Abstract
High blood pressure and lipoprotein abnormalities were identified by many cohort studies as the major risk factors for cardiovascular disease. Laboratory experiments apparently confirmed their role in the causation of atherosclerosis, but a proof of concept requires the corroboration by clinical trials in human beings. The size of benefit in clinical trials regarding the control of high blood pressure was within the estimations of risk provided by cohort studies. For a reduction of 10 mmHg in systolic blood pressure or 5 mmHg in diastolic blood pressure, the relative risk reduction of coronary heart disease was 22% (95% confidence interval 27%–17%) in a meta-analysis of clinical trials, close to the estimation of reduction of 25% (95% confidence interval 23%–27%) provided by a meta-analysis of cohort studies. The corresponding values for stroke were 41% (95% confidence interval 33%–48%) in clinical trials compared to a cohort risk prediction of 36% (95% confidence interval 34%–38%). This efficacy was shared by all blood pressure-lowering drugs. The same figure has not paradoxically happened with drugs that act over abnormalities of cholesterol and lipoproteins. Only statins, which have other beneficial actions as well, have consistently lowered the incidence of cardiovascular diseases, an efficacy that was not reproduced by older and newer quite potent lipid drugs. The adverse effects of these drugs may nullify their beneficial effects over lipoproteins and abnormalities of lipoproteins may only be surrogate markers of the underlying real risks.
Introduction
Classic cohort studies identified high blood pressure and blood lipids abnormalities as major risk factors for cardiovascular disease. Nonetheless, their role in the causation of cardiovascular disease – the proof of concept – requires corroboration by clinical trials. Findings from clinical trials regarding the control of high blood pressure have been consistent with the estimations of risk provided by cohort studies, but the same has not paradoxically happened with drugs that act on abnormalities of cholesterol and lipoproteins. In this descriptive review, the key studies of risk and benefit of treatment that support this view are presented.
Risks of blood pressure
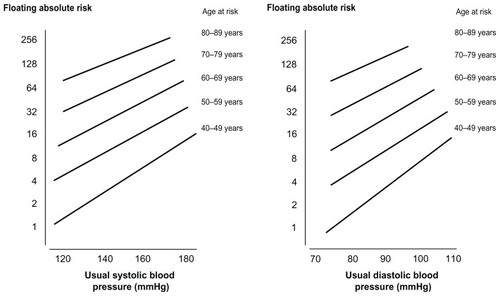
The meta-analysis of 61 cohort studies by the Prospective Studies Collaboration group,Citation1 with more than 1 million individuals at risk and with more than 53,000 fatal strokes and coronary events during a follow-up of more than 15 years, identified that the risks start at blood pressure values as low as 115/75 mmHg, doubling at each 20 mmHg of systolic blood pressure or 10 mmHg of diastolic blood pressure (). The play of chance was probably close to null in face of the large number of individuals included in the meta-analysis, and selection and measurement bias of the individual studies were essentially diluted as well.
Figure 1 Absolute risk for coronary heart disease by age and usual systolic and diastolic blood pressure.
Reproduced with permission from The Lancet, Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–1913.Citation1 Copyright 2002, with permission from Elsevier.
Risks of lipid abnormalities
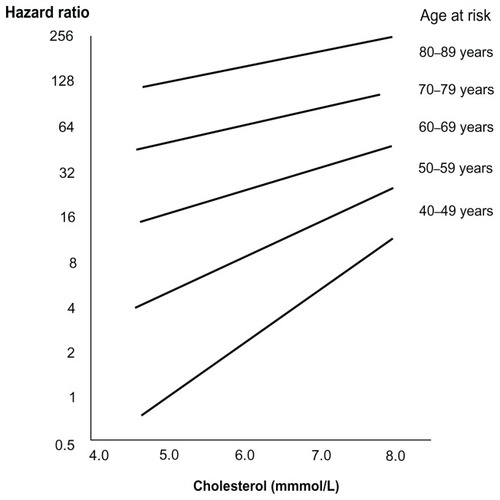
Using a methodology similar to the blood pressure meta-analysis, the investigators of the Prospective Studies Collaboration analyzed the association of cholesterol and lipoproteins with deaths by coronary heart disease (CHD) and stroke, based on 61 cohort studies, with almost 900,000 adults and with more than 55,000 vascular deaths in the follow-up.Citation2 The association between cholesterol levels with the incidence of CHD deaths was exponential, continuous, and observed at all age groups, reproducing the findings of blood pressure (). Low-density lipoprotein cholesterol (LDL-C) was positively associated, and high-density lipoprotein cholesterol (HDL-C) was inversely associated, with the incidence of coronary events. Differently from blood pressure, which was a risk for CHD and stroke, cholesterol levels (and fractions) were not associated with the incidence of stroke, particularly among individuals with high blood pressure and older ages.
