Abstract
Study objectives
To verify whether and to what extent the body mass index, airflow obstruction, dyspnea, and exercise capacity (BODE) index correlates with a disease-specific index of health status in patients with COPD.
Design
Cross-sectional study.
Setting
University-affiliated hospital.
Patients
One hundred patients with stable COPD recruited from the outpatient clinic of a single institution.
Measurements
The BODE index was calculated for each patient using variables obtained within 2 weeks of enrollment. At enrollment, all patients completed the St George’s Respiratory Questionnaire (SGRQ). The Kruskal-Wallis test was used to compare health status scores with clinical and functional categories of COPD. The Spearman correlation coefficient (r) was calculated to assess the association between health status scores and clinical or functional variables.
Results
Categorizing the BODE scores into 4 quartiles, we found that higher BODE quartiles were associated with higher (worse) SGRQ scores. The differences among the BODE quartiles in health status indexes were significant for total SGRQ as well as all 3 of the SGRQ sub-scales. In all sections of the SGRQ, scores were moderately to strongly associated with the BODE quartiles (r = 0.27–0.46). In contrast, the association between the SGRQ total, impacts, activity and Global Initiative for Chronic Obstructive Lung Disease (GOLD) stages were weaker (r = 0.27–0.28). There was no significant association between SGRQ symptoms and GOLD stages.
Conclusions
The BODE scoring system corresponds to important differences in health status of patients with COPD. This grading system is better correlated to the health status indexes of the SGRQ than the GOLD staging criteria.
Introduction
Chronic obstructive pulmonary disease has been described as a slowly progressive disorder characterized by airflow obstruction that is not fully reversible (CitationGOLD Expert Panel 2003). The spirometry-derived parameter, the FEV1, is a simple and valid measurement of the degree of airflow obstruction and is often used as a pragmatic surrogate for disease severity in COPD. Nonetheless, COPD is a complex multidimensional disease, and using the degree of airflow obstruction alone to predict outcomes has limitations. FEV1 is known to correlate poorly with patients’ symptoms (CitationMahler et al 1984), quality of life (CitationJones et al 1992), exacerbation frequency (CitationAlsaeedi et al 2002), and exercise intolerance (CitationO’Donnell et al 1998). Hence newer approaches to disease assessment are required and may even supersede the current FEV1-based system of classification of disease severity (CitationCalverley 2004). Recently, the body mass index, airflow obstruction, dyspnea, and exercise capacity (BODE) index, a multidimensional grading system, was shown to be better than the FEV1 at predicting the risk of death among patients with COPD (CitationCelli et al 2004). This multistage scoring system that incorporates an assessment of symptoms, body habitus, and exercise capacity, together with the spirometric measure of airflow (FEV1), can provide useful prognostic information in COPD.
It is increasingly recognized that survival and physiological measures by themselves do not represent the full experiences of patients with COPD. There has been a substantial increase in the use of developed tools that measure health status as clinicians and researchers realize that improving patients’ symptoms, functional status, and quality of life are important goals in the management of COPD (CitationCurtis and Patrick 2003). Although the BODE index has been shown to be a predictor of the risk of death, it is not known whether this index is a useful indicator of patients’ health status as well. Previously, it has been shown that the FEV1-based staging system by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) corresponds to important differences in health status (CitationAntonelli-Incalzi et al 2003). We hypothesized that the BODE index would better correlate with health status in COPD than the FEV1 alone. The purpose of this study is to verify whether and to what extent the BODE index correlates with a disease-specific index of health status in patients with stable COPD.
Methods
Study sample
Between October 2003 and April 2004, patients with a wide range of severity of COPD, regardless of whether they had previous COPD admissions or not, were recruited from a single institution and enrolled in the Health Service Development Program (HSDP) for COPD funded by the Ministry of Health, Singapore. This pilot service project provided several interventions: optimal medication, patient education, home care, and telephonic support, and is aimed at reducing hospitalization for COPD. The main outcome measure monitored in this project was the frequency of hospital admissions for COPD. Patients were recruited from the outpatient clinic. A diagnosis of COPD was established by a respiratory physician based on medical history, current symptoms, and available pulmonary function tests, following the GOLD guidelines (CitationGOLD Expert Panel 2003). All patients had COPD related to smoking. At enrollment, all patients were clinically stable (respiratory symptoms and medication unchanged for at least 4 weeks) and receiving appropriate therapy. The exclusion criteria were an illness other than COPD that was likely to result in death within 2 years; bronchial asthma, defined as an increase in the FEV1 of more than 15% above the baseline value or of 200 mL after the administration of a bronchodilator; an inability to perform the lung function and 6-minute walk tests; a myocardial infarction within the preceding 4 months; unstable angina; or congestive heart failure (New York Heart Association class III or IV). Patients with significant bronchiectasis and/or pulmonary tuberculosis were also excluded. The present study is a cross-sectional analysis of the patients’ baseline variables on entry in the HSDP project for COPD. The study protocol was approved by the institutional ethics committee.
