Abstract
Constipation disproportionately affects older adults, with a prevalences of 50% in community-dwelling elderly and 74% in nursing-home residents. Loss of mobility, medications, underlying diseases, impaired anorectal sensation, and ignoring calls to defecate are as important as dyssynergic defecation or irritable bowel syndrome in causing constipation. Detailed medical history on medications and co-morbid problems, and meticulous digital rectal examination may help identify causes of constipation. Likewise, blood tests and colonoscopy may identify organic causes such as colon cancer. Physiological tests such as colonic transit study with radio-opaque markers or wireless motility capsule, anorectal manometry, and balloon expulsion tests can identify disorders of colonic and anorectal function. However, in the elderly, there is usually more than one mechanism, requiring an individualized but multifactorial treatment approach. The management of constipation continues to evolve. Although osmotic laxatives such as polyethylene glycol remain mainstay, several new agents that target different mechanisms appear promising such as chloride-channel activator (lubiprostone), guanylate cyclase agonist (linaclotide), 5HT4 agonist (prucalopride), and peripherally acting μ-opioid receptor antagonists (alvimopan and methylnaltrexone) for opioid-induced constipation. Biofeedback therapy is efficacious for treating dyssynergic defecation and fecal impaction with soiling. However, data on efficacy and safety of drugs in elderly are limited and urgently needed.
Keywords:
Introduction
The management of constipation in the elderly is challenging both for patients and healthcare providers. Multiple reasons contribute to this phenomenon, such as the effects of aging on gut physiology, co-morbid illnesses, medications, loss of mobility, inadequate caloric intake, and anorectal sensory changes. Elderly patients, especially those with advanced dementia in nursing homes and those on opioids for palliative care, require an individualized approach for the treatment of constipation.
Definition and epidemiology
Constipation is not a well defined disease entity, but a general term used to describe the difficulties that a subject experiences with moving their bowels.Citation1 Healthcare providers typically define constipation as stool frequency of less than 3 bowel movements per week.Citation2 In contrast, patients define constipation as any form of “difficult defecation”, such as straining, hard stool, feeling of incomplete evacuation, and non-productive urge.Citation3,Citation4 Compared to younger patients, the elderly report more frequent straining, self-digitation, and feelings of anal blockage.Citation4,Citation5 In a study of 531 patients in general practice, 50% gave a different definition of constipation compared to their physicians. Citation6 Because of these variable definitions of constipation, an international panel of experts proposed the Rome criteria for constipation. The Rome III criteria used a combination of subjective symptoms to define constipation,Citation7 and are currently used widely for performing clinical research in this field.
It is reported that the prevalence of constipation increases with age, especially those over the age of 65 years.Citation8 In elderly patients living in the community, the prevalence of constipation is 50%.Citation4 This number is even higher in nursing home residents, with 74% using daily laxatives.Citation4,Citation9–Citation11 Likewise, elderly women are 2 to 3 times more likely to report constipation than their male counterparts.Citation4 Constipation is also more commonly seen in patients taking multiple medications.Citation12
Health-related quality of life and constipation
Evidence in both disease-specific and generic quality of life (QOL) instruments has shown that constipation is associated with impaired health-related quality of life (HR-QOL). For example, in one study of 126 community-dwelling older adults, respondents with chronic constipation had lower Short-Form 36 (SF-36) scores for physical functioning, mental health, general health perception, and bodily pain when compared to respondents with no constipation.Citation13 Likewise, using the Psychological General Well-Being (PGWB) index, 84 subjects with constipation has lower PGWB total scores and lower domain scores for anxiety, depression, well-being, self-control and general health subscales, indicating worse HR-QOL.Citation14 Furthermore, improvements with HR-QOL were noted with treatment of constipation.Citation15 After laxatives caused significant increases in weekly bowel movements, patients reported fewer urinary symptoms, better sexual function and improved mood and depression.