Figure 2 Absolute risk for coronary heart disease by age and serum cholesterol levels.
Reproduced with permission from The Lancet, Lewington S, Whitlock G, Clarke R, et al; Prospective Studies Collaboration. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007;370(9602):1829–1839.Citation2 Copyright 2007, with permission from Elsevier.
Requirements for a proof of concept
Despite the robust evidence, observational studies are not sufficient to provide a proof of concept since it is not possible to control for many potential biases on the relationship between exposures and events. Some confounding factors were controlled by stratification and statistical modeling, but others were difficult to measure or were not addressed in all studies, such as genetic traits, psychosocial characteristics, and other unknown confounders. Some characteristics may be only surrogates of risks and not the real risks. Only experiments can provide the proof of concept. Since human beings cannot be experimentally exposed to potential risks or causes for diseases, the proof of concept can be given only by indirect experiments, which try to demonstrate if diseases are prevented by removal or antagonism of potential risks.
Most, but not all, risks and benefits identified in observational studies have been corroborated by clinical trials. The prevention of cardiovascular disease by hormone replacement therapy after menopause, demonstrated in cohort studies and not confirmed by clinical trials, is a noticeable example.Citation3,Citation4
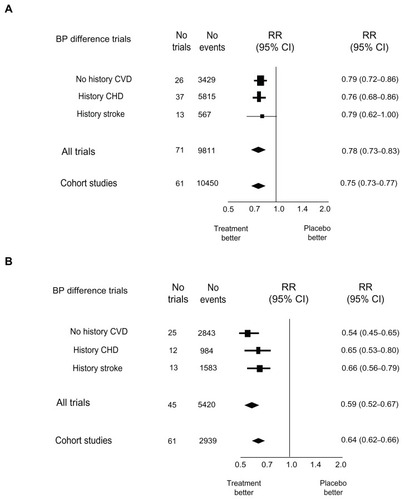
Proof of concept for hypertension
The causal role of high blood pressure for cardiovascular disease was fully confirmed by clinical trials. Compiling more than a hundred clinical trials, Law and associates demonstrated the robust association between lowering of blood pressure and the prevention of CHD and stroke.Citation5 The summary estimate and confidence intervals (CI) for the prevention of CHD (relative risk 0.78, 95% CI: 0.73–0.83) were almost those predicted by the cohort meta-analysis (relative risk 0.75, 95% CI: 0.73–0.77) ().Citation1 For stroke, the evidence was similar but of higher magnitude in face of the higher risk of blood pressure for cerebrovascular events (relative risk 0.59, 95% CI: 0.52–0.67) in the meta-analysis of the clinical trials in comparison with that predicted by the cohort meta-analysis (relative risk 0.64, 95% CI: 0.62–0.66) ().Citation1 All drugs tested in the trials lowered the incidence of cardiovascular events with slight variation between them, demonstrating that their blood pressure-lowering properties, and not pleiotropic effects, were responsible for cardiovascular protection.
Figure 3 Relative risk for (A) coronary heart disease and (B) stroke by standardized difference (10 mmHg of systolic blood pressure or 5 mmHg of diastolic blood pressure) between clinical trial arms in patients with and without previous cardiovascular disease, and the size effect prediction from cohort studies.
Reproduced with permission from BMJ Publishing Group Limited. Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665.Citation5 Copyright 2009.
