Abstract
Peripheral arterial disease (PAD) generally remains under-recognized, mainly due to the specialized technical skills required to detect the low values of the ankle-brachial index (ABI). As a simpler and faster alternative to the standard method using continuous-wave Doppler ultrasound, we evaluated automated oscillometric ABI measurement by VP-2000 with an elderly cohort of 113 subjects (age range, 61 to 88 years). The standard deviation in ABIs measured by the Doppler method was statistically greater than that measured by the oscillometric method for each of the two legs (P < 0.001). Correlations in ABIs between the two methods were 0.46 for the left leg and 0.61 for the right leg; this result appears to have been caused by interobserver variation in the Doppler ABI measurements. While the trend showing greater differences between average oscillometric- and Doppler-ABIs was significant at the lower ABI ranges, there was little indication of differences in measurements having an average ABI > 1.1. The difference between the methods was suggestively larger in subjects who were smokers than in non-smokers (P = 0.09), but the difference was not affected by other potential atherosclerotic risk factors, including age at examination (P > 0.50). A larger difference at lower ABIs led to better PAD detection by the Doppler method compared to the oscillometric method (sensitivity = 50%, specificity = 100%), although the overall agreement was not small (Cohen’s Kappa = 0.65). Our findings indicate that oscillometric devices can provide more accurate estimation of the prevalence of PAD in elderly individuals than the conventional Doppler method.
Introduction
Peripheral arterial disease (PAD) is a common atherosclerotic condition among elderly Japanese individuals: 5% of men aged 60 to 79 years,Citation1 and 3.4% of men and women aged 65 years or greater are affected by the disease.Citation2 Diagnosis of PAD has important prognostic implications in reducing cardiovascular morbidity and mortality. Half of patients remain undiagnosed,Citation3 given that asymptomatic PAD is common and is independently associated with impaired lower extremity functioning,Citation4 especially in elderly populations.Citation5 Although intermittent claudication has been considered the most classic manifestation of PAD, recent data show that most PAD cases do not have classic intermittent claudication symptoms.Citation6,Citation7 Moreover, many PAD patients also have arthritis or back ailments, which might also cause exertional leg pain.Citation4 A more accurate estimation of the prevalence of PAD in the elderly should rely upon a validated and reproducible test, such as the ankle-brachial index (ABI). One of the barriers to recognition of PAD is the time-consuming skill acquisition required of the examiner applying the Doppler method, the gold standard for ABI testing.Citation8 As a simple and fast alternative to facilitate disease diagnosis, several investigators have reported the feasibility of oscillometric-ABI in epidemiological settings among middle-aged subjects,Citation9 and in general EuropeanCitation10 and American populations.Citation11 Recent studies indicate that the VP-2000 (Omron Healthcare, Kyoto, Japan), an automated oscillometric device, can provide accurate ABI measurements with minimal examiner technical skill.Citation9,Citation10 The US Food and Drug Administration has approved the VP-2000 device for clinical use.Citation10 To our knowledge, however, few studies have evaluated the use of oscillometric-ABI among elderly subjects, in which ankle systolic blood pressure (SBP) may not be accurately measured when arterial blood flow cannot be abolished by inflation of an air-filled blood pressure cuff.Citation12 The aim of the current study was to validate oscillometric-ABI using the VP-2000 on elderly patients in an epidemiological setting.
Methods
Subjects
The Adult Health Study (AHS) cohort at the Radiation Effects Research Foundation (RERF) consists of atomic-bomb survivors who have undergone biennial health examinations since 1958. Between January 11 and February 29, 2008, 115 subjects provided written informed consent prior to their participation in this validation study at the Hiroshima laboratory. The study protocol was approved by the RERF ethics committee.
