Abstract
Massive rectal bleeding is an uncommon presentation of ileal tuberculosis. Fewer than 12 cases are reported in the literature. We report a case of ileal tuberculosis presenting at the emergency department with subacute intestinal obstruction and severe rectal bleeding. The case of the massive bleeding could be identified only after an exploratory laparotomy.
Introduction
The clinical manifestations of intestinal tuberculosis are nonspecific. Most patients present with low grade fever, weight loss, abdominal pain, anorexia, or diarrhea.Citation1 Ileal tuberculosis is one of the commonly encountered surgical emergencies; the incidence of intestinal tuberculosis in presence of active pulmonary tuberculosis is between 3%–90%.Citation2,Citation3 Varied acute presentations of ileal tuberculosis are encountered such as subacute intestinal obstruction due to stricture or adhesions, or tuberculous stricture perforation. Massive rectal bleeding is considered a rarely presented symptom of intestinal tuberculosis.Citation4–Citation9 The ileocaecal region is the most common site of gastrointestinal involvement and hemorrhage due to tuberculosis is often occurred in this region.Citation6 Here we report an Indian male diagnosed with ileal tuberculosis presenting with massive bleeding from the rectum.
Case report
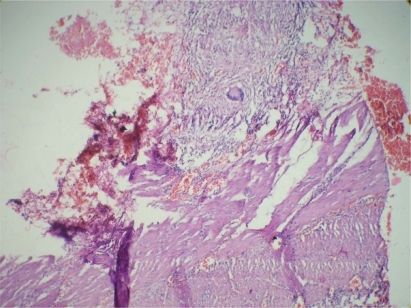
A 30-year-old male patient presented to us with a complaint of being unable to evacuate his bowels and flatulence for the previous two days and with persistant bleeding from the rectum for one day. No other positive history was elicited. On examination, patient was pale. He had a pulse rate of 120 beats/minute and blood pressure was 90/60 mm Hg. Rectal examination showed the presence of fresh blood. Ryle’s tube showed the presence of clear bile. Patient was stabilized haemodynamically. Upper gastrointestinal endoscopy performed was normal. Emergency investigations showed Hb of 4 g% and hematocrit 29%. The white blood cell count was 1,800/μl and platelet count was 95,000/μl. Chest X-ray was found to be normal. Patient’s rectal bleeding continued, hence a colonoscopy was performed, which could not be completed since the whole colon was filled with blood and blood clots. Hence a decision to explore the patient in view of persistent rectal bleeding was undertaken after adequate blood transfusion. At laparotomy terminal ileum was full of blood and a nonpassable stricture was seen in the terminal ileum one and a half feet from the ileocaecal junction and mesenteric lymph nodes were also enlarged. The rest of the bowel was unremarkable. A resection anastomosis of the stricture was performed. After opening the lumen of ileum which was resected, longitudinally we found polypoidal mass of size 3.5 × 2.5 × 2 cm intraluminally adjoining the stricture having hemorrhagic surface area. Rest of mucosa shows multiple superficial ulcers of size 0.5 cm (). Histopathology showed the presence of epitheloid granulomas and Langhans-type giant cells and evidence of endarteritis, suggestive of tuberculous etiology () Patient was started on four anti-tubercular drugs, and had an uneventful post-operative recovery.
Discussion
Intestinal tuberculosis is much more difficult to diagnose than pulmonary tuberculosis and requires a high index of suspicion. Intestinal tuberculosis presenting with lower gastrointestinal bleed is rare and accounts for about 5% of cases of lower gastrointestinal bleeding.Citation2,Citation3 In the presence of active pulmonary tuberculosis, vague abdominal pain, weight loss, and passage of a small amount of blood from the rectum could suggest the possibility of intestinal tuberculosis.Citation2,Citation6
Colonoscopy followed by biopsy is considered the most effective investigation for definitive diagnosis of ileocaecal and colonic tuberculosis.Citation10 However, the endoscopic and histological examination of the involved areas often shows nonspecific findings and cultures for tuberculosis are often negative.Citation11
The patient had no evidence of active pulmonary tuberculosis and had massive rectal bleeding so exploratory laprotomy was performed and ileal tuberculosis was diagnosed on the basis of histopathological examinations. Pathologic findings of a short diseased segment of ileum is common, although it is unusual to have proximal ileum involvement without the involvement of terminal ileum; the patient had a solitary stricture in the terminal ileum. The granulomas in the bowel may be noncaseating with circumferential ulcers, which can lead to bowel obstruction.Citation2–Citation4 Massive gastrointestinal bleed occurs because of underlying obliterative endarteritis within the ulcer cater.Citation2 The patient had both stricture formation and evidence of obliterative endarteritis. Technetium 99m-labeled red blood cell scan can help localize the bleeding lesion.Citation3
In a literature review, we found only 10 cases of intestinal tuberculosis presenting with bleeding per rectum.Citation2–Citation5,Citation7–Citation9,Citation12–Citation14 Of these patients, seven had bleeding from the ileocaecal area,Citation2,Citation4–Citation6,Citation13–Citation15 two from the descending colon,Citation16,Citation17 and one from the transverse colon.Citation18 Thus, in most of these patients, the bleeding occurred from the ileocecal area and massive bleeding from ileum or jejunum (except for terminal ileum) was not reported.