Lack of proof of concept for lipid abnormalities
A proof of evidence similar to that provided for the risks of high blood pressure was still not yielded for abnormalities of cholesterol and lipoproteins. Many drugs that are effective in improving the lipid profile did not lead to the expected reduction in the incidence of cardiovascular disease. The attempt to demonstrate the efficacy of the first lipid-lowering agents to prevent cardiovascular events in pioneering clinical trials was frustrating. Finnish executives with high risk of suffering a cardiovascular event and submitted to a multifactorial intervention, which included the use of probucol, clofibrate, or niacin, had higher incidence of CHD in comparison with participants randomized to usual care. The harmful effect of intervention persisted for 10 years after concluding the experimental phase.Citation6 In the Lipid Research Clinic trial, the prevention of CHD in patients treated with cholestyramine reached statistical significance only with the use of a controversial one-sided alpha error test.Citation7 Niacin was the only agent tested in the Coronary Drug Project that showed a trend for efficacy.Citation8 A meta-analysis of 22 trials showed that old lipid-lowering agents failed to prevent cardiovascular events.Citation9 Moreover, older lipid drugs were associated with higher risk for mortality by accidents and violence,Citation10 leading to the discredit of the beneficial effects of lipid-lowering interventions at that point in time.Citation11
The efficacy of statins to prevent cardiovascular events seemed to have settled the controversy about the effectiveness of lipid-lowering drugs to prevent cardiovascular disease, since they reduced the incidence of CHD mortality by 30% and total mortality by 12%.Citation12 A similar protection against stroke was somewhat unexpected, since higher cholesterol is not an evident risk factor for cerebrovascular events.Citation13 A recent meta-analysis done by investigators of the authors’ institute employed an innovative approach – mixed treatment comparisons – to compare the efficacy of different doses of statins.Citation14 Based on the results of 47 clinical trials, totalizing 175,232 patients, they demonstrated that intermediate and higher doses were more efficacious in the prevention of cardiovascular events than lower doses. On the other hand, larger doses were not superior to prevent against cardiovascular mortality. The efficacy of statins in the primary prevention of cardiovascular events in patients with low risk has been questioned because of the inclusion of people with cardiovascular disease in some primary prevention trials.Citation15 Many putative beneficial effects of statins have not been confirmed.Citation16,Citation17
The inefficacy of newer lipid-lowering agents introduced after statins renewed the uncertainty about the cardiovascular risks of higher cholesterol and other lipid abnormalities. Despite their intense effect over lipoproteins, newer drugs have failed to prevent major and surrogate cardiovascular outcomes. Torcetrapib increased HDL-C by 60% and reduced LDL-C by 20% (in addition to the effect obtained with a statin), but increased total mortality by 58%.Citation18 Ezetimibe reduced LDL-C by approximately 16% in addition to the effect of statins, but failed to reduce the carotid intima-media thickness in patients with familial hypercholesterolemia.Citation19 Compared to niacin, ezetimibe did not reduce carotid intima–media thickness and was associated with higher incidence of cardiovascular outcomes. Citation20 Fenofibrate, another agent with moderate effect over cholesterol and intense effect over triglycerides, failed to prevent major cardiovascular events in patients with type 2 diabetes.Citation21 The dissociation between the effect of drugs over cholesterol and fractions and over clinical outcomes is shown in .
Table 1 Effect of agents that interfere on lipid metabolism and consequences on surrogate and hard outcomes. Based on data from previous studiesCitation8,Citation12,Citation18–Citation21
Explanations for the beneficial effects of statins and maybe niacin and for the null or harmful effects of other agents have been presented. The size and precocious benefits of statins suggested they could act by other mechanisms, which were also aggregated under the denomination of pleiotropic effects.Citation22 A blood pressure-lowering effect of statins has been suggested as well.Citation23 In clinical trials, statins decreased cardiovascular outcomes to the same extent in hypertensive and nonhypertensive patients,Citation24 but the benefit of blood pressure-lowering effect has been identified in patients without hypertension as well.Citation25
The deleterious effects of torcetrapib were attributed to the increase of blood pressure by 4/2 mmHg during the course of the ILLUMINATE (Investigation of Lipid Level Management to Understand its Impact in Atherosclerotic Events) trial.Citation18 Anacetrapib, a newer cholesteryl ester transfer protein inhibitor free of the blood pressure-increasing effect, was tested in a small safety trial.Citation26 LDL-C was lowered by 39.8%, while HDL-C increased by 138.1% beyond that seen in the placebo group. Blood pressure and adverse events did not rise in participants treated with anacetrapib and there was no beneficial trend for prevention of clinical events, despite the huge effect over lipoproteins. The beneficial effects of niacin could also be secondary to its blood pressure-lowering properties, identified in a post hoc analysis of a lipid trial.Citation27
On the other hand, the absence of benefit of most lipid-lowering drugs may be secondary to the complex relationship between blood lipid abnormalities and vascular risk. In comparing the contribution of hypertension to cardiovascular events, the effect of circulation lipid on the cardiovascular system is more complicated and it is the nature of the complexity that determines the difficulty of drug development. Other factors may also share the deleterious pathway that lipid causes cardiovascular damage. The idea that the correction of such abnormalities would lead to the prevention of cardiovascular disease may be quite simplistic, and innovative approaches to control lipid abnormalities may be required.
Conclusion and perspective
The evidence of risks of high blood pressure and the consistent reduction of such risks by clinical trials of blood pressure-lowering agents are robust proofs of the concept that high blood pressure is a major cardiovascular risk. The lack of equivalent evidence with drugs that lower cholesterol (and LDL-C) or increase HDL-C leads to two interpretations: (1) adverse events of these drugs nullify their beneficial effects over lipoproteins, or (2) abnormalities of lipoproteins are only surrogate markers of the underlying real risks. In any case, drugs cannot be indicated to prevent cardiovascular events based exclusively on their effects over lipoproteins.
Acknowledgments
This study was supported, in part, by the National Institute of Science and Technology for Health Technology Assessment (IATS) – CNPq/Brazil.
