Abstract
Objectives
1. To determine if there are differences in the classes of antihypertensive agents prescribed for the elderly population as compared with younger patients. 2. To compare patterns of antihypertensive therapy with established national guidelines.
Design
National Ambulatory Medical Care Survey (NAMCS) database analysis from 1995–2000.
Setting
Multiple outpatient clinic settings in the US.
Participants
Primary care and sub-specialty physicians and their patients.
Measurements
332 510 280 outpatient visits with an ICD-9 code corresponding to a diagnosis of hypertension were analyzed. The class(es) of antihypertensive medications that patients were already taking and/or those added in that visit were noted. Demographics of the patients were also analyzed.
Results
There was a statistically significant association between the prescription of diuretics, calcium-channel blockers (CCBs), alpha-1-blockers (A1Bs), alpha-2 agonists (A2Ags) and age ≥65 years.
Conclusion
Patients aged 65 and over were prescribed different types of medications than those under age 65. Increased usage of diuretics and CCBs were in accordance with evidence-based guidelines for this group. A1Bs were likely used more due to co-morbid benign prostatic hyperplasia (BPH), but this is not certain. The increased prescription of A2Ags likely reflects long-term usage of these medications, which nonetheless may be hazardous due to their potential for causing increased cognitive dysfunction in the aged.
Introduction
Hypertension is commonly encountered in the aging population. The third National Health and Nutrition Examination Survey (NHANES III) found that 65% of individuals over 60 years of age were hypertensive (CitationBurt et al 1995). An analysis of the Framingham database revealed that late middle-aged individuals (between ages 55 and 65) have a residual lifetime risk for hypertension of nearly 90% (CitationVasan et al 2002). Randomized, controlled trial data demonstrate that antihypertensive therapy reduces morbidity and mortality in the elderly (CitationSHEP 1991; CitationStaessen et al 1997; CitationNeal et al 2000). Collectively, these observations suggest that a high proportion of the elderly population will receive antihypertensive therapy.
The means whereby clinicians develop a treatment plan for elderly patients with hypertension is unknown. The aging process is known to be associated with physiologic changes which raise blood pressure including increased arterial vessel stiffness, decreased arterial compliance, reduced beta-adrenergic function, and decreased plasma renin activity (CitationWeber et al 1989; CitationFurmaga et al 1993; CitationLakatta and Levy 2003). The aged population frequently has co-morbid disease and limited financial resources which may impact provider decision-making. Several studies have compared the efficacy of antihypertensive agents in the elderly and therapeutic recommendations based on these studies have been promulgated by different groups, most prominently by the 5th through 7th Joint National Committees on the Detection, Evaluation, and Treatment of High Blood Pressure (JNC 5–7) (CitationJNC 1993, Citation1997; CitationChobanian et al 2003). However, there is limited information on existing patterns of antihypertensive treatment in the elderly.
The present study was therefore undertaken to ascertain the current patterns of antihypertensive therapy in an older as compared with a younger population. We also desired to compare patterns of antihypertensive therapy with recommendations of national committees. For the timeframe of this study, JNC 7 was not yet available and diuretics and beta-blockers (BBs) were the recommended first-line agents by JNC 5 and 6. Also, JNC 6 suggested caution in prescribing either alpha-2 agonists (A2Ags), due to possible resultant cognitive dysfunction, or drugs which “may exaggerate postural changes in blood pressure” (eg, alpha-1 blockers [A1Bs], peripheral adrenergic blockers, and high-dose diuretics).
Methods
Study sample
The National Ambulatory Medical Care Survey (NAMCS) is a survey of office-based physicians in the US which is managed by the Center for Disease Control’s (CDCs) National Center for Health Statistics. It has been conducted annually since 1989. A report describing sample design, sampling variation, and estimation procedures of the NAMCS has been published (CitationNCHS 1998). Non-federally employed physicians from across the US are randomly selected to participate in NAMCS. Physicians may not be selected again for at least 3 years after inclusion in a given year’s sample. Once selected, physicians’ patient encounters are analyzed for a randomly assigned 7-day period of that year. Physicians are asked to comment on various patient characteristics (eg, sex, race, ethnicity) as well as list up to 3 diagnoses for the visit and up to 6 medications “ordered, supplied, administered, or continued” during the visit. In the NAMCS database, the diagnoses are noted according to their ICD-9 codes and the medications have specific numeric codes by which they are listed. Based on the geographic and population data, each site center is designated as urban or non-urban, and its region is designated as Northeast, South, Midwest, or West.