In addition, constipation is a significant driver of health care costs, as it is ranked among the top 5 most common physician diagnosis for gastrointestinal outpatient visits.Citation4 Using a community survey, the management of constipation is estimated to average $200 per patient within a large HMO.Citation16 Over $821 million dollars (2000 value) was spent on over-the-counter laxatives in the United States alone.Citation8 Other indirect costs of constipation to society include decrease in work related productivity, absences in school, lower quality of life and higher psychological distress.Citation8
Normal continence and defecation
The pelvic floor consists of superficial and deep muscle layers that envelope the rectum, bladder and uterus.Citation17 The superficial muscle layers consist of the internal and external anal sphincters, the perineal body and the transverse perinei muscles. In contrast, the deep pelvic muscles (also known as levator ani) are composed of the pubococcygeus, ileococcygeus and puborectalis muscles.Citation17 These structures are largely innervated by the sacral nerve roots (S2–S4) and the pudendal nerve.
Continence is the ability to retain feces until it is socially conducive to defecate, while defecation is the evacuation of fecal material from the colon. Both functions are regulated by voluntary and involuntary reflex mechanisms, anatomic factors, rectal sensation, and rectal compliance.
Defecation starts when the cerebral cortex receives an awareness and perception of critical level of filling in the rectum. When the individual adopts a sitting or squatting position, the anal sphincters and the puborectalis relax, straightening the anorectal angle. Simultaneously, the voluntary efforts of bearing down increases the intra-abdominal pressure, facilitating the development of a stripping wave, resulting in stool evacuation.
Common causes of constipation in the elderly
In the elderly, constipation most likely has a multifactorial etiology, with more than one mechanism present in a single patient, such as co-morbid illnesses or medication side effects (). In the elderly, living in hospice with advanced cancer and pain, opioid-induced constipation is common.
Table 1 Common causes of constipation in the elderly
Furthermore, there are psychosocial and behavioral factors that may predispose the elderly to develop constipation, such as decreased mobility, inadequate caloric intake, and anorectal sensation changes. Ignoring calls to defecate, can lead to fecal retention in the elderly.Citation4 Suppression of rectal sensation follows chronic fecal retention. As a result, only large stools will be perceived, leading to difficulty with defecation.Citation4
In the elderly, chronic constipation can lead to fecal impaction and fecal incontinence. Fecal impaction is the accumulation of hardened feces in the colon or rectum.Citation18 Liquid stools from the proximal colon can bypass the impacted stool, causing overflow incontinence, often mistaken for diarrhea. Fecal impaction has been identified in 40% of hospitalized older patients in the UK.Citation18 It has been linked to acute states of confusion in this population. In severe cases, fecal impaction can cause stercoral ulcerations, intestinal obstruction or bowel perforation.Citation18 If left untreated, these complications can be life threatening.
Disorders of colonic and anorectal function causing constipation in the elderly
In the absence of alarm symptoms, such as weight loss, bleeding, change in bowel habit, the two most commonly seen subtypes of primary constipation in the elderly are slow transit constipation (STC) and dyssynergic defecation (DD), with a less common subtype being irritable bowel syndrome with constipation (IBS-C).
Slow transit constipation
STC is defined as the delay of stool transit through the colon, due to a myopathy, neuropathy or secondary to an evacuation disorder such as DD.Citation8
In the elderly, age related neurodegenerative changes in the enteric nervous system have been previously noted. There was a 37% loss of enteric neurons in older people (more than 65 years old) when compared with younger people (20–35 years old).Citation4 This was associated with an increase in the elastic and collagen fibers in the myenteric ganglia of older subjects.Citation4
Similarly, a recent study showed the selective age related loss of neurons expressing choline acetyltransferase with sparing of neuronal nitric oxide in human colon.Citation20 These findings suggest an increase in inhibitory neurons in the aging colon, affecting gut motility. However, the significance of these studies is unclear since these findings could suggest either a primary entity or secondary to chronic use of laxatives and/or behavioral changes of constipated patients through the years.
In fact, gut transit time and colonic motility are similar between healthy older and younger participants.Citation1 In contrast, elderly people with chronic illness reporting constipation have a prolonged total gut transit time of 4 to 9 days (normal is less than 3 days).Citation1 In the least mobile of nursing home residents, transit times are prolonged up to 3 weeks.Citation1 It appears that factors related to aging, such as chronic medical conditions and immobility, impact gut motility, rather than aging itself.
