Abstract
Purpose:
To report on keratoectasia after laser in situ keratomileusis (LASIK) in two eyes of two patients who had no obvious preoperative risk factors, and treatment of keratoectasia by intrastromal corneal ring segments.
Method:
Clinical interventional case report.
Results:
Two patients underwent LASIK in both eyes at Shinagawa LASIK center, Tokyo. Preoperative standard ophthalmological examinations demonstrated no specific risk factors of keratoectasia. However, each eye of the two patients developed keratoectasia as defined by corneal topography. Treatment for keratoectasia was performed by inserting intrastromal corneal ring segments (ICRS) in the affected eyes. In one eye, KeraRing (MEDIPHACOS, Ltd, Brazil) was inserted, and Intacs SK (Addition Technology Inc, USA) was inserted in the other.
Conclusion:
Even in eyes where no risk factors for keratoectasia were found following thorough preoperative examinations, keratoectasia could develop after LASIK. ICRS could be effective for the treatment of keratoectasia after LASIK.
Introduction
Keratoectasia (corneal ectasia) is known as one of the most unfavorable complications after laser in situ keratomileusis (LASIK). There is increasing concern regarding risk factors for developing keratoectasia after LASIK. Keratoconus and pellucid marginal degeneration as demonstrated by corneal topographyCitation1,Citation2 are among significant risk factors for the development of post-LASIK keratoectasia. Besides these two diseases, a variety of other risk factors have also been reported including preoperative topographic abnormalities, low residual stromal bed thickness (RSBT), thin corneal thickness (CT), age younger than 30 years, and Sphere Equivalent (SE).Citation3 In this report, we present two eyes of two patients that developed keratoectasia after LASIK even though their preoperative risk was low as identified by the Ectasia Risk Score System.Citation3 In addition, both patients’ corneal topographies were evaluated using Pentacam (70700 OCULUS, Wetzlar, Germany), TMS-4 (TOMEY Corp, Nagoya, Japan), OPD-Scan (ARK10000 NIDEK Co, Ltd, Aichi, Japan), and Orbscan (Bausch and Lomb, Salt Lake City, UT, USA) in order to detect patients that might develop advanced keratoconus.Citation4 Slitlamp assessments showed that both eyes were normal. Preoperative central corneal thickness (CCT) was over 500 μm, RSBT was greater than 250 μm, and both patients were considered to be good candidates for LASIK according to generally accepted criteria.Citation5
Case report
Patient 1
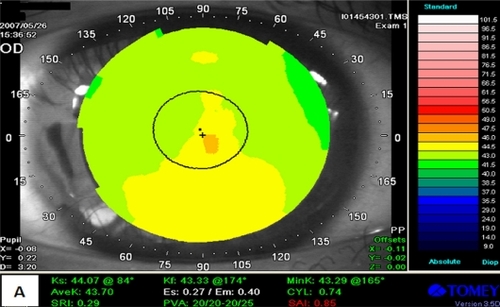
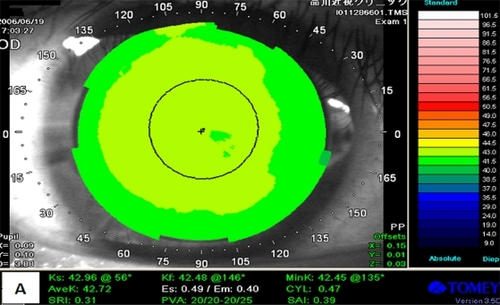
A 24-year-old male underwent bilateral LASIK in June 2007 at Shinagawa LASIK Center in Tokyo, Japan. Preoperatively, his uncorrected visual acuity (UCVA) was 20/400 in the right eye and 20/320 in the left. His best spectacle-corrected visual acuity (BSCVA) was 20/16 with a manifest refraction of −5.75D−0.75D × 155° in the right eye and 20/16 with a manifest refraction of −5.25D−1.0D × 5° in his left. The intraocular pressure (IOP) was 13.4 mmHg and 11.8 mmHg, central corneal ultrasound pachymetry was 512 μm and 523 μm, RSBT was 327 μm and 345 μm, corneal endothelial cell destiny was 2,817/mm2 and 2,618/mm2, and the mean keratometry (K) value was 43.75 D and 43.75 D in the right and left eyes, respectively. No abnormal preoperative findings were observed (), and the slitlamp examination also showed both eyes to be normal.
At his one-week follow-up examination post-LASIK, the UCVA in both eyes were 20/10. At his ten-month examination post surgery, his UCVA was 20/20 in the right eye and 20/13 in the left eye.
