usual Doppler-assisted method.
Results
We included 157 patients. Mean age was 59.1 years, 56.8% had hypertension, 22.3% had diabetes mellitus, and 17.6% were current smokers. An abnormal ABI was observed in 17.2% with the SCVL and in 16.2% with the Doppler. The prevalence rates of an abnormal ABI by patient measured with each device, ie, 15.7% (confidence interval [CI] 0.95: [11.8; 20.4]) or 14.3% (CI 0.95: [10.7; 18.9]), did not differ. The coefficient of variation of Doppler and SCVL measures was 15.8% and 15.1%, respectively. The regression line between the two measurement methods was statistically significant. The value-to-value comparison also shows a difference of mean equal to 0.010 (CI 0.95: [−0.272; 0.291]) (r = −0.055). Reproducibility of ABI measurements with the SCVL showed a difference of mean equal to 0.009 (CI 0.95: [−0.203; 0.222]), without heteroscedasticity (r = −0.003).
Conclusion
The SCVL is a fast and easy to use automated oscillometric device for the determination of ABI. The use of this two-synchronized-cuff device correlates well with the gold standard Doppler ultrasound method and is reproducible. The SCVL may ease the screening for peripheral arterial disease in routine medical practice.
Introduction
The ankle brachial index (ABI) is an indicator of generalized atherosclerosis. In population cohort studies,Citation1 a low ABI has been related to an increased incidence of total and cardiovascular (CV) mortality. The ABI related to increased CV risk has been shown to be independent of baseline CV disease and risk factors, suggesting that the ABI might have an independent role in predicting CV events.Citation2 Also, in a recent meta-analysis it was shown that ABI may improve the accuracy of CV risk prediction beyond the Framingham risk score.Citation3 ABI is the ratio of the systolic ankle blood pressure (BP) divided by the brachial BP. It is useful for the early detection of peripheral arterial disease (PAD) at the physician’s office and also for the assessment of the disease severity.Citation4 Although reliable, inexpensive and rather simple, Doppler-assisted ABI measurement has several limitations, especially in PAD patients in whom distal pulses are missing or difficult to detect by Doppler.Citation5
Then, it requires a degree of expertise that has so far precluded its widespread adoption in primary care. Moreover, the 10% intra observer variabilityCitation6 and the amount of time required to perform Doppler-assisted ABI measurements are found to be a drawback for widespread office-based application. Citation7 Lastly, ABI may be falsely normal or even high due to arterial calcifications in elderly patients and those with diabetes or advanced renal disease.Citation8,Citation9
A test that is automated, easy to perform, and less reliant on specialized skills may facilitate measurement of ABI, and thus the detection of PAD in susceptible populations.Citation10 Automated oscillometric determination of BP is approved for BP measurement and is commonly available, reliable, and simple to use.
The objective of this study was to evaluate the accuracy of the ABI as measured with the screening cardiovascular lab (SCVL®, GenNov, Paris, France), an automated device with synchronized arm and ankle cuffs, in a population of patients presenting at least two CV risk factors.
Methods
Population
A total of 157 consecutive patients with or without prior history of CV disease were included from March to July 2009 at the Cardiovascular Prevention Unit of the Department of Endocrinology and Metabolism at La Pitié-Salpêtrière Hospital in Paris, France. Patients who presented with a recent history of arterial claudication were included if they had not already undergone surgery. The inclusion criteria consisted of having at least two CV risk factors among the following as defined by the European guidelines on cardiovascular preventionCitation11: hypertension, dyslipidemia, diabetes mellitus, current smoking, familial history of premature CV disease, and age >65 years old for females or >55 years old for males. Arterial hypertension was considered present when measurement of brachial BP exceeded 140 mmHg (systolic) and/or 90 mm Hg (diastolic) on at least two different occasions, or if the patient was on antihypertensive medication. Dyslipidemia was defined as a total serum cholesterol level of >5.0 mmol/L, serum low-density lipoprotein (LDL) cholesterol level of >3.0 mmol/L serum high-density lipoprotein (HDL) cholesterol level of <1.0 mmol/L for men or <1.2 mmol/L for women, or serum triglycerides level of >1.7 mmol/L, or as a daily intake of any lipid-lowering medication. Diabetes mellitus was defined by fasting blood sugar levels ≥7.0 mmol/L or HbA1C >6.5%. Additionally, the presence of diabetes mellitus was assumed if the patient was taking any anti-diabetic treatment. Current smoking habits were divided into either current smoking (defined as any cigarette in the last month), never smoked or smoking stopped. Obesity was defined by a body mass index (BMI) >30 kg/m2. Moreover, abdominal obesity was defined by a waist circumference >102 cm in men and >88 cm in women.
