Abstract
Type 2 diabetes mellitus affects 5.9% of the world adult population, with older people and some ethnic groups disproportionately affected. Treatment of older people with diabetes differs in many ways from that in younger adults since the majority have type 2 disease and are at particular risk of macrovascular rather than disabling microvascular disease. Insulin therapy, the most effective of diabetes medications, can reduce any level of elevated HBA1c if used in adequate doses. However, some clinicians are often reluctant to initiate insulin therapy in older people with diabetes mainly out of their concerns about adverse reactions to insulin, particularly hypoglycemia. There is evidence suggesting that insulin aspart appears to act similarly to regular human insulin in older people with type 2 diabetes mellitus. Insulin aspart can be used in the treatment of older people with diabetes, but this should be individualized. There is evidence that it improves postprandial glucose control, improves long-term metabolic control, reduces risk of major nocturnal hypoglycemia and increases patient satisfaction compared with soluble insulin.
Introduction
The global epidemic of type 2 diabetes continues unabated and now affects 5.9% of the world’s adult population. Older people and members of some ethnic groups are disproportionately affected.Citation1
An age-associated hyperglycemia phase and glucose intolerance in older people was first described in 1921Citation2 and has been confirmed on many occasions since.Citation3 The clinical presentation of diabetes in older people is often non specific and atypical and as a result the diagnosis is often missed or delayed. In addition older people with diabetes have higher rates of functional, psychological and cognitive impairments, and disabilities. Moreover, older people often have a wide co-morbidity profile linked to the inevitable consumption of multiple medications, and management guidance up to now has been relatively limited due to the lack of focused clinical guidelines, despite the overwhelming evidence base in diabetes generally.
There are no outcome data on the long term effect of tight glycemic control in older people with diabetes, and it is by a process of extrapolation from data on young and middle age diabetic subjects that the management of type 2 older people remains essentially the same as in younger patients. Modification of lifestyle and dietary advice plus the targeted use of single oral agents such as metformin are the most important early management steps. When these measures fail to control the symptoms and improve glycemic control then other oral antidiabetic medications and insulin analogs can be considered. This paper describes the value of using a specific short-duration insulin analog.
Management of diabetes in older people
The consensus statement from the American Diabetes Association and the European Association for the study of Diabetes published in 2006 on the management of hyperglycemia in type 2 diabetes produced a consensus algorithm for the initiation and adjustment of therapy.Citation4
Treatment of older people with diabetes differs in many ways from that in younger adults since the majority have type 2 disease and are at particular risk of macrovascular rather than disabling microvascular disease. Treatment approaches therefore need to take particular account of cardiovascular risk factorsCitation5 particularly in those at home or in care homes.Citation6–Citation7 The decision to offer treatment should be based on the likely benefit/risk ratio for the intervention in the individual concerned, but factors such as vulnerability to hypoglycemia, ability to self-manage, the presence or absence of other pathologies, the cognitive status, and life expectancy must be considered.
Concern about hypoglycemia and lack of evidence of benefit has contributed to underutilization of insulin in older people with type 2 diabetes in the past. Following the landmark UKPDS (United Kingdom Prospective Diabetes Study) it is clear that many elderly patients treated with diet and oral antidiabetic agents will develop beta-cell failure and will be at risk of worsening glycemic control with reduced well-being unless insulin is considered. The UKPDSCitation8 and Kumamoto University studiesCitation9 utilized a target HbA1c level of 7.0% that may be unrealistic in the context of hypoglycemic risk for many older people. The Steno-2 study,Citation10 which includes treatment of macrovascular risk factors as well as glycemic control, represents a multifactoral approach to managing diabetes that is appropriate for all older people in the context of a healthy aging program combining lifestyle and therapeutic interventions. Recommendations from the European Diabetes Working Party For Older People 2000–2004 (available at www.eugms.org) suggest aiming for a target HbA1c of 6.5% to 7.5% for subjects with single system involvement, with the precise target depending on existing cardiovascular disease, presence of microvascular complications, and ability to self-manage.Citation11
Principles of insulin therapy in older people
Insulin therapy, the most effective of diabetes medications, can reduce any level of elevated HbA1c if used in adequate doses. However, some clinicians are often reluctant to initiate insulin therapy in older people with diabetes mainly out of their concerns about adverse reactions to insulin, particularly hypoglycemia (). Hypoglycemic risk can be minimized by initial careful assessment of the patient’s cognitive function, by patient education, and careful selection of treatment options and glycemic targets.