Dyssynergic defecation
DD is characterized by difficulty of expelling stool from the anorectum.Citation8
DD is believed to be caused by failure of recto-anal coordination, either by impaired rectal contraction, paradoxical anal contraction, or inadequate anal relaxation.Citation17 Anorectal physiologic changes, such as reductions in internal anal sphincter pressure, pelvic muscle strength, and changes in rectal sensitivity have been reported in the elderly.Citation4
Women, especially those who had sustained injuries during vaginal deliveries, have larger decrease in anorectal squeeze pressures.Citation4 Taken together, these may predispose the elderly to develop DD.
Irritable bowel syndrome with constipation
IBS-C is largely defined by chronic or recurrent abdominal pain or discomfort associated with altered bowel habits, with ≥25% of stools being hard or lumpy.Citation19 These patients may or may not have STC or DD. Although rare, some elderly subjects have IBS-C.
Diagnosis of constipation in the elderly
Medical history and physical examination
Constipated patients present with several symptoms. As a healthcare provider, it is important to ascertain the patient’s complaint regarding what they mean by constipation. A careful medical history, noting medical conditions and medications that affect colonic transit should be conducted ().
The history should include an assessment of stool frequency, stool consistency, stool size, degree of straining during defecation, and a history of ignoring a call to defecate. A dietary history should assess the amount of fiber and water intake, and the number of meals and when they are consumed. The history should also include the number, type and frequency of laxatives used. In the elderly, fecal seepage and incontinence may be presenting symptoms of fecal impaction.
Finally, a social history with emphasis on the patient’s current living situation, such as living with family or alone; nursing home; or in hospice are important. Furthermore, information about a patient’s activities of daily living, such as dressing and eating, and instrumental activities of daily living, such as grocery shopping and housework, can provide clues on the patient’s functional capacity and level of cognition. Taking note of the patients’ psychiatric co-morbidities and psychosocial stressors are especially important in dealing with IBS patients.
A thorough anorectal and digital rectal exam is essential. It should go beyond looking at skin erosions, skin tags, anal fissures, or hemorrhoids. Using a cotton bud or a blunt needle, gently stroke the four quadrants of the perineal skin. Neuropathy is suspected if this maneuver failed to invoke a reflex contraction of the external anal sphincter. Finally, patients should be asked to bear down as if to defecate. It is important for the examiner to perceive relaxation of the external anal sphincter together with perineal descent. If these features are absent, one should suspect DD.
Metabolic and structural evaluation
Since constipation may be caused by an underlying metabolic and pathologic disorder, routine blood tests, such as a complete blood count, biochemical profile, calcium levels and thyroid functions are usually performed. Structural tests including a flexible sigmoidoscopy or a colonoscopy can provide evidence for chronic laxative use, such as melanosis coli, or mucosal lesions such as solitary rectal ulcer, inflammatory bowel disease, or malignancy. In the absence of a clear explanation, a functional disorder should be considered.
Physiological tests
In order to diagnose STC and DD, several additional Physiological tests are usually employed.
Colonic transit study
The colonic transit study provides a physician with a better understanding of the rate of stool movement through the colon. The test involves the ingestion of a single Stizmarks® capsule (Konsyl Pharmaceuticals, Fort Worth, Texas) containing 24 radio-opaque markers on day 1 and by Obtaining a plain radiograph on day 6 (after 120 hours).