Patient evaluation
At enrollment, all patients completed the Singapore–English or Singapore–Chinese versions of the St George’s Respiratory Questionnaire (SGRQ). The SGRQ is a standardized, self-administered pulmonary-specific health status questionnaire containing 50 items and 76 weighted responses that is divided into 3 subscales: symptoms (8 items), activity (16 items), and impacts (26 items). SGRQ scores were calculated using score calculation algorithms and missing data imputation recommended by its developer. For each subscale and for the overall questionnaire, scores range from zero (no impairment) to 100 (maximum impairment).
The BODE index was calculated for each patient using variables obtained within 2 weeks of enrolment. For calculation of the BODE index, we used the empirical model as previously described (CitationCelli et al 2004) and as shown in : for each threshold value of FEV1, distance walked in 6 minutes, and score on the modified Medical Research Council (MMRC) dyspnea scale (CitationMahler and Wells 1988), the patients received points ranging from 0 (lowest value) to 3 (maximal value). For body mass index the values were 0 or 1. The points for each variable were added, so that the BODE index ranged from 0 to 10 points in each patient. The post-bronchodilator FEV1 as a percent of the predicted value (CitationChia et al 1993) was used and classified according to the 3 stages identified by the American Thoracic Society (CitationATS 1995). The best of two 6-minute walk tests performed at least 30 minutes apart (CitationATS 2002) was used for scoring.
Table 1 Variables and point values used for the computation of the BODE index
Statistical analysis
The Kruskal-Wallis test (with correlation for ties when necessary) was used to compare health status scores with clinical and functional categories of COPD. Differences between stages were assessed using the Mann-Whitney U test. The Spearman correlation coefficient (r) was calculated to assess the association between health status scores and clinical or functional variables. Analysis of data was performed using the Statistical Package for the Social Sciences (SPSS) version10.
Results
One hundred patients were enrolled during the study period. The general characteristics of the patients are summarized in . All patients were either current smokers or ex-smokers. The mean ± SD duration of smoking is 37.4 ± 15.3 years. The minority (16 patients) were current smokers and only 1 patient lived alone. The population was geriatric and poorly educated with only 7 patients having more than 8 years of formal education. The average nutritional status expressed by the body mass index was normal. Five patients had respiratory failure as defined by arterial partial pressure of oxygen (PaO2) less than 60 mmHg with or without arterial partial pressure of carbon dioxide (PaCO2) greater than 50 mmHg while breathing air at sea level. These 5 patients were receiving long-term oxygen therapy. Thirty-eight patients had significant comorbid conditions. The 4 most common comorbid conditions were hypertension (30 patients), ischemic heart disease (18), prostatic hypertrophy (6), and visual impairment (4). shows the classification of patients according to airflow obstruction and BODE index score. The vast majority of patients had moderate to very severe COPD (stages II to IV) according to the GOLD staging of severity.
Table 2 General characteristics of the patientsTable Footnotea
Table 3 Classification of patients according to airflow obstruction and BODE index score
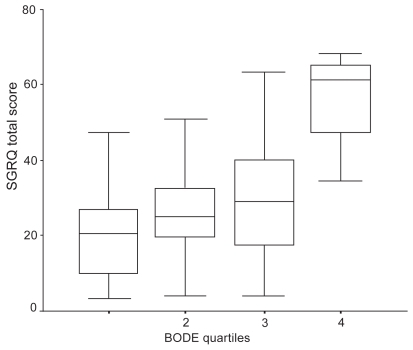
Categorizing the BODE scores into 4 quartiles (CitationCelli et al 2004) as follows: quartile 1 is a score of 0–2; quartile 2 is a score of 3–4; quartile 3 is a score of 5–6; and quartile 4 is a score of 7–10, we found that higher BODE quartiles were generally associated with higher (worse) SGRQ scores (). This pattern is shown clearly by the SGRQ total scores (). The differences among the BODE quartiles in health status indexes assessed by the Kruskal-Wallis test were significant for total SGRQ as well as all 3 of the SGRQ subscales. Post-hoc analysis of the differences between BODE quartiles showed important differences in SGRQ total, activity, and impacts between nonconsecutive quartiles but only between consecutive quartiles 3 and 4. The only consecutive quartiles significantly differing in SGRQ symptoms were quartiles 1 and 2.