Table 1 Concerns about the use of insulin in older people
Insulin aspart
The human insulin analog, insulin aspart, with its proline having been replaced by the negatively charged aspartic acid at position 28 of the B-chain, has an insulin-receptor affinity similar to that of human insulin.Citation12
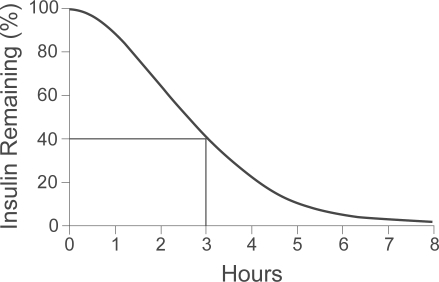
It has a shorter onset and duration of action and can be given immediately before meals.Citation13 Its unique molecular structure that its absorption is fast, its action is rapid and that its duration of action is short (). Other researchers suggested that subcutaneous injections of insulin aspart just before meals better mimic the endogenous insulin profile in blood compared with human insulin, resulting in improved glucose control in a meal-related insulin regimen.Citation14–Citation16
Figure 1 The timing of action for insulin aspart. A euglycemic clamp is used for delivery of the insulin aspart (0.2 units/kg of body weight, delivered into the abdomen). The use of this graph helps patients avoid “insulin stacking”. For example, 3 hours after the administration of 10 units of insulin aspart, one can estimate that there is still 40% times 10 units, or 4 units, of insulin remaining. Reproduced with permission from Hirsch IB, Insulin analogues. New Engl J Med. 2005;352:174–183.Citation14 Copyright © 2005 Massachusetts Medical Society. All rights reserved.
Home et alCitation17 in a 6-month, prospective, randomized, open-label, parallel study, the effect of insulin aspart on long term glycemic control was compared with soluble human insulin in 1070 patients with type 1 diabetes. The study found that after 8 months treatment, HbA1c was significantly lower (by 0.12%) with insulin aspart than soluble human insulin.
Treatment satisfaction assessed by the WHO DTSQ (Diabetes Treatment and Satisfaction Questionnaire) was significantly improved with insulin aspart.Citation16 The relative risk of a major hypoglycemic episode with insulin aspart compared with soluble human insulin was 0.83 (0.59–1.18, NS). Major night-time hypoglycemic events requiring parenteral treatment were less with insulin aspart (1.3 vs 3.4% of patients, p < 0.05). Other studies have also found that insulin aspart is superior to soluble human insulin in controlling post-prandial blood sugar.Citation18
A recent evidence-based medicine review of biphasic insulin aspart (BIAsp) 30 in type 2 diabetes mellitus has concluded that the reported efficacy and tolerability of BIAsp 30 in the treatment of diabetes based on a variety of clinical endpoints is supported by a good body of evidence relating to its use in different dosage regimens and in comparison with other insulin treatment regimens.Citation19 Chlup et al studied 57 individuals with type 2 diabetes, comparing the use of human regular insulin and insulin aspart, and found that insulin aspart appears to be more effective than human regular insulin.Citation20 Moreover, another short-acting insulin (insulin glulisine) was found to provide a small improvement in glycemic control compared with regular human insulin in patients with type 2 diabetes who are already relatively very well controlled in insulin alone or insulin plus oral hypoglycemic agents.Citation21
Use of insulin aspart in older people
Studies comparing insulin aspart and regular insulin in elderly patients with type 2 diabetes have been conducted by Meneilly.Citation22 The aim of the studies was to evaluate the pharmacokinetic and pharmacodynamic properties of insulin aspart in older people with diabetes. They studied 19 patients (10 males and 9 females), age 72 ± 1 years, BMI 27 ± 1 kg/m2 and HbA1c 6.4 ± 0.1%, diabetes duration <5 years; 9 patients were treated with metformin and 10 patients with diet. In a random order the subjects underwent 2 studies.