Normal transit is when there are less than 5 markers remaining in the colon.Citation21 STC is diagnosed when 6 or more markers are scattered throughout the colon. Recently, a wireless motility capsule has been tested and found to be useful and safe in the elderly. This not only provides colonic and whole gut transit time but also provides regional transit time such as gastric emptying using a standardized protocol and is free of radiation.Citation22
Anorectal manometry
The anorectal manometry (ARM) provides pressure readings in the rectum and anal sphincters, as well as data on rectal sensation, rectoanal reflexes, and rectal compliance. Citation8 In normal defecation, the rectal pressure rises with a synchronized fall in anal sphincter pressures. The inability to coordinate these anorectal processes underlies the main pathophysiological abnormality in patients with DD.Citation23 These patients are thought to have impaired rectal contraction, paradoxical anal contraction, impaired relaxation, or a combination of these mechanisms.Citation23,Citation24 Finally, the ARM provides information on anorectal sensory dysfunction, as exemplified by higher thresholds for first sensation and thresholds for desire to defecate.Citation23
Balloon expulsion test
This test is performed by inserting a silicon filled stool-like device called the fecom or a 4 cm long balloon filled with 50 mL of warm water inside the patient’s rectum. Most normal subjects can expel the stool-like device within 1 minute. Inability to expel the device within one minute is highly suggestive of DD.Citation23
Prevention and management of constipation in the elderly
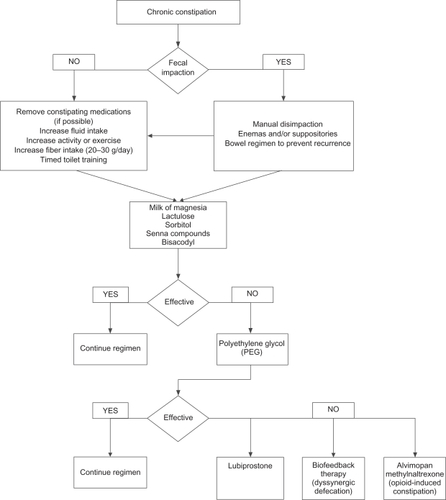
shows a convenient treatment algorithm to assist the practitioner in devising a suitable treatment modality for a given patient. Specific options and treatments are discussed below.
Fluid intake and exercise, caloric intake and timed toilet training
Although useful, there is little evidence to support maintenance of adequate hydration and regular nonstrenuous exercise in the management of constipation. In a study involving 6 test and 9 control subjects, consumption of extra fluid did not show significant differences in stool output.Citation25 Although epidemiologic studies show sedentary people are 3 times more likely to report constipation, studies on the effect of exercise and gut transit time are inconsistent. Citation8 In elderly patients, fluid intake should be monitored closely especially in those with cardiac and renal disease. In contrast, evidence suggests that elderly patients consuming fewer meals and caloric intake are more prone to constipation.Citation26
Patients who have a normal bowel pattern usually move their bowels at the same time every day, suggesting that defecation is partly a conditioned reflex.Citation8 Likewise, colonic motor activity increases after waking and after a meal (gastrocolonic reflex). These suggest that constipated patients may establish a regular pattern of defecation by ritualizing a bowel habit that takes advantage of this normal physiologic stimulus.Citation8 Using the same principle, timed toiled training consists of educating patients to attempt a bowel movement at least twice a day, usually 30 minutes after meals, and to strain no more than 5 minutes.
Diet and fiber
Previous studies have shown that a high fiber diet increases stool weight and decreases colon transit time, while low fiber diet leads to constipation.Citation27,Citation28 However, patients with either STC or DD do not respond well with a dietary fiber of ≥30 g/day.Citation29 In contrast, constipated patients without an underlying motility disorder have improved or became symptom free with this amount of supplemental fiber.Citation29 A systematic review showed that bulk laxatives or fibers showed an average weighted increase of 1.4 (95% CI, 0.6–2.2) bowel movements per week.Citation30 A fiber intake of 20–30 g of fiber a day is generally recommended. A recent randomized controlled trial (RCT) showed that dried plums were more effective than psyllium in the management of mild to moderate constipation.Citation31
Laxatives
Several recent reviews have discussed common classification of laxatives, their mode of action, the recommended dosage, and potential side effects. In the elderly, use of laxatives must be individualized with special attention to patient’s medical history (cardiac and renal co-morbid conditions), drug interactions, costs, and side effects.Citation32 Laxatives most commonly used in clinical practice include milk of magnesia, lactulose, senna compounds, bisacodyl and polyethylene glycol (PEG) preparations.Citation8 In a 4-week study involving constipated elderly patients, 70% sorbitol was as efficacious as lactulose, but was cheaper and better tolerated.Citation33
Similarly, a senna fiber combination (Agiolax®) in elderly nursing home residents improved stool consistency, frequency and ease of passage, when compared with lactulose. Citation34 The senna fiber was also 40% cheaper. In a long term randomized, multi-center study of polyethylene glycol (PEG), 17 grams once a day was better at achieving treatment success at 6 months, when compared with placebo (PEG 52% vs 11% placebo; P < 0.001).Citation35 Treatment success was defined as relief of modified Rome criteria for constipation for 50% or more of their treatment weeks. Furthermore, similar efficacy was seen in the study’s subgroup analysis involving 75 elderly subjects. Lastly, in a short term study of 100 patients with medication induced constipation, PEG at 17 g daily for 28 days was more effective than placebo in achieving treatment success (PEG 78.3% vs placebo 39.1%; P < 0.001).Citation36 Similar results were also observed in the subgroup of 28 elderly patients.
