Abstract
Objective
To describe the outcome of a one year self-management program (SMG) and a two year pulmonary rehabilitation program (PRG).
Methods
Two open prospective observational studies with 30 patients in each study. SMG had 46 hours over 12 months. PRG had in addition three weekly exercise sessions parallel which lasted an additional year.
Results
In SMG, health-related quality of life (HRQoL, measured by St. George’s Respiratory Questionnaire) had an improvement of −3.6 points (95% CI −6.7 to −0.5) one year after the end of the intervention, but there was no change in the six minutes walking test (6MWT). The PRG had an improvement in HRQoL at the end of the intervention of −11.2 points (95% CI −13.9 to −8.4) and the 6MWT was clinically significant improved with 86 metres (95% CI 63 to 109). None of the groups showed any clinical relevant change in lung function.
Conclusion
Participants in the SMG had had an improvement in quality of life and no deterioration in exercise tolerance one year after the end of the program compared to the start. Participants in the PRG significantly improved their quality of life and exercise tolerance the first year, but had no further clinical relevant improvement the second year.
Introduction
It is estimated that chronic obstructive pulmonary disease (COPD) will rise to a fifth place on the list of the leading causes of disability-adjusted life years (DALYs) in 2020, compared to a 12th place in 1990 (CitationMurray and Lopez 1997). It is consensus that there is a growing need to teach the patients skills to learn to adapt the activities of daily living to their physiological impairment (CitationAmerican Thoracic Society 1999).
There are several forms of interventions for patients with COPD in addition to pharmacological treatment, like self-management education (CitationMonninkhof et al 2003b), pulmonary rehabilitation (CitationLacasse et al 2006), actions plans (CitationTurnock et al 2005), nurse led management (CitationTaylor et al 2005) and smoking cessation (Citationvan der Meer et al 2003).
Based on systematically review of eight studies (CitationMonninkhof et al 2003b), there was found no effect of self-management programs on hospital admission, emergency room visits, days lost from work and lung function, but a trend towards better quality of life. None of these studies had a follow up time longer than 12 months and the majority of studies had interventions with duration of less than 10 hours. We describe the effect one year after the end of a one year (46 hours) self-management program.
The result of a systematic review on pulmonary rehabilitation concluded that this intervention is effective in relieving dyspnoea and fatigue, improving emotional function and enhancing patients’ sense of control over their condition (CitationLacasse et al 2006). Pulmonary rehabilitation programme typically consists of exercise 2–3 times a week for 6–12 weeks (CitationLacasse et al 2004), and there are only a few published studies with longer duration (eg, 6 months (CitationTroosters et al 2000) and one year (CitationEngstrom et al 1999)). There is a lack of data of the ideal length of and required degree of supervision in pulmonary rehabilitation programs (CitationLacasse et al 2006). We describe the effect during a two year pulmonary rehabilitation program including education.
In summary, the aims of the present studies are to describe the outcomes during and one year after the end of a one year (46 hours) self-management program and during and after a two year pulmonary rehabilitation program including education in patients with COPD.
Materials and methods
This was two open prospective observational outcome studies conducted at an out patient department in a hospital in Central Norway from January 2000 to January 2003. The trial was performed according to the principles of the Helsinki-declaration (CitationWorld Medical Association 2004). All who were asked to participate were informed both orally and in writing, and gave a written consent to participate.
Patients
Inclusion criteria for both programs were patients diagnosed with COPD who had a pre-bronchodilator forced expiratory volume in one second (FEV1) lower that 75% of predicted and who had the ability to converse.
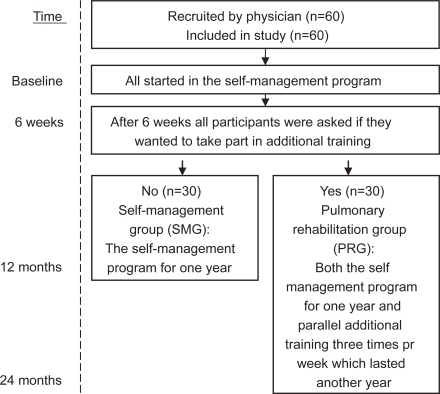
Patients were recruited to a self-management program and informed that they parallel to this could participate in an additional pulmonary rehabilitation program (). This means that the assignment to the groups was based on self-selection and the numbers assigned to each group were not predefined. The main reason for not participating in the additional training was given to be the distance between hospital and home.