In a study of 130 patients with alimentary tract tuberculosis by Al Karawi and colleagues,Citation1 the disease was located in the small bowel in 44 patients (33.8%) and in the large bowel in 29 patients (22.3%). Moreover, in their study of 44 patients with small bowel tuberculosis, hemorrhage was observed in only one patient but was observed in three of 29 patients with large bowel tuberculosis.Citation1 According to their report, it is suggested that bleeding from small bowel tuberculosis is rare although small bowel tuberculosis is not so uncommon.
Barium enema was performed in seven of 10 patients who reported with intestinal tuberculosis with massive rectal bleeding. Colonic lesions were revealed in five patients. The nature of the lesions remained unrecognized preoperatively. Carcinoma or Crohn’s disease were the most common preoperative diagnoses.
Colonoscopy was performed in four of 10 patients and showed lesions in two patients. Except for one patient,Citation16 histological small intestinal tuberculosis was not found. 99mTc red blood cell scintigraphy was useful to locate the bleeding lesion and to make a preoperative diagnosis of hemorrhage from the ileum. 99Tc red blood cell scintigraphy is more sensitive than angiography for detecting bleeding sites and can detect sites with a minimum bleeding rate as low as 0.1 ml/min.Citation19
Our literature review found that the preferred treatment of intestinal tuberculosis was medical. Except for one patient with bleeding from the descending colon,Citation16 patients with massive bleeding from intestinal tuberculosis were treated by laprotomy and antitubercular drugs postoperatively. Histological examination of resected specimen showed caseating granulomas in all patients. This finding indicates that surgery remains the definitive therapeutic for the diagnosis and treatment of patients of massive rectal bleeding due to intestinal tuberculosis. Indeed, in our patient, no rectal bleeding was seen after surgery and diagnosis was made on basis of histopathological examination of the resected specimen.
Since the symptoms associated with intestinal tuberculosis are highly variable, hemorrhage, obstruction, perforation, or fistula may occur at various levels of the small and large bowel. From our experience and review of literature, although massive rectal bleeding from intestinal tuberculosis is rare, it is suggested that small intestinal tuberculosis should be kept in mind as a cause of rectal bleeding, especially if the patient is an immunocompromised host.
Conclusion
Massive rectal bleeding is an uncommon presentation of ileal tuberculosis. In the presence of active pulmonary tuberculosis, intestinal tuberculosis can be considered as a differential diagnosis of massive rectal bleeding, especially in endemic areas of tuberculosis.
Disclosures
The authors report no conflicts of interest in this work.
References
- Al KarawiMAMohamedAEYasawyMIProtean manifestation of gastrointestinal tuberculosis: report on 130 patientsJ Clin Gastroenterol19952032252327797832
- ShermanHIJohnsonRBrockTMassive gastrointestinal bleeding from tuberculosis of small intestineAm J Gastroenterol1978703314316309722
- WatanabeTKudoMKayabaMMassive rectal bleeding due to ileal tuberculosisJ Gastroenterol199934452552910452689
- VermaPKapurBMMassive rectal bleeding due to intestinal tuberculosisAm J Gastroenterol1979712217219312011
- GoudarziHAMasonLBFatal rectal bleeding due to tuberculosis of the cecumJAMA198224756676686976444
- AnscombeARKeddieNCSchofieldPFCaecal tuberculosisGut1967843373436039721
- RabkinDGCaiatiJMAllendorfJATreatMIntractable hematochezia: an unusual presentation of intestinal tuberculosisSurgery2003133559259312773991
- ParkJKLeeSHKimSGA case of intestinal tuberculosis presenting massive hematochezia controlled by endoscopic coagulation therapyKorean J Gastroenterol2005451606315665569
- NdububaDAOlasodeBJOlatundeLOAbdominal tuberculosis with fatal gastro-intestinal haemorrhageCent Afr J Med19974361751779431746
- MarshallJBTuberculosis of the gastrointestinal tract and peritoneumAm J Gastroenterol19938879899998317433
- MorgantePEGandaraMASterleEThe endoscopic diagnosis of colonic tuberculosisGastrointest Endosc19893521151182714594
- JoshiMABalsarkarDAbhyankarAMassive rectal bleeding due to jejunal and colonic tuberculosisTrop Gastroenterol199819416817010228447
- PozniakALDalton-ClarkHJRalphsDNColonic tuberculosis presenting with massive rectal bleedingTubercle19856642952993878613
- HiranSPandeTKKumarSMassive rectal bleeding due to ileocaecal tuberculosis (conservative approach)Postgrad Med J19947081955568140028
- BrennerSMAnnesGParkerJGTuberculous colitis simulating non specific granulomatous disease of the colonAm J Dig Dis19701585925410870
- MonkemullerKELewisJBJrMassive rectal bleeding from colonic tuberculosisAm J Gastroenterol1996917143914418678011
- DevanesanJDSableRAPitchumoniCSLevRZapiachLSegmental tuberculosis of the colon mimicking carcinomaArch Surg1980115190917350891
- TishlerJMTuberculosis of the transverse colonAJR Am J Roentgenol19791332229232110085
- SmithRCopelyDJBolenFH99mTc RBC scintigraphy: correlation of gastrointestinal bleeding rates with scintigraphic findingsAJR Am J Roentgenol198714858698743495120