Despite efforts in including the elderly in RCTs, most studies on the use of laxatives in the elderly are limited because of small sample size and problems with methodology. Side effects of laxatives such as abdominal discomfort, electrolyte imbalances, allergic reactions and hepatotoxicity have been previously reported.Citation4
Stool softeners, suppositories and enemas
Although widely practiced, stool softeners have limited clinical efficacy.Citation4,Citation37 Suppositories may be used in institutionalized patients with obstructed defecation to help with rectal evacuation.Citation4
Similarly, enemas are used in this population group to prevent fecal impaction. Side effects such as electrolyte imbalances have been noted with phosphate enemas and rectal mucosal damage with soapsuds enema. When necessary, tap water enema is the safest one to use.
Newer and upcoming treatment options
Lubiprostone
Lubiprostone is an oral bicyclic fatty acid that activates type 2 chloride channels on the intestinal epithelial cells, secreting chloride and water in the gut lumen.Citation38 In several multi-center RCTs, lubiprostone, when compared to placebo, has consistently shown to increase complete spontaneous bowel movements per week, as well as improved stool consistency, straining, constipation severity and patient-reported treatment effectiveness.Citation39–Citation41 In one of the study, 10% of the studies participants were elderly.Citation40
Prucalopride
Prucalopride, a dihydrobenzofurancarboxamide derivative, is a selective high-affinity 5HT4 receptor agonist.Citation42 Unlike other drugs in its class, such as tegaserod, mosapride and renzapride, prucalopride has a lower affinity for the human Ether-a-go-go Related Gene protein (hERG).Citation42 It is believed that the effects on the hERG channel may have led to the unfavorable cardiovascular profile seen with tegaserod. Recently, in a double-blind RCT with 84 elderly nursing home residents with chronic constipation, 2 mg prucalopride once daily for 4 weeks was safe and well tolerated.Citation43 Currently, prucalopride has been released in Europe, but not in the USA.
Linaclotide
Linaclotide is a guanylate cyclase C receptor agonist that stimulates intestinal fluid secretion and transit; it also has been shown to reduce pain in animal models.Citation44 In a multicenter RCT, 310 patients with chronic constipation were randomly assigned to receive 75, 150, 300, or 600 μg oral linaclotide or placebo daily for 4 weeks.Citation44 Compared with placebo, there was a significant dose related increase in weekly rate of spontaneous bowel movements (SBMs) in the linaclotide groups.
Linaclotide also proved effective in improving secondary endpoints, such as stool consistency, straining, abdominal discomfort, bloating, global assessments and quality of life. Diarrhea was the most common adverse event.
Colchicine
Colchicine, an alkaloid substance usually used to treat gout, is an anti-inflammatory agent that inhibits microtubule assembly in white blood cells. However, it is known to induce diarrhea when taken in higher doses. The mechanism of inducing diarrhea by colchicine is unknown. It has been reported that colchicine increases prostaglandin synthesis, intestinal secretion and gastrointestrial motility.Citation45 It also reduces water and electrolyte absorption in the intestine and increases secretion through a cyclic AMP mediated activity.
In a double-blind, placebo-controlled study of patients with STC (n = 60), colchicine was shown to be effective in lowering Knowles-Eccersly-Scot symptoms (KESS) scores.Citation45 KESS is a valid technique in diagnosing and evaluating symptoms of constipation. The mean KESS scores at 2 months were 11.67 and 18.66 for colchicine and placebo groups, respectively (P = 0.0001). The authors concluded that low-dose colchicine (1 mg daily) is effective in the treatment of STC.Citation45
Alvimopan and methylnaltrexone
Recently, alvimopanCitation46–Citation48 and methylnaltrexoneCitation49 have been introduced for the treatment of opioid-induced constipation. Both agents are peripherally acting μ-opioid receptor antagonists that do not cross the blood–brain barrier. As a result, these agents have the advantage of not inhibiting the analgesic effects of opioids.