We identified the encounters with an ICD-9 code for essential hypertension (eg, 401.0, 401.1, or 401.9) in the NAMCS database for the years 1995–2000. NAMCS data sets were combined to produce reliable estimates regarding medication usage of the essential hypertensive patient population. We then analyzed the antihypertensive medications listed for these encounters and classified them into the appropriate therapeutic class. The antihypertensive classes identified were A1Bs, A2Ags, angiotensin-converting-enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), BBs, calcium-channel blockers, both dihydropyridine and non-dihydropyridine (CCBs), diuretics, and other (eg, rauwolfia). For combination antihypertensives, we noted the patient was on both classes of medications (eg, lotrel, which is a combination of amlodipine and benazepril, was classified as both a CCB and an ACEI).
Demographic data of the patient sample was also obtained.
Data analysis
Descriptives
The hypertensive patient population (1995–2000) is described by the estimated total patient visits, patient’s gender, race (white, non-white), insurance type (self-pay, all other), region’s population (metropolitan area, non-metropolitan area), geographic location of region (Northeast, Midwest, South, West) as they relate to age (less than 65 years, 65 years of age or older). Proportional comparisons were made using the chi-square test of association. Since the chi-square test determined unadjusted general associations between geriatric age of patient and region, pairwise comparisons were also performed to determine the specific regional differences.
Mantel-Haenszel chi-square tests were performed to determine the associations between geriatric age and the demographic variables of gender, race, insurance type, urban status, and region as stratified by survey year. The results of the stratified analysis indicated similar associations between geriatric age and the demographic variables. Within each year strata, the association between geriatric age and the demographic variables were the same.
Geriatric age
For the analysis, each antihypertensive class was dichotomized into two categories, “medication prescribed” and “medication not prescribed”. Bivariate analyses were first performed to determine unadjusted associations between antihypertensive class and geriatric age. For antihypertensive medications that were statistically associated with age 65 years and over (p≤0.05), multivariate logistic regression analyses were performed to determine adjusted associations between age (<65 years, ≥65 years) and the prescription use of the antihypertensive classes. Each analysis controlled for patient gender, race (white or non-white), insurance type (self-pay, all other), urban status (metropolitan area, non-metropolitan area), geographic region (Northeast, Midwest, South, or West), and NAMCS year (1995–2000).
Prescribing year trend
Prescribing time patterns of each antihypertensive medication class were also explored. First, unadjusted chi-squared analyses determined general associations between year (1995–2000) and each of the antihypertensive medication classes. For the antihypertensive medication classes that were statistically associated with prescribing year (p<0.05), an additional chi-square analysis was performed. This analysis determined if the time trend associations remained when the essential hypertensive population was restricted by age (less than 65 years, 65 years of age or older). These analyses were performed only for hypertensive classes with sample sizes large enough to produce reliable estimates according to National Center for Health Statistics (NCHS) standards (number of sampled patient visits is at least 30 and the relative standard error is less than 0.30). Multivariate logistic regression analysis determined adjusted association between antihypertensive class and prescribing year while controlling for demographic variables discussed above.
SAS-callable SUDAAN software was used to perform each of the statistical procedures. Data were weighted, in accordance with the statistical requirements of the NAMCS database. Statistical associations were determined at the alpha level of 0.05. All estimates reported are reliable by NCHS standards.
Results
Descriptives
Per the NAMCS database, an estimated 332 510 280 essential hypertension patient visits occurred during 1995–2000. The baseline characteristics of this group were assessed (Table ). Of these hypertensive patients, 51.3% were 65 years of age or older. Hypertensive patients 65 years and older were more likely female (63.8% vs 53.2% under age 65; p<0.0001), white (83.2% vs 74.7% under age 65; p<0.0001), insured (2.1% self-pay vs 7.7% self-pay under age 65, p<0.0001) and reside in the Northeast region of the US (23.5% vs 20.0% under age 65; p=0.0054).
Table 1 Demographics of NAMCS database hypertensive patients between 1995–2000 (≥65 years vs <65 years)
Age analysis
Bivariate analyses determined unadjusted statistical associations between the use of diuretics, CCBs, A1Bs, A2Ags and hypertensive patients 65 years of age or older (p<0.05). A higher proportion of elderly hypertensive patients were prescribed or already taking these medications when compared with younger hypertensive patients (Table ).