Disclosure
The authors report no conflicts of interest in this work.
References
- LewingtonSClarkeRQizilbashNPetoRCollinsRAge-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studiesLancet200236093491903191312493255
- LewingtonSWhitlockGClarkeRProspective Studies CollaborationBlood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deathsLancet200737096021829183918061058
- GradyDHerringtonDBittnerVCardiovascular disease outcomes during 6.8 years of hormone therapy: Heart and Estrogen/progestin Replacement study follow-up (HERS II)JAMA20022881495712090862
- RossouwJEAndersonGLPrenticeRLRisks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trialJAMA2002288332133312117397
- LawMRMorrisJKWaldNJUse of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studiesBMJ2009338b166519454737
- StrandbergTESalomaaVVNaukkarinenVAVanhanenHTSarnaSJMiettinenTALong-term mortality after 5-year multifactorial primary prevention of cardiovascular disease in middle-aged menJAMA19912669122512291870247
- Lipid Research Clinics ProgramThe Lipid Research Clinics Coronary Prevention Trial results. I. Reduction in incidence of coronary heart diseaseJAMA198425133513646361299
- Coronary Drug ProjectClofibrate and niacin in coronary heart diseaseJAMA197523143603811088963
- RavnskovUCholesterol lowering trials in coronary heart disease: frequency of citation and outcomeBMJ1992305684415191638188
- MuldoonMFManuckSBMatthewsKALowering cholesterol concentration and mortality: a quantitative rewiew of primary prevention trialsBMJ199030167473093142144195
- OliverMFPrevention of coronary heart disease – propaganda, promises, problems, and prospectsCirculation1986731193510083
- BrugtsJJYetginTHoeksSEThe benefits of statins in people without established cardiovascular disease but with cardiovascular risk factors: meta-analysis of randomised controlled trialsBMJ2009338b237619567909
- PaciaroniMBogousslavskyJStatins and stroke preventionExpert Rev Cardiovasc Ther20097101231124319814666
- RibeiroRAZiegelmannPKDuncanBBImpact of statin dose on major cardiovascular events: a mixed treatment comparison meta-analysis involving more than 175,000 patientsInt J Cardiol12202011 [Epub ahead of print.]
- TaylorFWardKMooreTHStatins for the primary prevention of cardiovascular diseaseCochrane Database Syst Rev20111CD00481621249663
- ShafiqNMalhotraSPandhiPGroverAThe “Statinth” wonder of the world: a panacea for all illnesses or a bubble about to burstJ Negat Results Biomed20054315788096
- RahimiKMajoniWMerhiAEmbersonJEffect of statins on ventricular tachyarrhythmia, cardiac arrest, and sudden cardiac death: a meta-analysis of published and unpublished evidence from randomized trialsEur Heart J232012 [Epub ahead of print.]
- BarterPJCaulfieldMErikssonMILLUMINATE InvestigatorsEffects of torcetrapib in patients at high risk for coronary eventsN Engl J Med2007357212109212217984165
- KasteleinJJPAkdimFStroesESGENHANCE InvestigatorsSimvastatin with or without ezetimibe in familial hypercholesterolemiaN Engl J Med2008358181431144318376000
- TaylorAJVillinesTCStanekEJExtended-release niacin or ezetimibe and carotid intima-media thicknessN Engl J Med2009361222113212219915217
- GinsbergHNElamMBLovatoLCACCORD Study GroupEffects of combination lipid therapy in type 2 diabetes mellitusN Engl J Med2010362171563157420228404
- DavignonJBeneficial cardiovascular pleiotropic effects of statinsCirculation200410923 Suppl 13943
- CorreaVJrGusMFuchsFDDoes the blood pressure-lowering effect of statins contribute to their beneficial cardiovascular effects?Expert Rev Cardiovasc Ther20108677577920528635
- MesserliFHPintoLTangSSImpact of systemic hypertension on the cardiovascular benefits of statin therapy – a meta-analysisAm J Cardiol2008101331932518237593
- ThompsonAMHuTEshelbrennerCLReynoldsKHeJBazzanoLAAntihypertensive treatment and secondary prevention of cardiovascular disease events among persons without hypertension: a meta-analysisJAMA2011305991392221364140
- CannonCPShahSDanskyHMSafety of anacetrapib in patients with or at high risk for coronary heart diseaseN Engl J Med2010363252406241521082868
- BaysHEMaccubbinDMeehanAGKuznetsovaOMitchelYBPaoliniJFBlood pressure-lowering effects of extended-release niacin alone and extended-release niacin/laropiprant combination: a post hoc analysis of a 24-week, placebo-controlled trial in dyslipidemic patientsClin Ther200931111512219243712