Measurements of ankle and brachial blood pressures
ABI is the ratio of SBP at the ankle to that in the arm. To obtain ABIs, trained technicians measured SBPs on subjects in the supine position in a quiet room after the subjects had rested for 10 minutes. Participants had been instructed to abstain from smoking and drinking, except for water, for at least two hours prior to the examination. ABI was measured twice on each participant by one of seven randomly assigned technicians using two methods, the oscillometric and Doppler methods, on both the subjects’ left and right legs. The oscillometric-ABI was calculated as the ratio of ankle SBP to the highest of the right and left brachial SBPs. For the Doppler-ABI, SBP was measured twice at the right brachial and the right and left posterior tibial arteries with a handheld 5-MHz Doppler probe (MedaSonics 5 MHz Doppler Ultrasound Stethoscope, model BF4B, MedaSonics, Fremont, CA). As commonly used as a diagnostic criterion for PAD, we classified ABI <0.90 as low. Two subjects with Doppler-ABI ≥1.4 were excluded from the analysis because such results usually reflect arterial rigidity preventing arterial compression, leaving 113 subjects for the subsequent analyses. The intraclass correlation coefficients for interobserver agreements were 0.95 in the Doppler-ABI and 0.80 in the oscillometric-ABI, and intraobserver agreements were 0.71 in the Doppler-ABI and 0.87 in the oscillometric-ABI.
Atherosclerotic risk factors and cardiovascular disease
We obtained patient information for the factors that could potentially influence SBP measurements. The subjects’ smoking and drinking habits were obtained from medical interviews. Hypertension (HT) was defined as an auscultatory SBP/DBP of ≥140/90 mmHg, or under treatment for HT. Hyperlipidemia (HLp) was defined as a serum cholesterol level of ≥220 mg/dL or under treatment for HLp. Diabetes mellitus (DM) was defined as a casual plasma glucose level of ≥200 mg/dL, or under treatment with oral hypoglycemic agents. Cardiovascular disease (CVD) was defined as evidence of ischemic changes on a 12-lead ECG, or a history of coronary bypass surgery, coronary angioplasty, or stroke. Body mass index (BMI, kg/mCitation2) was calculated from the patient’s height and weight at the examination.
Statistical analysis
Standard deviation of the ABI measurements between the oscillometric and Doppler methods was compared by the F-test. To assess the agreement in measurements by the two methods, we conducted linear regression analyses for the difference of the two measurements within each individual, and the pattern of the agreement was graphically assessed by a Bland-Altman plot.Citation14 In the regression analyses, we evaluated variations in the differences due to other factors — smoking and drinking habits, HT, DM, CVD, HLp and BMI — with or without adjustment by the examiners (assumed to be normally distributed with mean zero). In addition to separate analyses for the right and left legs, we performed combined data analyses for both legs with random effects to account for within-individual correlations between the left and right leg measurements. All presented P-values are two-sided. The agreement in PAD diagnosis (ABI < 0.9) between the methods was checked with Cohen’s Kappa statistic, as well as sensitivity and specificity, using the Doppler measurement as the gold standard. Conventionally, a Cohen’s Kappa statistic of <0.2 is considered poor agreement, 0.21–0.4 fair, 0.41–0.6 moderate, 0.61–0.8 strong, and >0.8 is considered near complete agreement.
Results
Among the 113 study participants, mean ages (standard deviation [SD]) were 73.9 years (8.1) for women and 70.0 years (7.6) for men. presents the distribution of the study subjects by selected characteristics with means (SD) of ABIs measured by the two methods. The standard deviation in ABIs measured by the Doppler method was statistically larger than that measured by the oscillometric method for each of the two legs (P < 0.001). Correlations in ABIs between the two methods were 0.46 for the left leg and 0.61 for the right leg. Doppler ABIs tended to vary significantly by examiner (P = 0.006 for the right leg and P = 0.02 for the left leg), while the examiner effect was not significant in oscillometric-ABIs (P > 0.5 for each leg).
Table 1 Mean ankle brachial index (ABI) measurements and the difference between oscillometric and Doppler methods in the study subjects by selected characteristics
Without any adjustment, the level of the oscillometric ABIs was significantly greater than that for the DopplerABIs for right legs (95% CI = 0.02–0.06, P < 0.001), while the difference was not significant in left legs (−0.01; 0.04, P = 0.31). The difference between the two methods appeared to vary significantly over the subgroups by examiner (P < 0.001 for both legs). With adjustment for examiners, the significance of the difference was reduced (P = 0.04 in the right leg and P = 0.15 in the combined analysis). While the difference between the methods might be larger among smokers than non-smokers (P = 0.07 in the left leg and P = 0.09 in the combined analysis), there was no evidence for variations in the difference over the other clinical condition categories, including age at examination (P > 0.5).