Patients underwent complete medical interrogation and physical examination. After 12 hours, fasting blood was sampled to ascertain levels of glucose, total cholesterol, triglycerides, LDL and HDL cholesterol, HbA1C (for diabetic patients) and creatinine. During physical examination, bilateral brachial BP measurements were performed and patients were excluded if the inter-arm BP difference was >10 mmHg for the systolic or the diastolic BP.
ABI measurements
All measurements were made by the same trained operator in a temperature-controlled room where each subject rested supine for 5 minutes and refrained from smoking, heavy exercise, and drinking alcohol or caffeinated beverages for at least 2 hours before measurements were started. ABI measurements were performed as described later with both Doppler assisted and oscillometric techniques in all 157 patients. To avoid a possible effect of the order of measurements, explorations with the SCVL and the Doppler were performed in a random way (using random number tables). ABI was measured on both sides as this has been demonstrated to be more sensitive for detection of PAD.Citation12
Doppler assisted ABI measurement procedure
Doppler-assisted ABI measurements were performed on both sides using an automatic OMRON® HEM-907 sphygmomanometer (Omron Healthcare, Kyoto, Japan) with an upper arm cuff width ranging between 29 cm and 40 cm and a handheld Doppler device with an 8.2 MHz continuous wave. Brachial BP was recorded on the right arm using the OMRON device.
Systolic BP was measured for each leg in the dorsalis pedis and posterior tibial arteries using the Doppler device after placing the cuff just above the ankle. ABI was calculated using a computer by dividing the lower value by the higher brachial systolic BP.
Automated ABI measurement procedure
The SCVL is an automated device driven by the USB ports of any computer and allows the simultaneous determination of BP in the arm and in the ankle with the oscillometric method using two synchronized cuffs (). The cuff for the arm measurement and the pre-shaped cuff for the ankle measurement had bladders with sizes of 24 × 12 cm and 27 × 12 cm, respectively. When the oscillations of pressure in a sphygmomanometer cuff are recorded during gradual deflation, the point of maximal oscillation corresponds to the mean intra-arterial pressure. The oscillation technique allows reliable BP measurements by recording oscillations of the BP during the cuff deflation. The point of maximal oscillation corresponds to the mean intra-arterial pressure and the oscillations begin at approximately systolic BP and continue below diastolic one, so systolic and diastolic BP are estimated indirectly according to the SCVL algorithm. The pressure sensor of the device used to measure systolic BP at the level of the ankle is different from the pressure sensor of the upper arm device to take into account the higher pressure needed to compress the artery against the bone at the level of the ankle. The SCVL is validated for brachial BP measurement according to the protocol of the European Society of Hypertension.Citation13 The oscillometric BP readings were obtained using the SCVL device, first at the right brachial and ankle arteries and then rotated on the other side at the left brachial and ankle arteries. At the ankle level, the oscillometric measure reflects all arterial flow at that level, also including peroneal arteries. ABI was automatically calculated by dividing the ankle value by the higher brachial systolic BP recorded. We computed the SCVL and Doppler obtained ABIs. To ensure reproducibility, two consecutive measurements were performed for each side of each patient. Procedure duration was measured on a sample of 30 patients and lasted about 3 minutes and 57 seconds.
Statistics
Subject characteristics were expressed as means ± SD or frequencies. For comparison between the two methods, we used the ABI as measured by Doppler and the lower of the two SCVL measures using a paired Student’s t test and a two-way analysis of variance (ANOVA). The series of values of calculated indexes were correlated using linear regression. Agreement between the two methods and reproducibility of the SCVL measurement were tested by the Bland-Altman analysis.