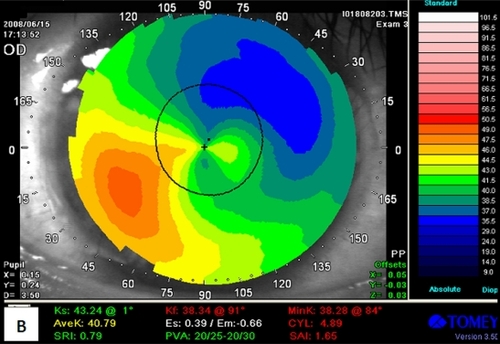
In July 2008, the patient returned to our clinic reporting a decrease in the visual acuity of his right eye, but no problems in his left eye. Corneal topographic examinations showed inferior steepening in the right eye (). The patient was prescribed hard contact lenses (HCLs), and eye drops of timolol maleate and latanoprost were administrated in both eyes. However, for several months the patient did not wear the prescribed HCLs and missed our follow-up examinations.
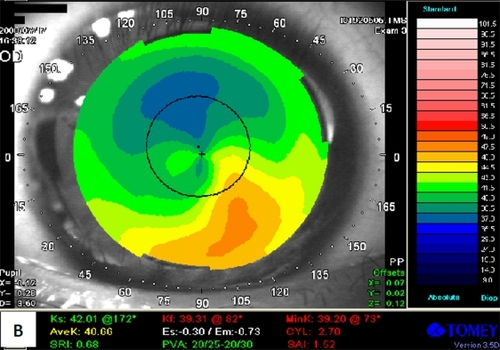
In July 2009, he returned again to our clinic with further declined vision in the right eye. Corneal topographical examinations showed the development of progressive keratoectasia in his right eye but no changes in the left eye. In the right eye, UCVA was 20/700 and BSCVA was 20/12.5 with a manifest refraction of +2.00D−6.5D × −85°. The IOP was 7.4 mmHg, central corneal ultrasound pachymetry 378 μm, corneal endothelial cell destiny 2,762/mm2, and the mean K value was 48.75D in the right eye.
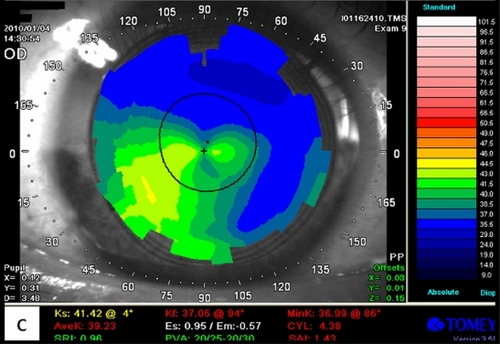
In order to treat keratoectasia, KeraRings (MEDIPHA-COS, Ltd, Brazil) was implanted in the right eye (). The channels for KeraRings ICRS were created by IntraLase FS60 (Advanced Medical Optics Inc, CA, USA) with 1.50 μJ for the ring energy and 1.50 μJ for the entry cut energy. The inner diameter was set to 4.9 mm and its outer diameter 5.8 mm. The channels’ entry cut thickness was 1 μm, the incision Axis was 180° and the depth in the cornea was 315 μm. The implantation of the two KeraRings ICRS was as follows. Superior ICRS: thickness = 150 μm; arc length = 90°; apical diameter = 5 mm. Inferior ICRS: thickness = 300 μm; arc length = 160°; apical diameter = 5 mm. One month after the KeraRings implantation, his UCVA had improved to 20/25 in his right eye, and shows the improvement of the corneal curvature post KeraRing implantation.