The recruitment took place from January 2000 to February 2001 and 60 patients were recruited from the hospital and from local general practitioners. An information sheet describing the intervention and the inclusion criteria was sent to physicians who were asked to recruit participants among their own patients. The referred patients had an initial meeting with the program director where baseline measurements were taken. All the patients invited said yes to participate.
Interventions
The participants were grouped with 5–7 others. Neither age, sex nor the severity of the disease were considered in the setting up of the groups. All patients participated in the same self-management program (). Half the participants chose to only take part in the self-management program and constituted the Self-Management Group (SMG). The other half joined the additional training program and constituted the Pulmonary Rehabilitation Group (PRG). Current smokers in both groups were invited to take part in an individual smoking cessation program.
Description of the self-management program
The self-management program consisted of a combined educational and exercise program with 16 sessions over one year. The 12 first sessions each lasting 3 hours, were given twice a week for 6 weeks. The 13th session lasting 4 hours was held 12 weeks after the start. Session 14 to 16, each lasting 2 hours, were held 24, 36 and 48 weeks after the start. The patient’s partner or a significant other was also invited to attend the course.
The content of the program was constructed through a meeting between participating health care professionals and a group of COPD-patients, some of these newly diagnosed and others more experienced in how the disease affects everyday life. The sessions included both verbal and visual information. In order to facilitate social interactions and sharing of experiences, the patients were encouraged to interact during both the educational and exercise sessions. A patient with COPD, diagnosed since 18 years, participated in the running of all the classes. The participants were encouraged to exercise at home for at least 30 min every day. Patients who did not show up on a session were phoned. The participants could contact the program director between the sessions if needed. All received a specially made booklet with a summary of all the lectures at the end of the course.
In the first 12 sessions, the educational part consisted of information from a medical practitioner, pharmacist, psychologist, occupational therapist, nurse, social worker, physiotherapist and a clinical nutritional physiologist. The first session focused on gaining knowledge of the nature of the disease. During the next three sessions, the content was coping with breathlessness, symptom perception, coping with triggers for breathlessness and physical activity/relaxation. Examples of how to exercise at home were both lectured and practiced. Other topics were oxygen therapy, pulmonary medications, nutrition, ergonomic posture and energy conservation during daily activity. Action plans were individually adjusted for all participants. The content of the last four sessions was decided by the participants themselves and focused mainly on exchanging experiences according to different dyspnoea management strategies and how to cope with COPD.
The last one hour of all the 16 sessions were group exercise lead by a physiotherapist trained in COPD care. The participants were, with physical testing and the baseline data as background information, helped to find their individual exercise intensity. The exercise program included strength training of legs, arms and back and breathing and cardiovascular exercises. During the activities, the instructor always had an individual conversation with each of the participants. In the beginning of the program, it was clearly stated that there would be no high impact exercise in order not to frighten anyone from participating. As the exercise took place at the end of the sessions, the participants were informed to wear loose clothing. To facilitate that all the participants should be able to do the exercises and to avoid that anyone should feel that they were the reason for a break or feel that they did not cope, the exercise was stopped when the poorest was short of breath. In these breaks, breathing exercises were carried out. It was used music to help keep the rhythm. During the instructions the patients and the instructor were placed so that everyone could see each other. When walking, the patients were told to go all over the place and not in a line in order to not make anyone feel that they slowed the others down. Activities which during the exercise were identified by participants as causing dyspnoea were used to practice controlled breathing. Those who could exercise more heavily were encouraged to do so.
Description of the pulmonary rehabilitation program
Those who after the first 6 weeks of the self-management program chose to join the additional training constituted the pulmonary rehabilitation group (PRG) (). They had three weekly one hour exercise sessions parallel to the self-management program the first year and continued with these three weekly sessions an additional year. Two of the three sessions per week were held in the hospital’s gym and the third session took place in the swimming-pool. These sessions were based on the same principles as described above.