Table 2 Unadjusted use of medications by NAMCS database hypertensive patients between 1995–2000 (≥65 years vs <65 years)
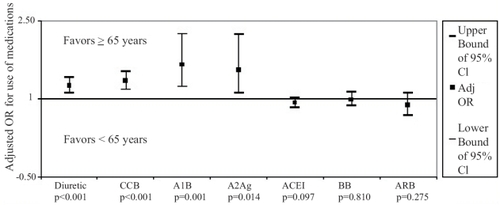
Multivariate analyses determined adjusted associations between the use of diuretics, CCBs, A1Bs, A2Ags, and age category of hypertensive patients (p<0.05). Hypertensive patients who were 65 years of age or older were more likely to be prescribed or already using diuretics (adjusted odds ratio [adj OR] – 65 yrs or older: 1.25, 95% confidence interval [CI] [1.10, 1.41]), CCBs (adj OR – 65 yrs or older: 1.34, 95% CI [1.17, 1.53]), A1Bs (adj OR – 65 yrs or older: 1.66, 95% CI [1.23, 2.24]), or A2Ags (adj OR – 65 yrs or older: 1.56, 95% CI [1.10, 2.23]) when compared with essential hypertensive patients younger than 65 years of age (Figure ).
Figure 1 Adjusted odds ratio for hypertensive medication usage by NAMCS database hypertensive subjects between 1995–2000 (≥65 years vs <65 years old).
Prescribing year trend
Bivariate analyses determined unadjusted statistical associations between the usage of BBs and ARBs among hypertensive patients and prescribing year, (p<0.05, data not shown). The proportion of essential hypertensive patients prescribed BBs appear to decrease between 1995 and 2000; whereas the proportion of essential hypertensive patients prescribed ARBs appear to increase. When the essential hypertensive patient population was restricted to patients 65 years of age or older, there was no statistically significant trend in the prescribing pattern of BBs over the same time period (p=0.11). For ARBs, reliable estimates could not be made due to the small number of ARB prescriptions in the NAMCS essential hypertensive population aged 65 years and older for this time period.
Discussion
Our results demonstrate that hypertensive patients aged 65 and over were treated differently than their younger counterparts in the US from 1995–2000. Those over 65 years of age were most commonly treated with diuretics, CCBs, ACEIs, and BBs, in that order of prevalence. However, the prescription of diuretics, CCBs, A1Bs, and A2Ags was significantly more frequent in the older population than in younger hypertensives. Our theories regarding this discrepant prescribing are detailed below.
Diuretics and CCBs are recommended agents by JNC 6 in the hypertensive elderly population. Their preferential use in the group aged 65 and older may reflect adherence to evidence-based guidelines such as JNC 6. However, CCBs were advocated by JNC 6 as second-line agents in the elderly following diuretics and/or BBs. This study shows that CCBs were preferentially prescribed more often than BBs to all hypertensive patients, regardless of age. At best, physicians were following the evidence in some ways (eg, by prescribing diuretics frequently) while eschewing them in others. Possibly, physician perceptions of frequent BB side effects led to this behavior (CitationUbel et al 2003). Publicity for CCBs by drug representatives may have led to more frequent prescription for the general population, but this does not explain their preferential use in the geriatric population.
Caution is urged in the prescription of A1Bs to the elderly due to potential orthostatic hypotension, and yet these agents were preferentially used in the elderly population. One can surmise this is likely due to the frequent co-morbidity of benign prostatic hyperplasia (BPH) in elderly men. However, it is interesting to note that these medications were specifically noted in a visit coded for hypertension, so some practitioners may have considered these to be good medications for high blood pressure in their elderly male patients regardless of the degree of BPH which was present. Subsequent to the timeframe we were studying, the Antihypertensive and Lipid-lowering Treatment to Prevent Heart Attack (ALLHAT) trial showed increased major cardiovascular events in hypertensive patients treated with an A1B versus a diuretic, and we now know that the A1B medication class should be avoided for hypertension indications alone (CitationALLHAT 2002).
A2Ags were also prescribed preferentially to the geriatric population despite concerns that cognitive dysfunction, notably sedation, may occur when used in this group (CitationJNC 1997). We hypothesize that these medications were prescribed years ago when there were few alternatives and if they were well-tolerated, they were continued by practitioners. We believe that the “grandfathering” of older medications would result in a greater number of geriatric patients on these medications than the younger hypertensive population. Simply put, the longer that someone has been hypertensive, the more likely they are taking an older medication. Clearly, the geriatric population would be more likely to have been hypertensive for a longer period of time than younger adults. One other theory is that the convenience of once-weekly topical dosing options with clonidine patches leads to greater use in older adults who may suffer from memory impairment or difficulties in swallowing pills.
There are several caveats to consider in reviewing our results. Since the source of the data is dependent on multiple doctors’ ICD-9 coding and the medications they chose to list for the visit, the degree of completeness of the data is uncertain. Patients who are hypertensive may not have been included in the database search because the reason for that visit was for a separate issue (eg, ankle sprain). Also, we do not necessarily have a full medication list on our hypertensive patients. The medications listed for each visit in the NAMCS database may be those initiated and/or continued. The discretion of the physician seeing the patient dictated what was listed. Summing the prevalence of the medications prescribed shows patients averaged just over one medication in both elderly and younger adult categories. If a newer medication was added to the prior regimen (eg, CCB added to an existing regimen of BB and diuretic), we could overestimate the relative prevalence of the newer medications compared with the older agents. However, the fact that diuretics were the leading medication listed for the elderly population suggests this is not the case.