In a 21-day randomized trial involving 168 patients, alvimopan, in a dose response manner, significantly produced at least 1 bowel movement in 8 hours.Citation48 Furthermore, in a randomized, parallel-group, repeated dose trial involving methylnaltrexone, 5 mg methylnaltrexone produced a 50% laxation response within 4 hours of administration.Citation49 Furthermore, this class of agents has potential uses for other narcotic induced side effects, such as opioid-related nausea and vomiting, urinary retention, pruritus or post-operative ileus.
Dyssynergic defecation and fecal impaction with soiling
The treatment of DD consists of fiber rich diet, laxatives, timed toilet training and biofeedback therapy. The purpose of biofeedback is to restore the normal pattern of defecation by using an instrument based learning process. In biofeedback therapy, patients are taught diaphragmatic breathing techniques to improve their abdominal push efforts and to synchronize this with anal relaxation. A manometric probe is inserted into the patient’s rectum, capturing anal and rectal pressure readings on a monitor. Auditory and visual feedback is provided to the patients as they attempt defecation. The patient’s posture and breathing techniques are also corrected. For sensory rectal training, a balloon in the rectum is distended with 60 mL of air to provide the patient a sensation of rectal fullness or a desire to defecate.
Four RCTs that evaluated the efficacy of biofeedback therapy in the treatment of DD concluded that biofeedback is consistently superior to laxatives, standard therapy, sham therapy, placebo and diazepam.Citation50–Citation53 A preliminary study also showed that home biofeedback is a cost effective alternative when compared to office biofeedback.Citation54
However, the efficacy of biofeedback in the elderly remains unclear. Since biofeedback is based on operant learning conditioning techniques, an evaluation of the patient’s physical and mental capabilities is important in assessing its usefulness in the elderly with significant co-morbidities and advanced dementia.
Surgery
In patients with constipation that is refractory to medical therapy, surgery can be an option. Subtotal colectomy with ileorectal anastomosis is the treatment of choice in patients with refractory slow transit constipation, provided that DD has been excluded.Citation55,Citation56 Results with using segmental colonic resection in constipation are always disappointing.Citation4,Citation57
It is also important to emphasize that in patients with DD, surgery does not improve symptoms unless the dyssynergia has been corrected with biofeedback.Citation8
Reported side effects of surgery include diarrhea, incontinence and bowel obstruction.Citation4
Furthermore, the elderly might be unfit for surgery due to advanced age and significant co-morbidities.
Summary
Constipation is a common polysymptomatic disorder affecting up to 74% of elderly nursing-home residents. It leads to considerable economic burden, loss of work-related productivity, as well as decreased HR-QOL.
Multiple conditions and causes predispose the elderly to constipation and many factors are usually present in one single individual.
The past decade has given us significant mechanistic insights in the pathophysiology of constipation, providing us with newer therapeutic agents and modalities such as lubiprostone, prucalopride, linaclotide, methylnaltrexone and biofeedback therapy. However, data on their efficacy, safety and real-life applicability in the elderly are still limited.
More active recruitment of the elderly in clinical trials is needed to provide better evidence-based management of constipation in this population.
Disclosures
Dr Rao has served as an Advisory Board member, and has received research support from, SmartPill Corporation, Ironwood Pharmaceuticals, and Takeda Pharmaceuticals.
Dr Satish Rao is supported by NIH grant RO1 DK 57100-05.