Patient 2
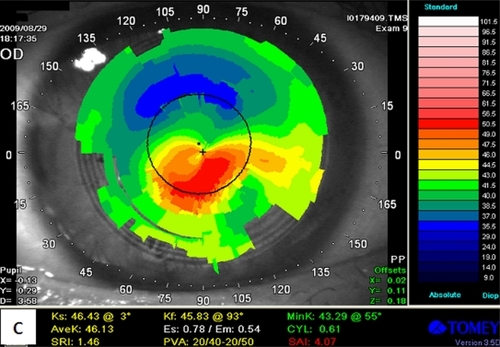
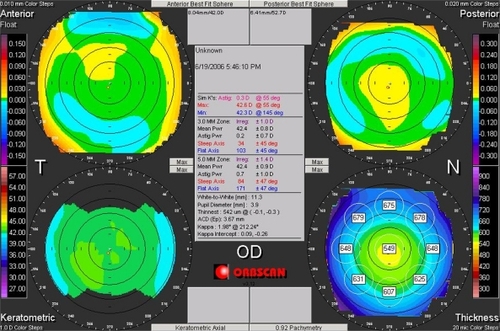
A 29-year-old male underwent bilateral LASIK in June 2006 at Shinagawa LASIK Center. Preoperatively, his UCVA was 20/250 in the right eye and 20/320 in the left. The BSCVA was 20/12.5 with a manifest refraction of −7.25D−0.25D ×95 ° in the right eye and 20/12.5 with a manifest refraction of −7.50D−0.50D × 180° in the left. IOP was 13.4 mmHg and 13.1 mmHg, central corneal ultrasound pachymetry 539 μm and 543 μm, RSBT 337 μm and 338 μm, and the mean K value was 42.50D and 43.00D in the right and left eyes, respectively. The preoperative topography was normal and showed no sign of keratoconus ( and ). Slitlamp examination showed both eyes to be normal. The day after LASIK, the UCVA and BSCVA were 20/16 in both eyes. The patient did not return to our clinic for follow-up examinations.
He returned to our clinic in June 2008, 2 years after LASIK, complaining of progressive loss of visual acuity in the right eye. The UCVA was 20/25 and BSCVA was 20/12.5 with a manifest refraction of −1.00D−0.5D × 105° in the right eye. Corneal topography demonstrated inferotemporal steepening in the right eye (). He started to wear HCL in the right eye, and hyaluronate sodium (0.1%), timolol maleate, and Latanoprost eye drops were prescribed for both eyes.
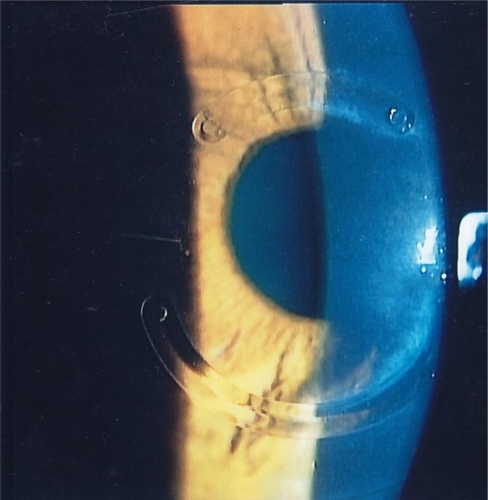
Because the right vision did not improve, Intacs SK (Addition Technology Inc USA) implantation was performed in December 2008 (). Before the Intacs SK implantation, his UCVA was 20/32 and BSCVA was 20/16 with a manifest refraction of −1.00D−4.25D × 90° in the right eye. Central corneal ultrasound pachymetry was 406 μm, endothelial cell destiny 2,907/mm2, and the mean K value was 41.50 D in the right eye.
The Intacs SK ICRS channels were created using IntraLase FS60 with 1.80 μJ for the ring energy and 1.50 μJ for the entry cut energy. The inner and outer diameters or the channel were 6.0 mm and 6.8 mm, respectively. The channel’s entry cut thickness was 1 μm, the incision Axis 20°, and the depth in the cornea was 314 μm. Two identical Intacs SK of 400 μm ICRS thickness and 150°arc length were implanted superiorly and inferiorly. After the Intacs SK implantation, the patient used the prescribed soft contact lenses (SCL).
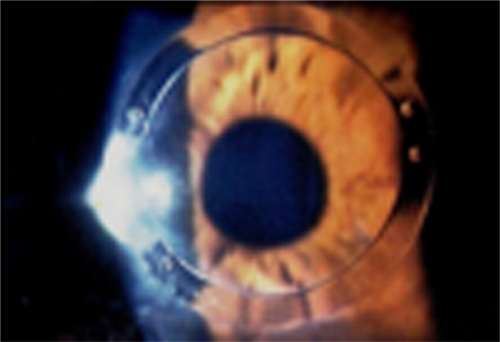
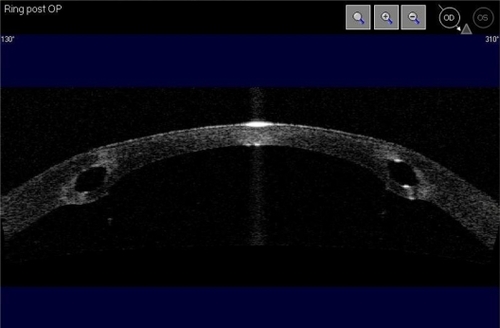
At the one-week follow-up examination, his UCVA was 20/32 and BSCVA was 20/16 with a manifest refraction of −1.0−1.50 × 70 in his right eye. Three months after implantation, the corneal topographical examination revealed improvement, although central steepening was still observed (). His UCVA and BSCVA were 20/32 and 20/16 with a manifest refraction of 0D−5.00D × 90°, respectively. An anterior segment imaging was obtained using Visante™ OCT (Carl Zeiss Meditec Inc, Jena, Germany), which showed the positioning of ring segment was good (). However, induced astigmatism was present in his right eye.