An ABI was considered as abnormal when it was strictly <0.90 or strictly >1.30. In other words, the values between 0.851 and 0.899 or between 1.301 and 1.349, often rounded to 0.9 or 1.3 and then considered as normal, here were abnormal.
The data were analyzed with XLSTAT 2010.3 software (Addinsoft, Paris, France). The 95% two-sided confidence interval (CI 0.95) for a prevalence rate was calculated according to the efficient-score method (corrected for continuity) described by Newcombe,Citation14 based on the procedure outlined by Wilson.Citation15
Results
Population characteristics
A total of 157 patients were included in the study. Clinical and biological characteristics are shown in . The mean age of this population was 59.1 years and 51.0% of patients were men. Among the patients 56.8% had treated hypertension, 22.3% were treated for diabetes mellitus, 71.0% had dyslipidemia, 17.6% were current smokers and 50.3% never smoked. Further, 41.2% of patients presented with an abdominal obesity and 36.2% had a familial history of premature CV disease. In our population, 21 patients (13.4%) had a history of prior CV disease and 11 (7.0%) had an already diagnosed PAD.
Table 1 Characteristics of the participants
ABI results
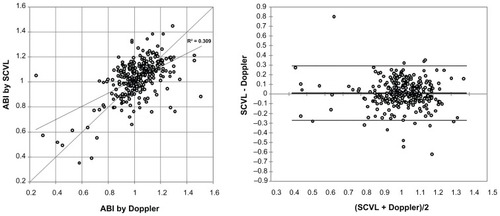
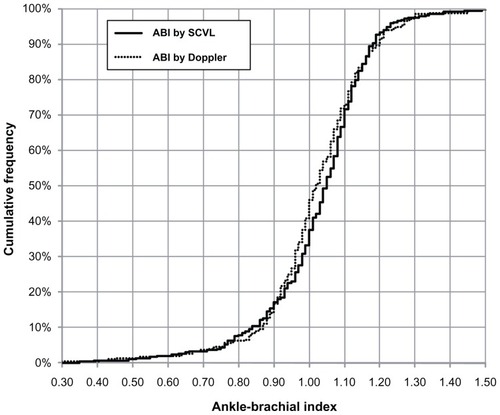
ABI was measured with the two devices in 157 patients and therefore 314 legs. The cumulative distribution of ABI as obtained by the two methods is shown in . The means of all Doppler measured ABI on left and right sides were not different and equal to 1.02 ± 0.16. The coefficient of variation (CV) was 15.8% for the 314 Doppler measures made by one operator. When measured with the SCVL device, mean ABI was 1.04 ± 0.15 on the right side and 1.03 ± 0.16 on the left side for the first measurement. The CV of the SCVL measures was 15.1%. For the second measurement with the SCVL device, ABI was 1.05 ± 0.16 on the right side and 1.04 ± 0.14 on the left side. The paired means did not differ. The two-way ANOVA showed neither interaction, nor side effect, nor method effect. When assessed with the SCVL, 17.2% of the calculated ABI were <0.90 and 2.2% were >1.30. When assessed by Doppler, 16.2% of the calculated ABI were <0.90 and 1.6% were >1.30 as displayed in . The prevalence rates of an abnormal ABI by patient measured with the SCVL or the Doppler, ie, 15.7% (CI 0.95: [11.8; 20.4]) or 14.3% (CI 0.95: [10.7; 18.9]), did not differ. The regression between the two measurements methods was statistically significant: r = 0.56, P < 0.0001. The value to value comparison and the Bland-Altman analysis assessing the agreement of the two methods for all 314 legs also shows a difference of mean equal to 0.010 (CI 0.95: [−0.272; 0.291]) with a correlation coefficient between the difference and the average equal to −0.055 (CI 0.95: [−0.167; 0.059]) rejecting any heteroscedasticity.
Figure 2 Cumulative distribution of ABI as obtained by SCVL® and Doppler.
Correlations between the two methods of measurement are represented in . The average time for measurements were not calculated for the 157 patients but were roughly estimated by the operator inferior to 5 minutes with the SCVL and about more than 10 minutes for the Doppler assisted method.