References
- McCreaGLMiaskowskiCStottsNAPathophysiology of constipation in the older adultWorld J Gastroenterol200814172631263818461648
- DrossmanDASandlerRSMcKeeDCBowel patterns among subjects not seeking health care. Use of a questionnaire to identify a population with bowel dysfunctionGastroenterology19828335295347095360
- ParePFerrazziSThompsonWGAn epidemiological survey of constipation in Canada: Definitions, rates, demographics, and predictors of health care seekingAm J Gastroenterol200196113130313711721760
- BourasEPTangalosEGChronic constipation in the elderlyGastroenterol Clin North Am200938346348019699408
- TalleyNJFlemingKCEvansJMConstipation in an elderly community: A study of prevalence and potential risk factorsAm J Gastroenterol199691119258561137
- HerzMJKahanEZalevskiSConstipation: A different entity for patients and doctorsFam Pract19961321561598732327
- LongstrethGFFunctional bowel disorders: Functional constipationDrossmanDAThe functional gastrointestinal disorders3rd edLawrence (KS)Allen Press Inc.2006515
- RaoSSConstipation: Evaluation and treatment of colonic and anorectal motility disordersGastroenterol Clin North Am2007363687711x17950444
- HarariDGurwitzJHAvornJConstipation: Assessment and management in an institutionalized elderly populationJ Am Geriatr Soc19944299479528064102
- TalleyNJDef initions, epidemiology, and impact of chronic constipationRev Gastroenterol Disord20044Suppl 2S3S1015184814
- PrimroseWRCapewellAESimpsonGKPrescribing patterns observed in registered nursing homes and long-stay geriatric wardsAge Ageing198716125283105271
- WhiteheadWEDrinkwaterDCheskinLJConstipation in the elderly living at home. definition, prevalence, and relationship to lifestyle and health statusJ Am Geriatr Soc19893754234292539405
- O’KeefeEATalleyNJTangalosEGA bowel symptom questionnaire for the elderlyJ Gerontol1992474M116M1211624694
- GliaALindbergGQuality of life in patients with different types of functional constipationScand J Gastroenterol19973211108310899399387
- CharachGGreensteinARabinovichPAlleviating constipation in the elderly improves lower urinary tract symptomsGerontology200;472727611287730
- SinghGLingalaVWangHUse of health care resources and cost of care for adults with constipationClin Gastroenterol Hepatol2007591053105817625982
- RaoSSGoJTTreating pelvic floor disorders of defecation: Management or cure?Curr Gastroenterol Rep200911427828719615303
- GallagherPO’MahonyDConstipation in old ageBest Pract Res Clin Gastroenterol200923687588719942165
- VidelockEJChangLIrritable bowel syndrome: Current approach to symptoms, evaluation, and treatmentGastroenterol Clin North Am200736366568517950443
- BernardCEGibbonsSJGomez-PinillaPJEffect of age on the enteric nervous system of the human colonNeurogastroenterol Motil2009217746E4619220755
- BharuchaAEPhillipsSFSlow transit constipationGastroenterol Clin North Am2001301779511394038
- RaoSSPaulsonJSaadRAssessment of colonic, whole gut and regional transit in elderly constipated and healthy subjects with novel wireless pH/pressure capsule (SmartPill®).Gastroenterology2009136A950
- RaoSSWelcherKDLeistikowJSObstructive defecation: A failure of rectoanal coordinationAm J Gastroenterol1998937104210509672327
- RaoSSHatfieldRSofferEManometric tests of anorectal function in healthy adultsAm J Gastroenterol199994377378310086665
- ChungBDParekhUSellinJHEffect of increased fluid intake on stool output in normal healthy volunteersJ Clin Gastroenterol199928129329916661
- TowersALBurgioKLLocherJLConstipation in the elderly: Influence of dietary, psychological, and physiological factorsJ Am Geriatr Soc19944277017068014342
- TuckerDMSandsteadHHLoganGMJrDietary fiber and personality factors as determinants of stool outputGastroenterology19818158798836269944
- BurkittDPWalkerARPainterNSEffect of dietary fibre on stools and the transit-times, and its role in the causation of diseaseLancet197227792140814124118696
- VoderholzerWASchatkeWMuhldorferBEClinical response to dietary fiber treatment of chronic constipationAm J Gastroenterol199792195988995945
- TramonteSMBrandMBMulrowCDThe treatment of chronic constipation in adults. A systematic reviewJ Gen Intern Med199712115249034942
- RaoSSCPaulsonJDonahoeRInvestigation of dried plums in constipation – a randomized controlled trialAM J Gastroenterol2009104S496
- LockeGR3rdPembertonJHPhillipsSFAmerican gastroenterological association medical position statement: Guidelines on constipationGastroenterology200011961761176611113098