Each session in the gym started with 10 minutes of mobility of shoulder, neck and thorax. The next 40 minutes were aimed at endurance training where lower extremity dynamic training was focused, but also arms and back were involved. It was 8 activities per session and in the beginning it was used 30 repetitions per series for 3 series. This was changed gradually down to 8 to 10 repetitions pr series for 5 series with faster speed and heavier weights, to have more strength training. The last 10 minutes were used for stretching and relaxation. Individualized feedback was given during the sessions. During the heaviest parts of the program, alternative exercises were instructed in order to keep everyone occupied.
In the swimming-sessions the foci were endurance, improved mobility in thorax, mobilization of mucus and relaxation. The first 15 minutes were used for warm up, then 30 minutes with endurance training where the resistance of the water was used to increase intensity and finally the last 15 minutes were used for relaxation and stretching.
Smoking cessation
Seven participants, 2 in SMG and 5 in PRG were current smokers. They were offered an individual smoking cessation intervention as part of the program. This program consisted of 16 individual sessions with the program director during six months, each lasting 1 hour. The 6 first sessions were given once a week and the 10 next biweekly. The content was the first year based on a program from Pharmacia and Upjohn. The two last year a program from GlaxoSmithKlines was used. No funding was received from these companies.
Outcome measures
The outcomes were measured at baseline, at 6, 12 and 24 months. The primary outcomes were:
St. George’s Respiratory Questionnaire (SGRQ) (CitationJones et al 1992), Norwegian version (CitationGallefoss et al 1999). The SGRQ is a health-related quality of life disease-specific instrument composed of 76 items that produce scores in the domains: “symptoms”, “activity” and “impact” as well as a total score. The scores for all scales are weighted to range from 0–100, a score of 100 indicating maximum disability. A difference of four units or more indicates a clinically relevant effect (CitationJones 2002).
6-minute walk test (6MWT) to measure exercise tolerance (CitationButland et al 1982; CitationAmerican Thoracic Society 2002). The test was done indoors, the walking course was 45 m in length and the same technician performed all the tests. Verbal cueing was limited to two standardized prompts: “You’re half way done” and “You have one minute to go”. The 6MWT was done about the same time of the day and administered twice at baseline (practise – the best result used), and once on the other time points. A change of 54 m or more in walking distance is considered clinically relevant (CitationRedelmeier et al 1997).
The secondary outcomes were:
Modified Borg scale (MBS) pre, during and post 6MWT (CitationBurdon et al 1982; CitationAmerican Thoracic Society 2002). The highest value, indicating maximum disability, during 6MWT is reported. Borg scale ranges from 0 to 10, where 0 is no problem.
Breathing Problems Questionnaire short version (CitationHyland et al 1998), Norwegian version. (CitationHaave 2003; CitationHaave et al 2005) with 10 items with a possible score between 0 and 30 where 0 is indicates no problem.
COPD Self-Efficacy scale (CSES) (CitationWigal et al 1991). Norwegian short form version (not validated) with 12 questions with a possible score between 0 and 60 where 0 is indicates no problem.
Pre-bronchodilator FVC (Forced vital capacity) % predicted and pre-bronchodilator FEV1 (forced expiratory volume in one second) % predicted (Spirobank G, Ocèan WinSpiro, Roma, Italia).
Arterial saturation (SaO2) (Tuffsat, Datex-Ohmeda, Louisville, USA) during rest.
Number of hospitalizations and days in hospital where the reason for admission in the medical record was exacerbations.
Analysis
Confirmatory testing of the main outcome measure is based on intention to treat, with all patients who started the studies included in the analysis. Missing data for those who died were replaced with the last recorded value carried forward (none was lost to follow up) Data were analysed using general linear model repeated measurement analysis with Bonferroni confidence interval (CI) adjustment in SPSS for Windows version 13.0.1.
Results
The recruitment stopped after 60 patients were included (). 11 were recruited from the hospital and 49 from primary care clinics. 30 patients chose to take part in the additional training (PRG) of which 27 were originally recruited from primary care. 30 chose to participate in the self-management group (SMG). The baseline demographics characteristics are presented in for SMG and for PRG and the baseline values for the outcome measurements are presented in and respectively. The pre-bronchodilator FEV1/FVC was 44% for SMG and 42% for PRG.