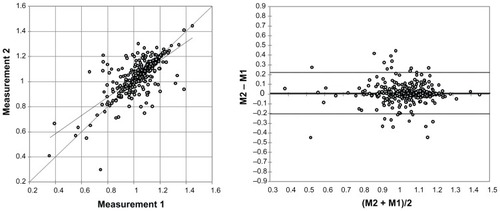
SCVL reproducibility
Correlations between the two measurements of ABI using the SCVL are represented in . A positive correlation between the two measurements was observed: r = 0.71, P < 0.0001. The value to value comparison and the Bland-Altman analysis assessing the agreement of the two measurements for all the 314 legs also shows a difference of mean equal to 0.009 (CI 0.95: [−0.203; 0.222]). The plot and the correlation coefficient between the difference and the average equal to −0.003 (CI 0.95: [−0.117; 0.110]) revealed no systematic trend for heteroscedasticity.
Discussion
In our population of 157 patients, we found a good concordance between ABI as measured by the reference method and ABI as measured by the SCVL. We also found the ABI measurement with the SCVL to be reproducible.
The prevention of CV diseases is based on identification of high risk patients and the presence of a low ABI has been demonstrated to have an independent value in predicting the risk of CV events.Citation2 The reference method for ABI calculation is the Doppler ultrasound method and requires dedicated equipment, training, and is at least a 10–15 minute test with an operator-dependent result. These constraints limit the broad use of ABI in medical practice. A simple, faster, and accurate method should facilitate the ABI evaluation in patients with CV risk factors and will help in the detection of subjects with an augmented risk of CV events.
The SCVL is an automated device using two synchronized cuffs to determine ABI. It showed good measurement reproducibility in our study. When compared to the reference method for assessing ABI, the regression analysis showed a strong correlation between the two methods and the Bland-Altman analysis indicated only a small difference between values. Furthermore, this new automated method has a strong correlation with the standard manual Doppler method in classified subjects with an abnormal ABI. One major advantage of this new method is its ease of use, as it does not need special equipment (such as a Doppler probe) and requires only very minimal user training. It is also a much faster measurement than the standard Doppler method. The use of a single device with two automatically synchronized cuffs rather than sequential BP measurements using the user-dependent Doppler methods is also a major advantage. Because of these reasons, the SCVL will help to extend the number of ABI assessments in routine clinical practice.
In our population, the prevalence of PAD as defined by the determination of an ABI < 0.90 or > 1.30 was 15.7% according to measurements made by the SCVL device and 14.3% according to the Doppler method. Prevalence of PAD varies across populations based on the groups and the detection methods used. Studies have shown that measuring the ABI in patients above the age of 70 or above the age of 50 in patients with diabetes or smokers should yield a positive rate of approximately 29%.Citation16 In unselected patients above the age of 65, disease prevalence approaches 20%Citation17 and would be closer to 10% between 40 and 60 years of age in studies using Doppler measurements of ABICitation18 or in lipid clinics.Citation19 Diabetes and tobacco are the main causes of PAD among the different major CV risk factors and our population counted only 50% of current or former smokers, 22% of diabetics whereas 57% of our patients presented with hypertension and 71% with dyslipidemia. This can explain the relatively low prevalence of PAD in our population compared to the PARTNERS Study.Citation16
Our results confirm previous studies that have found that oscillometric measurements are a useful tool for assessment of ABI. A study involving patients recruited in office practice studies showed a sensitivity of 73% or 88% and a specificity of 85% or 95% for detection of PAD using oscillometric methods.Citation10 Another study where subjects were recruited in a cardiology department demonstrated a sensitivity of 73% and specificity of 95% when compared to the reference Doppler assisted ABI measurement.Citation20 Accordingly, the oscillometric measurement of ABI is appropriate in such population.
Limitations of this study are as follows. It is an observational study on a selected population of patients who do not reflect the general population but is still characteristic of the target population in which PAD should be detected.Citation21
In conclusion, our study demonstrated that the automated determination of ABI using the SCVL, an automated device with two synchronized cuffs, correlates well with the reference Doppler ultrasound method. Because of the quick and easy procedure for ABI determination using the SCVL device, it is possible to imagine that, after validation by larger randomized trials and cost effective analysis, a greater number of ABI measurements could be performed in asymptomatic subjects with CV risk factors, a population in which ABI evaluation is recommended but is not currently realized in medical practice.