Discussion
LASIK has been recognized as a safe, effective, and predictable surgical procedure to treat refractive errors, and is the most commonly performed worldwide. However, there is the possibility of post-LASIK induced keratoectasia for these patients. Even after passing strict screening criteria prior to LASIK, there are still unknown risk factors.Citation6,Citation7 Significant risk factors have been identified for the development of keratoectasia after LASIK. These include topographic diagnosis, high refractive errors, younger age, thin RSBT, and thin central CT. In order to avoid the development of keratoectasia, these exclusion criteria may need to be expanded. In this report we described two patients who developed keratoectasia after LASIK even though thorough preoperative examinations indicated no specific risk factors. The two patients were treated by intrastromal corneal ring segments (KeraRing and Intacs SK for each patient) to correct post-LASIK keratoectasia.Citation8–Citation10
Patient 1 achieved UCVA of 20/25 at one month after ring implantation in his affected eye; however, his UCVA decreased to 20/125 at his 5-month examination. In Patient 1, a certain improvement of visual acuity was observed after intrastromal ring implantation, but then myopic regression gradually developed, and corneal steepening was progressive over time. Continued examinations and follow-up treatments using cross linking or phakic IOL will be considered for Patient 1.
For Patient 2, after the Intacs SK surgery in his right eye, his UCVA was 20/32 at his 7-month examination. One year after the Intacs SK implantation, Patient 2’s UCVA remained 20/32. Intacs SK ICRS had an effect on Patient 2 significantly.
In conclusion, post-LASIK keratoectasia can occur even in patients without specific risk factors. There have been recent reports showing that measurement of corneal hysteresis (CH) and corneal resistance factor (CRF) with the Ocular Response Analyzer (ORA) can detect early keratoectasia.Citation11–Citation13 In order to decide proper indications of LASIK, surgeons should take CH and CRF values into consideration besides current standard preoperative screening examinations.
Disclosure
The authors have no financial interests in the materials or products presented herein.
References
- AmbrósioRJrWilsonSEEarly pellucid marginal corneal degenerationCornea200221111411711805521
- HolladayJTKeratoconus detection using corneal topographyJ Refract Surg200925958962
- RandlemanJBTrattlerWBStultingRDValidation of the ectasia risk score system for preoperative laser in situ keratomileusis screeningAm J Ophthalmol2008145581381818328998
- ErtanAKamburogluGColinJLocation of steepest corneal area of cone in keratoconus stratified by age using pentacamJ Refract Surg2009251012101619921770
- KymionisGDBouZoukisDDiakonisVLong-term results of thin corneas after refractive laser surgeryAm J Ophthalmol2007144218118517533106
- KleinSREpsteinRJRandlemanJBStultingRDCorneal ectasia after laser in situ keratomileusis in patients without apparent preoperative risk factorsCornea200625438840316670474
- BinderPSLindstromRLStultingRDKeratoconus and corneal ectasia after LASIKJ Refract Surg20052174975216329368
- CarrasquilloKGRandJTalamoJHIntacs for keratoconus and post-LASIK ectasia mechanical versus femtosecond laser-assisted channel creationCornea200726895696217721296
- SansanayudhWBaharIKumearNLIntrastromal corneal ring segment SK implantation for moderate to severe keratoconusJ Refract Surg201036110113
- CoskunsevenEKymionisGDNikolaosSOne-year results of intrastromal corneal ring segment implantation (KeraRing) using femtosecond laser in patients with keratoconusAm J Ophthalmol2008145577577918291344
- KerautretJColinJTouboulDRobertsCBiomechanical characteristics of the ectasic corneaJ Cataract Refract Surg20083451051318299080
- LiuRChuRYZhouXTQuXMDaiJHWangLA compare study on cornea biomechanical properties in normal and keratoconic eyesZhonghua Yan Ke Za Zhi200945650951319957673
- KirwanCO’MalleyDO’ KeefeMCorneal hysteresis and corneal resistance factor in keratoectasia: findings using the Reichert Ocular Response AnalyzerOphthalmologia20082225334337 Epub 2008 Jul 15.