Table 1 Baseline demographics characteristics of the participants in the self-management group (SMG) (see for other baseline values). Values are mean for the whole group (standard deviation – SD) or number of persons (percentage – %). N = 30
Table 2 Mean for the self-management group (SMG) at baseline and after 6, 12 and 24 months (standard error – SE)
Table 3 Baseline demographics characteristics of the participants in the pulmonary rehabilitation group (PRG). See also for other baseline values. Values are mean for the whole group (standard deviation – SD) or number of persons (percentage – %). N = 30.
Table 4 Mean values for the pulmonary rehabilitation group (PRG) at baseline and after 6, 12 and 24 months (standard error – SE)
In order to call the self-management program accomplished, the patients had to take part in at least 80% of the whole course. All participants fulfilled this criterion. Three patients (5%) died during the studies. In the PRG one person died of heart failure (10 months after start). In the SMG one died of heart failure (2 months after start) and one of cerebral infarct (11 months after start).
All the seven participants, five in PRG and 2 in SMG, who took part in the smoking cessation program stopped smoking and did not start again during the study time.
Outcome SMG
Regarding the main outcomes, the SMG had a statistical significant and clinical relevant improvement in health-related quality of life (HRQoL) measured with SGRQ half way in the program (6 months) of −4.9 points (95% CI −6.9 to −2.8) (). During the last six months of the program and in the following year the improvement in HRQoL was maintained with a difference between baseline and two years of −3.6 points (95% CI −6.7 to −0.5). There were significant improvements in the SGRQ domains symptom and impact from baseline to six months and these improvements were maintained one year after the end of the program. The SGRQ symptom domain improved with −8.3 points (95% CI −16.1 to −0.5) and impact −5.0 points (95% CI −9.0 to −1.1) from baseline to one year after the end of the program. There was no significant change in the activity domain.
There was no significant change in 6MWD (−12 metres (95% CI −28 to 4) from baseline to one year after the end of the program.
Coping measured by the COPD SE scale improved statistically significant during the intervention with 7.6 points (95% CI 4.4 to 10.8) from baseline to end of intervention, but was at nearly the same level as before the intervention two years from the start. There was no change in Borg score during 6MWT or in hospitalization in the study period.
Lung function measured with FEV1% of predicted showed a small but statistical significant worsening one year after the intervention of −0.5 (95% CI −0.9 to −0.1) compared to baseline. There were no changes in FVC% of predicted. had a slight non-significant improvement after 6 months SaO2 (p = 0.158) but no change between the start of the study to one year after the end.
Outcome PRG
The PRG had a statistical significant and clinical relevant improvement for the primary outcomes at the end of the program (24 months) with a change in SGRQ total score of −11.2 points (95% CI −13.9 to −8.4) and an increased 6MWD of 85.8 metres (95% CI 63.0 −108.7) (). These improvements were both statistical and clinical significant the first 12 months, but no further significant clinical improvements were evident the next 12 months. The SGRQ domains symptom, activity and impact all improved significantly throughout the two years, with the largest improvement after six months. The improvement in each SRGQ domain from baseline to end of program was −13.7 (95%CI −19.9 to −7.5) for symptom, −7.8 (95%CI −11.0 to −4.7) for activity and −13.4 (95%CI −17.9 to −8.8) for impact.
There was also a statistical significant improvement from baseline to end of program (p < 0.037) for BPQ, (CSES), Borg score during 6MWT and number of hospitalizations. The tendency was the same as for the primary outcomes, a significant improvement the first 12 months without any further significant clinical improvement the next 12 months. Number of days in hospital had a trend for a decrease the first year of 2.8 days (95% CI −0.3 to 6.0, p = 0. 094) without any significant change the next year.
There was a small but statistical significant increase in lung function measured by FEV1 % of predicted from baseline to one year of 0.4 (95% CI 0.1 to 0.8, p = 0.017). There was no statistical significant change in FVC%of predicted or SaO2 – rest during the two years.