Acknowledgments
We gratefully acknowledge the expert assistance of Uwe Diegel in the development of the SCVL device.
Disclosure
There was no funding for this study. DR, SR-C, EB, PG, and XG have no conflicts of interest with the SCVL manufacturer. PL is a co-founder of GenNov, the SCVL manufacturer. The authors declare no other conflicts of interest in this work.
References
- LaminaCMeisingerCHeidIMAssociation of ankle-brachial index and plaques in the carotid and femoral arteries with cardiovascular events and total mortality in a population-based study with 13 years of follow-upEur Heart J200627212580258716952925
- DoobayAVAnandSSSensitivity and specificity of the ankle-brachial index to predict future cardiovascular outcomes: a systematic reviewArterioscler Thromb Vasc Biol20052571463146915879302
- Ankle Brachial Index CollaborationAnkle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysisJAMA2008300219720818612117
- NorgrenLHiattWRDormandyJAInter-society consensus for the management of peripheral arterial disease (TASC II)Eur J Vasc Endovasc Surg200733Suppl 1S17517140820
- MohlerER3rdTreat-JacobsonDReillyMPUtility and barriers to performance of the ankle-brachial index in primary care practiceVasc Med20049425326015678616
- Holland-LetzTEndresHGBiedermannSReproducibility and reliability of the ankle-brachial index as assessed by vascular experts, family physicians and nursesVasc Med200712210511217615798
- DiehmNDickFCzuprinCLawallHBaumgartnerIDiehmCOscillometric measurement of ankle-brachial index in patients with suspected peripheral disease: comparison with Doppler methodSwiss Med Wkly200913925–2635736319562530
- NeubauerBA quantitative study of peripheral arterial calcification and glucose tolerance in elderly diabetics and non-diabeticsDiabetologia1971764094135144548
- IxJHKatzRDe BoerIHAssociation of chronic kidney disease with the spectrum of ankle brachial index the CHS (Cardiovascular Health Study)J Am Coll Cardiol200954131176118419761940
- BeckmanJAHigginsCOGerhard-HermanMAutomated oscillometric determination of the ankle brachial index provides accuracy necessary for office practiceHypertension2006471353816344373
- GrahamIAtarDBorch-JohnsenKEuropean guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts)Eur J Cardiovasc Prev Rehabil200714Suppl 2S111317726407
- McDermottMMCriquiMHLiuKLower ankle/brachial index, as calculated by averaging the dorsalis pedis and posterior tibial arterial pressures, and association with leg functioning in peripheral arterial diseaseJ Vasc Surg20003261164117111107089
- BelghaziJEl FeghaliRNMoussalemTRejdychMAsmarRGValidation of four automatic devices for self-measurement of blood pressure according to the International Protocol of the European Society of HypertensionVasc Health Risk Manag20073438940017969368
- NewcombeRGTwo-sided confidence intervals for the single proportion: comparison of seven methodsStat Med19981788578729595616
- WilsonEBProbable inference, the law of succession, and statistical inferenceJASA192722209212
- HirschATCriquiMHTreat-JacobsonDPeripheral arterial disease detection, awareness and treatment in primary careJAMA2001286111317112411560536
- BirdCECriquiMHFronekADenenbergJOKlauberMRLangerRDQuantitative and qualitative progression of peripheral arterial disease by non-invasive testingVasc Med199941152110355865
- MeijerWTHoesAWRutgersDBotsMLHofmanAGrobbeeDEPeripheral arterial disease in the elderly: The Rotterdam StudyArterioscler Thromb Vasc Biol19981821851929484982
- CriquiMHFronekAKlauberMRBarrett-ConnorEGabrielSThe sensitivity, specificity, and predictive value of traditional clinical evaluation of peripheral arterial disease: results from non-invasive testing in a defined populationCirculation19857135165223156007
- BenchimolABernardVPilloisXHongNTBenchimolDBonnetJValidation of a new method of detecting peripheral artery disease by determination of ankle-brachial index using an automatic blood pressure deviceAngiology200455212713415026866
- HirschATHaskalZJHertzerNRACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease FoundationCirculation200611311e463e65416549646