- LederleFABuschDLMattoxKMCost-effective treatment of constipation in the elderly: A randomized double-blind comparison of sorbitol and lactuloseAm J Med19908955976012122724
- PassmoreAPDaviesKWFlanaganPGA comparison of agiolax and lactulose in elderly patients with chronic constipationPharmacology199347Suppl 12492528234437
- DipalmaJAClevelandMVMcGowanJA randomized, multicenter, placebo-controlled trial of polyethylene glycol laxative for chronic treatment of chronic constipationAm J Gastroenterol200710271436144117403074
- DiPalmaJAClevelandMBMcGowanJA comparison of polyethylene glycol laxative and placebo for relief of constipation from constipating medicationsSouth Med J2007100111085109017984738
- RamkumarDRaoSSEfficacy and safety of traditional medical therapies for chronic constipation: Systematic reviewAm J Gastroenterol2005100493697115784043
- CuppolettiJMalinowskaDHTewariKPSPI-0211 activates T84 cell chloride transport and recombinant human ClC-2 chloride currentsAm J Physiol Cell Physiol20042875C1173C118315213059
- JohansonJFMortonDGeenenJMulticenter, 4-week, double-blind, randomized, placebo-controlled trial of lubiprostone, a locally-acting type-2 chloride channel activator, in patients with chronic constipationAm J Gastroenterol2008103117017717916109
- JohansonJFUenoRLubiprostone, a locally acting chloride channel activator, in adult patients with chronic constipation: A double-blind, placebo-controlled, dose-ranging study to evaluate efficacy and safetyAliment Pharmacol Ther200725111351136117509103
- JohansonJFDrossmanDAPanasRClinical trial: Phase 2 study of lubiprostone for irritable bowel syndrome with constipationAliment Pharmacol Ther200827868569618248656
- CamilleriMKerstensRRykxAA placebo-controlled trial of prucalopride for severe chronic constipationN Engl J Med2008358222344235418509121
- CamilleriMBeyensGKerstensRSafety assessment of prucalopride in elderly patients with constipation: A doubleblind, placebo-controlled studyNeurogastroenterol Motil200921121256126319751247
- LemboAJKurtzCBMacdougallJELinaclotide is effective for patients with chronic constipationGastroenterology201013888689520045700
- TaghaviSAShabaniSMehramiriAColchicine is effective for short-term treatment of slow transit constipation: A double-blind placebo-controlled clinical trialInt J Colorectal Dis201025338939419705134
- GonenneJCamilleriMFerberIEffect of alvimopan and codeine on gastrointestinal transit: A randomized controlled studyClin Gastroenterol Hepatol20053878479116234007
- CamilleriMAlvimopan, a selective peripherally acting mu-opioid antagonistNeurogastroenterol Motil2005417215716515787936
- PaulsonDMKennedyDTDonovickRAAlvimopan: An oral, peripherally acting, mu-opioid receptor antagonist for the treatment of opioid-induced bowel dysfunction – a 21-day treatment-randomized clinical trialJ Pain20056318419215772912
- PortenoyRKThomasJMoehl BoatwrightMLSubcutaneous methylnaltrexone for the treatment of opioid-induced constipation in patients with advanced illness: A double-blind, randomized, parallel group, dose-ranging studyJ Pain Symptom Manage200835545846818440447
- RaoSSSeatonKMillerMRandomized controlled trial of biofeedback, sham feedback, and standard therapy for dyssynergic defecationClin Gastroenterol Hepatol20075333133817368232
- ChiarioniGWhiteheadWEPezzaVBiofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergiaGastroenterology2006130365766416530506
- ChiarioniGSalandiniLWhiteheadWEBiofeedback benefits only patients with outlet dysfunction, not patients with isolated slow transit constipationGastroenterology20051291869716012938
- HeymenSScarlettYJonesKRandomized, controlled trial shows biofeedback to be superior to alternative treatments for patients with pelvic floor dyssynergia-type constipationDis Colon Rectum2007450442844117294322
- GoJTBrownKSchneiderJCost-effectiveness analysis of office vs home biofeedback in the treatment of dyssynergic defecationAM J Gastroenterol2009104S488
- NyamDCPembertonJHIlstrupDMLong-term results of surgery for chronic constipationDis Colon Rectum19974032732799118740
- HassanIPembertonJHYoung-FadokTMIleorectal anastomosis for slow transit constipation: Long-term functional and quality of life resultsJ Gastrointest Surg2006101013306; discussion 1336–133717175451
- RotholtzNAWexnerSDSurgical treatment of constipation and fecal incontinenceGastroenterol Clin North Am200130113116611394027