Discussion
Patients with COPD participating in the one year self-management program (SMG) had an improvement in quality of life and no deterioration in exercise tolerance from the start to one year after the end of the program. Those who took part in the two year pulmonary rehabilitation program (PRG) had a clinical relevant improvement in both quality of life and exercise tolerance the first year which was only slightly improved the second year.
Strengths and limitations
The strength of the present studies is that it mirrors real life. The programs were developed based on clinical experience and in cooperation between experienced COPD patients and clinicians from a range of health professions. An additional strength is the duration of the intervention, the compliance from the patients and the range of measures of the health level.
There are several limitations to these studies. They are neither randomised nor controlled and like all uncontrolled observational studies, there is no way of controlling to what degree the improvements reported by the patients are attributed to the programs. The patients were mainly recruited from general practice and this could lead to a selection of patients who were not optimally treated. Furthermore, those volunteering to take part in the studies could be more motivated to do something about their own health. Both these factors could contribute to a better outcome of the programs than could have been observed with other groups of patients with COPD. Having this in mind, the next paragraphs will discuss some of the findings in these studies.
Self-management
Compared with other studies of self-management (CitationMonninkhof et al 2003b), the program in the present study was more comprehensive both regarding the duration of the intervention (46 hour during 1 year) and in that 35% of the program were exercise sessions. Therefore the results are not directly comparable but it seems as the same tendency is found both in the review and in the present study; self-management programs mainly improve quality of life. It is noteworthy that the observed development in quality of life measured with SGRQ, with a worsening of 1 point during the year after the end of the intervention, was smaller than the worsening of 3.2 points pr year that was observed for the placebo group in the ISOLDE study where the participants had the same pre-bronchodilator FEV1 as participants in the present study (1.20 litres in our study and 1.23 litres in the ISOLDE study) (CitationBurge et al 2000).
Pulmonary rehabilitation
The main finding in this study is that it indicates that there is no further clinical relevant improvement of continuing the pulmonary rehabilitation program after the first year, but the additional year may ensure that the gained effect is maintained. It might be likely that the gained effect would diminish, but it could also be that the participants would continue to exercise even outside a program as they already had gotten into the habit of regular exercising.
Based on the systematic review of pulmonary rehabilitation programs, we calculated that the average increase in 6MWT for those in the intervention groups was 46.0 metres (16 studies, intervention length of 4 to 52 weeks with a median of 8. 5 weeks) (CitationLacasse et al 2006). This is a similar increase as the one observed after six months in the present study (43 metres), a result which was doubled after one year. This could indicate that in order to maximise physical endurance in this group of patients, pulmonary rehabilitation programs should last for at least one year.
A randomised study with an educational intervention over four months and a fitness program lasting two years (although using self-management in the title), found no effect of the intervention (CitationMonninkhof et al 2003a). However at baseline the participants in the present study had more severe COPD with a mean FEV1 of 41% predicted compared to 56% in the Dutch study. This could indicate that extensive programs have a better effect for patients with more severe COPD. This suspicion is strengthened by another recent study with a mean baseline FEV1 of 55% predicted that also failed to show an effect (CitationWadell et al 2004), while an US study with baseline FEV1 of 45% of predicted, found an effect (CitationCarrieri-Kohlman et al 2005).
Conclusion
There is no agreed standard regarding what is to be viewed as self-management or pulmonary rehabilitation programs and the terms. If one should try to distinguish between them based on the literature it might be said that self-management include education that focus on self-management skills (self-efficacy) while pulmonary rehabilitation focuses on exercise. A recent study highlights the importance of linking self-efficacy with physical function, as it was found that self-efficacy explained the main part of self-reported physical functioning (CitationArnold et al 2005). Our clinical interpretation of the present studies is that programs should combine comprehensive educational intervention with extensive supervised exercise for at least one year of length for optimal results. There is a need for more research on the long-term effect of such programs.
Disclosure
Borghild K. Lomundal has no conflicts to disclose. Aslak Steinsbekk has no conflicts to disclose. Sources of support: The Norwegian Foundation for Health and Rehabilitation and the Central Norway Health Authorities.