We have limited data on patients’ co-morbidities because the physicians in NAMCS could only list up to 3 diagnoses addressed in their patient encounter. This limits our ability to evaluate the appropriateness of medications in patients with “compelling indications”, per JNC 6. For example, if we knew that many of the elderly patients on ACEIs had diabetic nephropathy, there would be excellent evidence for using that medication preferentially in that group. Likewise, if we knew all of the elderly patients on A1Bs had symptomatic BPH, then we would have a reasonable explanation for its prescription.
Data are at least six years old in a rapidly changing field. Although physician’s prescribing practices for hypertension may have changed significantly in the interim, the significant discrepancies between practice guidelines and physicians’ prescribing are still important to recognize. This suggests additional efforts to promote adherence to JNC 7 may be helpful in increasing the practice of evidence-based medicine.
Sampling error is possible with the use of weighted data. This is an inherent limitation of using the NAMCS database as it must be weighted for proper interpretation. It is set up to illustrate nationwide practices and individual patient encounters must be weighted in order to achieve this. We evaluated only the relatively healthy elderly population which is seen in the ambulatory setting. However, we believe this is appropriate for comparing the prescription of antihypertensives in older and younger adult populations, and for considering adherence with JNC 6.
Conclusions
The hypertensive population aged 65 and older was treated with different medications than their younger counterparts in the late 1990s. The increased usage of diuretics and CCBs was evidence-based. However, the greater prevalence of A1B and A2Ag prescription has potential for significant adverse events in this group (CitationJNC 1997; CitationALLHAT 2002). BBs were under-prescribed in the hypertensive population at large, likely due to exaggerated physician beliefs that they are poorly tolerated (CitationUbel et al 2003). Physicians did not adhere to the recommendations of the well-publicized hypertension practice guidelines, JNC 5 and 6. This cross-section of American physician antihypertensive prescribing practices demonstrates the need for continued evidence-based provider education.
Acknowledgements
This research was supported by the Primary Care Research Unit, University of Colorado Health Sciences Center, Denver Colorado and HRSA Administrative Unit Grant #HP00054 5 D12. The authors wish to thank Matthew Huebschmann for his technical support in preparing the manuscript. Financial Arrangements with companies: None for any author. Financial support for this research: None for any author. The support from the Primary Care Research Unit was used to finance costs of accessing the NAMCS database and the services of Caroline Bublitz for research analysis. Consultations or speakers’ forums: None for any author. Company holdings or stocks: None for any author. This information was presented in abstract form at the Society of General Internal Medicine meeting in Vancouver, BC on May 1, 2003.
References
- [ALLHAT] ALLHAT Collaborative Research Group2002Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)JAMA28829819712479763
- BurtVLWheltonPRoccellaEJ1995Prevalence of hypertension in the US adult population: results from the third National Health and Nutrition Examination Survey, 1988–1991Hypertension25305137875754
- ChobanianAVBakrisGLBlackHRNational High Blood Pressure Education Program Coordinating Committee2003The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 reportJAMA28925607212748199
- FurmagaEMMurphyCMCarterBL1993Isolated systolic hypertension in older patientsClin Pharm12347588319419
- [JNC] Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure1993The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V)Arch Intern Med153154838422206
- [JNC] Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure1997The sixth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI)Arch Intern Med1572413469385294
- LakattaEGLevyD2003Arterial and cardiac aging: major shareholders in cardiovascular disease enterprisesCirculation1071394612515756
- [NCHS] National Center for Health StatisticsBryantEShimizuI1998Sample design, sampling variance, and estimation procedures for the National Ambulatory Medical Care SurveyVital and Health Statistics Series 2. No. 108. DHHS Pub. No. (PHS) 88-1382. Public Health ServiceWashingonUS Govt Printing Office
- NealBMacMahonSChapmanN2000Effects of ACE inhibitors, calcium antagonists, and other blood pressure lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists’ CollaborationLancet35519556410859041
- [SHEP] SHEP Cooperative Research Group1991Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension: final results of the Systolic Hypertension in the Elderly Program (SHEP)JAMA2653255642046107
- StaessenJAFagardRThijsL1997Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial InvestigatorsLancet350757649297994
- UbelPAJepsonCAschDA2003Misperceptions about B-blockers and DiureticsJ Gen Intern Med189778314687255
- VasanRSBeiserASeshadriS2002Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart StudyJAMA287197698
- WeberMANeutelJMCheungDG1989Hypertension in the aged: a pathophysiologic basis for treatmentAm J Card6325H32H