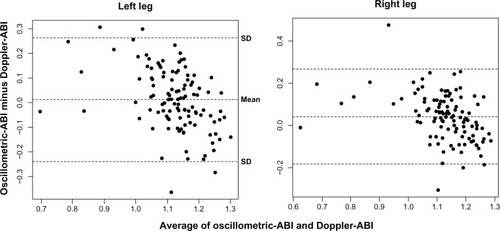
The Bland-Altman plot in indicates that the oscillometric-ABI tended to yield larger values than the Doppler-ABI for those individuals with relatively smaller ABI averages on both legs. This trend of the difference decreasing with average was significant, with a coefficient of —0.55 for the left leg and −0.41 for the right leg (P < 0.001 for both legs); however, there was little indication of difference among those having average ABI > 1.1 (P > 0.1 for each leg).
The Doppler method detected 10 subjects with low-ABI (<0.9) in either leg, among which, 5 had measurements below the cutoff by oscillometric-ABI (<0.9). There was no over-diagnosis by the oscillometric method compared to the Doppler method, thus, specificity = 100% and sensitivity = 50%. Despite the small sensitivity, no strong overall disagreement in diagnosis was indicated by Kappa measures (ê = 0.65 (95% CI = 0.40–1.0), conventionally considered strong agreement). When we also tested agreement between the two methods using the worst legs based on ABIs, sensitivity = 40% and Kappa = 0.55 (95% CI = 0.20–0.90).
Discussion
Peripheral artery disease generally remains under-recognized, which has been a limiting factor in the reduction of cardiovascular morbidity and mortality in these patients. This is mainly due to the specialized skills required by technicians to detect low ABI values using the gold-standard method of continuous-wave Doppler ultrasound. To examine a potential simple and fast alternative,Citation15 we evaluated automated oscillometric-ABI measurement using a cohort of elderly individuals in Japan.
Consistent with many other studies,Citation10,Citation11,Citation16–Citation19 our observations indicate that the mean oscillometric-ABI value using the VP-2000 might be higher compared to the Doppler counterpart, particularly at lower-range ABIs. While this might be attributed to the intrinsic differences in the oscillometric and Doppler blood pressure measurement techniques, our analysis demonstrated that deviation in the difference was explained, to some extent, by variation in the Doppler measurements due to interexaminer differences. In contrast, the oscillometric method was not affected by the examiner. It is also worth noting that, in our analysis, the difference was not affected by age, which indicates that use of the oscillometric method may not be limited by the age of the patient.
The reliability of automated oscillometric-ABI values for PAD diagnosis is controversial. As in many other studies,Citation16,Citation18,Citation19 we found that the automated oscillometric device led to a conservative detection of PAD compared to the Doppler method, as a result of the differences at lower ABIs. Beckman et alCitation11 and Kollias et alCitation15 concluded that oscillometric devices could provide a reliable and simple method of PAD detection with relatively good agreement with the Doppler method. Another recent study reported poor agreement in PAD diagnosis between primary care facilities and vascular laboratories (ê, 0.41); over-diagnosis of PAD was made in primary care facilities compared with vascular laboratories, and over 60% of cases were assessed by a Doppler device in primary care.Citation17
In our analysis, the agreement between the two methods for detecting PAD was not good (sensitivity = 50%) if PAD was diagnosed for ABI <0.9. Due to the limited number of PAD cases detected in this study (10 by the Doppler method and 5 by the oscillometric method), rationalizing this diagnostic disagreement is not straightforward. Our observed pattern of differences suggests that raising the cutoff level should facilitate an improvement in the screening of PAD by oscillometric devices. For example, when an oscillometric-ABI of less than 1.0, instead of 0.9, was considered low, the agreement somewhat improved with sensitivity = 60%, specificity = 97%. In this cohort, the PAD prevalence generally reported for Japanese elderly populations (3%–5%)Citation1, Citation2 was closer to the observed prevalence by the oscillometric method (4.4%) than that by the Doppler method (8.8%). That evidence, together with our findings of increased variability in Doppler measurements, indicates that the oscillometric-ABI may not necessarily be inefficient in detecting PAD compared with Doppler-ABI. Further comparison between Doppler and oscillometric tools among known PAD patients is necessary because, in the current study, few subjects had low ABIs.