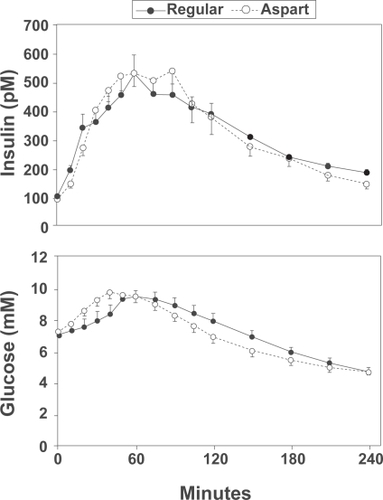
In one study, 0.1 units/kg of regular insulin were administered at 7:30 AM. Thirty minutes later at time 0 subjects were given 235 mL of Ensure Plus Fibre® (Abbott). The other study was identical to the first study except that insulin aspart 0.1 units/kg was given at time zero. Insulin and glucose values were measured at regular intervals. The results indicate that insulin aspart appears to act similarly to regular human insulin in older people with type 2 diabetes ().
Figure 2 Insulin and glucose values during the test meal in response to regular insulin and insulin aspart in 19 patients (10 males and 9 females), age 72 ± 1 years, BMI 27 ± 1 kg/m2 and HbA1c 6.4 ± 0.1% and diabetes duration <5 years. Reproduced with permission from Meneilly GS. A comparison of insulin aspart and regular insulin in elderly patients with type 2 diabetes. Diabetes Obes Metab. 2007;9(5):754–755.Citation22 Copyright © 2007 Blackwell Publishing.
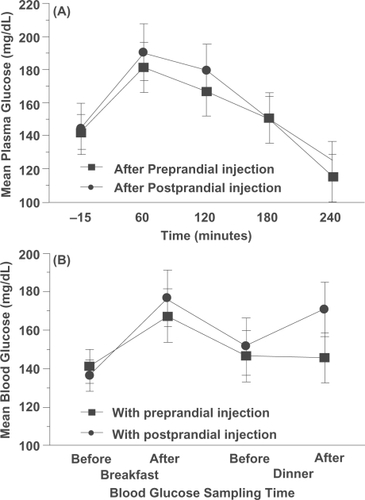
Warren et al,Citation23 in a multi-center open-label randomized cross-over two-arm study of 10 weeks’ treatment, also looked at post-prandial versus pre-prandial dosing of BIAsp 30 in elderly type 2 diabetes patients. Their conclusion was that post-prandial injection of BIAsp 30 may be an acceptable alternative to minimize the risk of hypoglycemia for some older people with type 2 diabetes ().
Figure 3 Glycemic profiles at the end of each treatment period. Ninety-three elderly patients (≥65 years) were treated with bid pre-prandial injections of BIAsp 30 during a 2-week run-in period and subsequently randomized to a 4-week treatment with either pre- or post-prandial bid BIAsp 30, followed by crossover to the other regimen for 4 weeks. Reproduced with permission from Warren ML, Conway MJ, Klaff LJ, Rosenstock J, Allen E. Postprandial versus preprandial dosing of biphasic insulin aspart in elderly type 2 diabetes patients. Diabetes Res Clin Pract. 2004;66(1):23–29.Citation23 Copyright © 2004 Elsevier.
In a sub-group analysis,Citation24 the efficacy, safety and treatment satisfaction of insulin aspart was evaluated in elderly patients with type 2 diabetes in the PRESENT Korea NovoMix study. In this 6-month, prospective study, patients inadequately controlled on previous therapies achieved better glycemia (reduction of HbA1c of 1.2 ± 1.6%; reductions of fasting plasma glucose and post-prandial glucose of 2.3 ± 3.5 mmol/L and 4.8 ± 5.3 mmol/L at 6 months, respectively, p < 0.0001 for all). Hypoglycemia rates were lower and weight gain was minimal. Treatment satisfaction was greater than 80%.
Miyashita et al conducted a prospective, randomized study for optimal insulin therapy in type 2 diabetic patients with secondary failure and found that both basal-bolus therapy with the ultra rapid-acting insulin analog and conventional therapy with the twice daily BIAsp produce comparable reduction in HbA1c in type 2 diabetic patients with secondary failure.Citation25 With particular reference to elderly and given that their appetite may be unstable, it may be preferable to treat them with a fast-acting insulin eg, insulin aspart, the dose of which is dependable on the actual amount of food consumed.
With this increasing evidence base, the European Commission announced in September, 2007, their approval of rapidly acting insulin aspart (NovoRapid®; Novo Norkisk) in the treatment of diabetes in elderly patients.