Table 4 Mean SGRQ scores by BODE quartiles and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) stagesTable Footnotea
Figure 1 Box plot showing the distribution of St George’s Respiratory Questionaire (SGRQ) scores by BODE quartiles. Error bars show SD; horizontal lines within boxes show the mean.
The differences in health status indexes among the GOLD stages of severity as assessed by the Kruskal-Wallis test was significant for all except the SGRQ symptoms (). The SGRQ total, activity, and impacts scores worsened from stage I to stage IV, but the only consecutive stages differing in these indexes were III and IV.
In all sections of the SGRQ, scores were positively associated with the BODE index quartiles (r = 0.27–0.46). In contrast, the association between the SGRQ total, impacts, activity, and GOLD severity stages were weaker (r = 0.27–0.28). There was no significant association between SGRQ symptoms and GOLD stages ().
Table 5 Correlation between 2 COPD staging systems and St George’s Respiratory Questionnaire scoresTable Footnotea
Discussion
The main finding of this study is that the BODE staging system (CitationCelli et al 2004), which includes in addition to FEV1 other physiologic and clinical variables, corresponds to important differences in health status of patients with COPD. Furthermore, the BODE scoring system is better correlated to health status as assessed by a disease-specific index for COPD than the GOLD staging criteria based largely on the FEV1.
COPD is a complex multidimensional disease, and classification schemes that incorporate more parameters than the degree of airflow obstruction are likely to predict outcomes more accurately (CitationRennard 2004). The multistage scoring system used in this study incorporates variables that can be easily evaluated in any office setting, and the BODE index has potential widespread applicability, just like the FEV1. Important to the acceptance for use of this new classification system is the evidence to support that it provides more useful information than the FEV1 alone. The multidimensional staging system of the BODE index has already been shown to be a superior predictor of the risk of death in COPD patients compared with the FEV1-based staging system by the ATS (CitationCelli et al 2004). Recently the BODE index was also reported to be a much better predictor of the severity in COPD acute exacerbations than the FEV1 (CitationMarin et al 2003). Additionally, the BODE index is also responsive to changes resulting from exacerbations and may capture the impact of exacerbations in patients with COPD (CitationCote and Celli 2004).
The relation between both the ATS and GOLD systems for staging COPD with health status has been examined previously (CitationFerrer et al 1997; CitationAntonelli-Incalzi et al 2003). With both staging systems, the effect of COPD on health status assessed by the SGRQ increases as the disease severity worsens. In a previous study (CitationAntonelli-Incalzi et al 2003), the GOLD staging of COPD corresponded to important differences in health status between stages II and III (previously labeled stages IIa and IIb, respectively), but not between other consecutive stages. The authors concluded that passing the boundary of a FEV1 of <50% of predicted is likely to herald a dramatic decline in health status. We observed a lower potential turning point in the evolution of health status in our study population, ie, between stages III and IV, with no significant change in SGRQ total scores marking the progression of COPD from stage I to III. Differences in study populations may explain these findings. In particular, fewer patients in the present study had significant comorbid conditions compared with previous studies, in part due to the stringent exclusion criteria. Consistent with the GOLD classification, important differences in health status between the highest quartiles (quartiles 3 and 4) of the BODE classification system were observed but not between lower grade consecutive quartiles. This suggests that health status may be relatively preserved in these patients till the disease is very advanced and every effort should thus be made to prevent disease progression even in severe COPD before a dramatic decline of health status occurs.