In conclusion, the oscillometric method to measure ABI using the VP-2000 can provide more accurate estimation of the prevalence of PAD, independent of the examiner’s skill, than the conventional Doppler method, and may be beneficial in reducing the health burden of this condition in the elderly population.
Acknowledgment
The Radiation Effects Research Foundation (RERF), Hiroshima and Nagasaki, Japan is a private, non-profit foundation funded by the Japanese Ministry of Health, Labour and Welfare (MHLW) and the US Department of Energy (DOE), the latter in part through DOE Award DE-HS0000031 to the National Academy of Sciences. This publication was supported by RERF Research Protocols RP2–75 and 7–09. The views of the authors do not necessarily refect those of the two governments.
Disclosure
The authors report no conflicts of interest in this work.
References
- CuiRIsoHYamagishiKAnkle-arm blood pressure index and cardiovascular risk factors in elderly Japanese menHypertens Res200326537738212887128
- FujiwaraTSaitohSTakagiSPrevalence of asymptomatic arteriosclerosis obliterans and its relationship with risk factors in inhabitants of rural communities in Japan: Tanno-Sobetsu studyAtherosclerosis20041771838815488869
- HirschATCriquiMHTreat-JacobsonDPeripheral arterial disease detection, awareness, and treatment in primary careJAMA2001286111317132411560536
- McDermottMMGFriedLSimonsickELingSGuralnikJAsymptomatic peripheral arterial disease is independently associated with impaired lower extremity functioning: The women’s health and aging studyCirculation200010191007101210704168
- HiattWRMedical treatment of peripheral arterial disease and claudicationN Engl J Med2001344211608162111372014
- CriquiMHFronekAKlauberMRBarrett-ConnorEGabrielSThe sensitivity, specificity, and predictive value of traditional clinical evaluation of peripheral arterial disease: Results from noninvasive testing in a defined populationCirculation19857135165223156007
- McDermottMMMehtaSGreenlandPExertional leg symptoms other than intermittent claudication are common in peripheral arterial diseaseArch Intern Med1999159438739210030313
- MohlerERTreat-JacobsonDReillyMPUtility and barriers to performance of the ankle-brachial index in primary care practiceVasc Med20049425326015678616
- Cortez-CooperSupakTanaka. A new device for automatic measurements of arterial stiffness and ankle-brachial indexAm J Cardiol2003911215191522A151912804752
- RichartTKuznetsovaTWiznerBStruijker-BoudierHAStaessenJAValidation of automated oscillometric versus manual measurement of the ankle-brachial indexHypertens Res2009321088488819730440
- BeckmanJAHigginsCOGerhard-HermanMAutomated oscillometric determination of the ankle-brachial index provides accuracy necessary for office practiceHypertension2006471353816344373
- HirschATHaskalZTHertzerNRACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): A collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients with Peripheral Arterial Disease): Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; Transatlantic Inter-society Consensus; and Vascular Disease FoundationCirculation200611311e463e65416549646
- NewmanABSiscovickDSManolioTAAnkle-arm index as a marker of atherosclerosis in the cardiovascular health study. Cardiovascular heart study (CHS) collaborative research groupCirculation19938838378458353913
- BlandJMAltmanDGStatistical methods for assessing agreement between two methods of clinical measurementLancet1986184763073102868172
- KolliasAXilomenosAProtogerouADimakakosEStergiouGSAutomated determination of the ankle-brachial index using an oscillometric blood pressure monitor: Validation vs Doppler measurement and cardiovascular risk factor profileHypertens Res201134782583021593742
- HamelJFFoucaudDFanelloSComparison of the automated oscillometric method with the gold standard Doppler ultrasound method to access the ankle-brachial pressure indexAngiology201061548749120211935
- NicolaiSPKruidenierLMRouwetEVAnkle brachial index measurement in primary care: Are we doing it right?Br J Gen Pract20095956342242719520025
- KornoMEldrupNSillesenHComparison of ankle-brachial index measured by an automated oscillometric apparatus with that by standard Doppler technique in vascular patientsEur J Vasc Endovasc Surg200938561061519751982
- MacDougallAMTandonVWilsonMPWilsonTWOscillometric measurement of ankle-brachial indexCan J Cardiol2008241495118209769