Conclusion
Insulin aspart can be used in the treatment of older people with diabetes; however this treatment should be individualized. There is evidence that it improves post-prandial glucose control, improves long-term metabolic control, reduces risk of major nocturnal hypoglycemia and increases patient satisfaction compared with soluble insulin.
Disclosures
The authors have no conflicts of interest to declare.
References
- SinclairAJCroxsonSCMDiabetes mellitusTallisRCFillitHMBrocklehurst’s textbook of geriatric medicine and gerontology6th edLondonChurchill Livingstone200311931218
- SpenceJCSome observations on sugar tolerance with special reference to variations found at different agesQJ Med192114314326
- DavidsonMBThe effect of aging on carbohydrate metabolism: a review of the English literature and a practical approach to the diagnosis of diabetes mellitus in the elderlyMetabolism1979286688705377005
- NathanDMBuseJBDavidsonMBManagement of hyperglycaemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapyDiabetolgia20064911711721
- HendraTJSinclairAJImproving the care of elderly diabetic patients: the final report of the St Vincent Joint Task Force for diabetesAge Ageing199726369143430
- SinclairAJTurnbullCJCroxsonSCMDocument of care for older people with diabetesPostgrad Med J1996723343388758009
- SinclairAJTurnbullCJCroxsonSCMDocument of diabetes care for residential and nursing homesPostgrad Med J1997736116129497967
- UK Prospective Diabetes Study (UKPDS) GroupIntensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33)Lancet19983528378539742976
- OhkuboYKishikawaHArakiEIntensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year studyDiabetes Res Clin Pract1995281031177587918
- GaedePVedelPLarsenNMultifactorial intervention and cardiovascular disease in patients with type 2 diabetesN Engl J Med200334838339312556541
- European Diabetes Working Party For Older People 2000–2003. Clinical Guidelines for Type 2 Diabetes Mellitus. Available from: www.eugms.org
- SimpsonKLSpencerCMInsulin aspartDrugs19995775976510353301
- LindholmAJacobsenLVClinical pharmacokinetics and pharmacodynamics of insulin aspartClin Pharmacokinet20014064165911605714
- HirschIBInsulin analoguesNew Engl J Med200535217418315647580
- MudaliarSLindbergFAJoyceMInsulin aspart (B28 Asp-insulin): a fast-acting analog of human insulin: absorption kinetics and action profile compared with regular human insulin in healthy nondiabetic subjectsDiabetes Care1999221501150610480516
- ØsterbergOErichsenLIngwersenSHPlumAPoulsenHEViciniPPharmacokinetic and pharmacodynamic properties of insulin aspart and human insulinJ Pharmacokinet Pharmacodyn20033022123514571692
- HomePDLindholmARiisAInsulin aspart vs human insulin in the management of long-term blood glucose control in type 1 diabetes mellitus: a randomized controlled trialDiabet Med20001776277011131100
- RaskinPGuthrieRALeiterLRiisAJovanovicLUse of insulin aspart, a fast-acting insulin analog, as the mealtime insulin in the management of patients with type 1 diabetesDiabetes Care200023558358810834413
- GoughSCLTibaldiJBiphasic insulin aspart in type 2 diabetes mellitus: an evidence-based medicine reviewClin Drug Invest2007275299324
- ChlupRZapletalovaJSeckarPBenefits of complementary therapy with insulin aspart versus human regular insulin in persons with type 2 diabetes mellitusDiabetes Technol Ther20079322323117561792
- DaileyGMosesRRosenstockJInsulin glulisine provides improved glycemic control in patients with type 2 diabetesDiabetes Care2004272363236815451901
- MeneillyGSA comparison of insulin aspart and regular insulin in elderly patients with type 2 diabetesDiabetes Obes Metab20079575475517697065
- WarrenMLConwayMJKlaffLJRosenstockJAllenEPostprandial versus preprandial dosing of biphasic insulin aspart in elderly type 2 diabetes patientsDiabetes Res Clin Pract2004661232915364158
- JangHCLeeSRVazJABiphasic insulin aspart 30 in the treatment of eldserly patients with type 2 diabetes: a subgroup analysis of the PRESENT Korea NovoMix studyDiabetes Obes Metab2009111202618479469
- MiyashitaYNishimuraRNemotoMMatsudairaTProspective randomized study for optimal insulin therapy in type 2 diabetic patients with secondary failureCardiovasc Diabetol2008716doi:1186/1475-2840-7-16.18507868