References
- American Thoracic Society1999Pulmonary Rehabilitation–1999American Journal of Respiratory and Critical Care Medicine15916668210228143
- American Thoracic Society2002ATS statement: guidelines for the six-minute walk testAm J Respir Crit Care Med1661111712091180
- ArnoldRRanchorAVDeJongsteMJ2005The relationship between self-efficacy and self-reported physical functioning in chronic obstructive pulmonary disease and chronic heart failureBehav Med311071516252622
- BurdonJGJuniperEFKillianKJ1982The perception of breathlessness in asthmaAm Rev Respir Dis12682587149447
- BurgePSCalverleyPMJonesPW2000Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trialBMJ32012970310807619
- ButlandRJPangJGrossER1982Two-, six-, and 12-minute walking tests in respiratory diseaseBr Med J (Clin Res Ed)28416078
- Carrieri-KohlmanVNguyenHQDonesky-CuencoD2005Impact of Brief or Extended Exercise Training on the Benefit of a Dyspnea Self-management Program in COPDJ Cardiopulm Rehabil252758416217231
- EngstromCPPerssonLOLarssonS1999Long-term effects of a pulmonary rehabilitation programme in outpatients with chronic obstructive pulmonary disease: a randomized controlled studyScand J Rehabil Med312071310599897
- GallefossFBakkePSRsgaardPK1999Quality of life assessment after patient education in a randomized controlled study on asthma and chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1598121710051255
- HaaveE2003Selvopplevd helsestatus og forventet mestring av pustevansker hos pasienter med KOLS [Patient reported health status and anticipated coping of breathibng problems in COPD]Lungeforum13239
- HaaveEHylandMEEngvikH2005Physical and emotional aspects of self-reported health status: a two-factor model of the short-form Breathing Problems QuestionnaireChron Respir Dis221616279745
- HylandMESinghSJSodergrenSC1998Development of a shortened version of the Breathing Problems Questionnaire suitable for use in a pulmonary rehabilitation clinic: a purpose-specific, disease-specific questionnaireQual Life Res7227339584553
- JonesPW2002Interpreting thresholds for a clinically significant change in health status in asthma and COPDEur Respir J1939840411936514
- JonesPWQuirkFHBaveystockCM1992A self-complete measure of health status for chronic airflow limitation. The St. George’s Respiratory QuestionnaireAm Rev Respir Dis145132171595997
- LacasseYGoldsteinRLassersonTJ2006Pulmonary rehabilitation for chronic obstructive pulmonary diseaseCochrane Database Syst Rev4CD00379317054186
- LacasseYMaltaisFGoldsteinRS2004Pulmonary rehabilitation: an integral part of the long-term management of COPDSwiss Med Wkly134601515592953
- MonninkhofEMvan der ValkPDvan der PalenJ2003aEffects of a comprehensive self-management programme in patients with chronic obstructive pulmonary diseaseEur Respir J2281520
- MonninkhofEMvan der ValkPDvan der PalenJ2003bSelf-management education for chronic obstructive pulmonary diseaseCochrane Database Syst Rev1CD002990
- MurrayCJLopezAD1997Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease StudyLancet34914985049167458
- RedelmeierDABayoumiAMGoldsteinRS1997Interpreting small differences in functional status: the Six Minute Walk test in chronic lung disease patientsAm J Respir Crit Care Med1551278829105067
- TaylorSJCandyBBryarRM2005Effectiveness of innovations in nurse led chronic disease management for patients with chronic obstructive pulmonary disease: systematic review of evidenceBMJ33148516093253
- TroostersTGosselinkRDecramerM2000Short- and long-term effects of outpatient rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trialAm J Med1092071210974183
- TurnockACWaltersEHWaltersJA2005Action plans for chronic obstructive pulmonary diseaseCochrane Database Syst Rev4CD00507416235392
- van der MeerRMWagenaEJOsteloRW2003Smoking cessation for chronic obstructive pulmonary diseaseCochrane Database Syst Rev2CD00299912804448
- WadellKSundelinGHenriksson-LarsenK2004High intensity physical group training in water – an effective training modality for patients with COPDRespir Med984283815139572
- WigalJKCreerTLKotsesH1991The COPD Self-Efficacy ScaleChest99119362019177
- World Medical AssociationWorld Medical Association Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects [online]. Accessed 9-10-2004. URL: http://www.wma.net/e/policy/b3.htm