To our knowledge, this is the first study that has shown the BODE staging system to be generally better correlated with health status than current COPD classification based on the FEV1. Nonetheless, it is noteworthy that the multi-dimensional staging system of the BODE index accounted for a minority of the explained variance in SGRQ total score and health status patterns of consecutive BODE quartiles overlap remarkably. This finding of a great interindividual variability in health status within a given BODE quartile clearly shows that the health status cannot be inferred from the BODE index and should be systematically assessed in the individual patient. Although the findings of the present study are in support of the utility of the BODE index as an assessment tool for COPD patients compared with the sole measurement of airflow obstruction, the BODE index cannot be recommended as a valuable alternative to a disease-specific instrument for evaluation of health status. Further research is needed to verify whether integrating the BODE index with selected measures of health status will allow definition of subgroups with distinctive prognosis. Few interventions can affect the decline of FEV1 in COPD patients but modalities such as medications and exercise training may impact on the other components of the BODE scoring system, namely exercise tolerance and dyspnea level. Prospectively assessing the BODE index in response to treatment or exacerbations will improve knowledge of the BODE classificatory and prognostic implications, as well as of the feasibility of a mixed, ie, physiological-clinical and health-status indicator based COPD staging system. Prospective follow-up studies will also be required for comparison of treatment responses of BODE and SGRQ scores.
Several limitations of this study require discussion. First, survival bias might have attenuated the differences between the most severe cases. Only a longitudinal study can test this hypothesis. Second, the lack of statistically significant differences between consecutive stages other than stages III and IV of the GOLD classification and quartiles 3 and 4 of the BODE staging system does not mean that clinically significant differences were absent. For instance, BODE quartiles 1 and 2 differed in SGRQ total and impacts score by 5 points, ie, of a magnitude over the clinically relevant minimal difference of four (CitationJones et al 1992). Such differences may qualify as statistically significant in a larger population. Third, none of the patients in this study who were recruited from a hospital outpatient clinic were of GOLD stage 0 and hence not all stages of the current GOLD classification that identifies 5 stages of COPD are evaluated here. However, we do not consider that absence of stage 0 is likely to affect the conclusions of this study since stage 0, the presence of symptoms without airflow limitation, was conceived of as an opportunity for early identification of the disease rather than a precursor of illness in all cases in the current form of the GOLD classification (CitationCalverley 2004).
In summary, the BODE scoring system corresponds to important differences in health status of patients with COPD. This grading system is better correlated to health status as assessed by a disease-specific index for COPD than the GOLD staging criteria.
References
- AlsaeediASinDDMcAlisterFA2002The effects of inhaled corticosteroids in chronic obstructive pulmonary disease: a systematic review of randomized placebo-controlled trialsAm J Med113596512106623
- Antonelli-IncalziRImperialeCBelliaV2003Do GOLD stages of COPD severity really correspond to differences in health status?Eur Respir J22444914516133
- [ATS] American Thoracic Society1995Standards for the diagnosis and care of patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med152S771207582322
- [ATS] American Thoracic Society Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories2002ATS statement: guidelines for the six-minute walk testAm J Respir Crit Care Med1661111712091180
- CalverleyPMA2004The GOLD classification has advanced understanding of COPDAm J Respir Crit Care Med1702111215280171
- CelliBRCoteCGMarinJM2004The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary diseaseN Engl J Med35010051214999112
- ChiaSEWangYTChanOY1993Pulmonary function in healthy Chinese, Malay and Indian adults in SingaporeAnn Acad Med Singapore22878848129348
- CoteCGCelliBR2004Effect of exacerbations of COPD (AE) on the multidimensional body mass index (B), airflow obstruction (O), dyspnea (D) and exercise capacity (E), BODE index [abstract]Chest126840S
- CurtisJRPatrickDL2003The assessment of health status among patients with COPDEur Respir J2136s45s
- FerrerMAlonsoJMoreraJ1997Chronic obstructive pulmonary disease stage and health-related quality of lifeAnn Intern Med127107299412309
- GOLD Expert Panel2003Global strategy for the diagnosis, management and prevention of COPDAccessed 2 Feb 2005 URL: http://www.goldcopd.com
- JonesPWQuirkFHBavestockCM1992A self-complete measure of health status for chronic airflow limitationAm Rev Respir Dis145132171595997
- MahlerDAWeinbergDHWellsCK1984The measurement of dyspnea: contents, interobserver agreement, and physiologic correlates of two new clinical indexesChest8575186723384
- MahlerDWellsC1988Evaluation of clinical methods for rating dyspneaChest9358063342669
- MarinJMSanchezAAlonsoJE2003A multivariate grading system (BODE) as predictor of the severity of exacerbation in COPD [abstract]Am J Respir Crit Care Med167A23
- O’DonnellDELamMWebbKA1998Measurement of symptoms, lung hyperinflation, and endurance during exercise in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1581557659817708
- RennardSI2004Looking at the patient – approaching the problem of COPDN Engl J Med350965614999106