Abstract
Purpose:
To compare the effectiveness of standard revision surgery using mitomycin C (MMC) with revision using amniotic membrane transplantation and MMC for elevated intraocular pressure (IOP) after trabeculectomy.
Patients and methods:
A retrospective, nonrandomized comparative study of 36 eyes of 36 patients with a failed trabeculectomy. Patients were divided into two groups, ie, a nonamnion-transplanted group and an amnion-transplanted group. The amniotic membrane was placed on the scleral flap under the conjunctiva in the amnion-transplanted group. Both groups recovered filtration of aqueous humor from the surgical site with the adjunctive use of MMC. The changes in IOP and cumulative survival rate were compared for the two groups. Success was defined as a 30% reduction in IOP from the preoperative IOP and maintenance below 21 mmHg with or without the use of antiglaucomatous agents.
Results:
The mean preoperative IOP was not significantly different in the two groups. The mean postoperative IOP in the nonamnion group, 12.1 ± 5.5 mmHg, was significantly lower than the IOP in the amnion group, 16.0 ± 3.7 mmHg. Survival curves in the two groups did not reach significantly different levels.
Conclusions:
Conventional surgical bleb revision with MMC can significantly reduce the elevated IOP associated with a failed filtration bleb. The use of an amniotic membrane transplant did not improve the surgical outcome in our cases.
Introduction
Trabeculectomy has been the surgery of choice in eyes with glaucoma since it was first described by Cairns in 1968.Citation1 Antifibrotic drugs, such as 5-fluorouracil and mitomycin C (MMC), have been commonly used adjunctively to prevent scar formation, and they have increased the success rate of trabeculectomy. However, there is still a low but unacceptable rate of failure of trabeculectomy because of progressive scarring of the subconjunctival tissues. Patients with secondary glaucoma, aphakia, and prior surgery to the conjunctiva are reported to have poorer success rates following trabeculectomy.Citation2
When filtration surgery fails to reduce the intraocular pressure (IOP), a revision of the bleb is one of the options. Several investigators have advocated bleb revision with adjunctive 5-fluorouracil or MMC,Citation3 while others have advocated the use of an amniotic transplant.Citation4–Citation7 The amniotic membrane is the innermost layer of the three-layered fetal membrane, and has anti-inflammatory, antifibrotic, and antiangiogenic properties.Citation8,Citation9 Amniotic membranes have been transplanted to reconstruct the ocular surface after pterygium excisionCitation10 and in nonhealing corneal epithelial defects.Citation11 Nagai-Kusuhara et al reported that the use of an amniotic membrane for reconstructing a filtration bleb is useful for late-onset bleb leaks.Citation12 Because of its ability to suppress wound healing, amniotic membrane transplantation has been used in glaucoma-filtering surgery to prevent subconjunctival fibrosis.Citation4–Citation7
The purpose of this study was to assess the effectiveness of conventional surgical revision using adjunctive MMC with that of bleb revision using adjunctive MMC and transplantation of an amniotic membrane in lowering IOP.
Material and methods
The medical charts of 36 eyes of 36 patients who had undergone trabeculectomy and bleb revision by a single surgeon (YK) at the Otemae Hospital from February 2003 to July 2006 were reviewed. This study was approved by the Otemae Hospital Institutional Review Board, and the procedures used conformed to the tenets of the Declaration of Helsinki. Informed consent for the surgery had been obtained in all cases.
Two groups were compared; there were 24 eyes in the nonamnion-transplanted groups and 12 eyes in the amnion-transplanted group. The patients in the nonamnion group had conventional bleb revision with adjunctive MMC between February 2003 and July 2005. The remaining 12 patients had bleb revision with amniotic membrane transplantation and MMC between August 2005 and July 2006.
The surgical procedures were slightly modified from those reported by Drolsum et al.Citation6 For the surgery, the conjunctiva was anesthetized with a 1 mL injection of 2% xylocaine, and a conjunctival incision was made approximately 9 mm from the limbus or at the limbus. All of the cases in the nonamnion group had limbus-based surgery. For this, the conjunctiva was separated from the sclera, and the scar tissue was dissected from the scleral surface both anteriorly and posteriorly. After applying 0.4 mg/mL MMC to the sclera for five minutes, the surgical area was irrigated with 100 mL of balanced salt solution. The wall of the bleb or fibrotic membrane on the scleral flap was reopened as confirmed by the leakage of aqueous humor. The conjunctiva was closed with a 10-0 nylon running suture.
The amniotic membrane was obtained under sterile conditions after a cesarean delivery and cryopreserved at −80°C in dimethyl sulfoxide until immediately before use. In the amnion group, a piece of amniotic membrane measuring approximately 7 × 10 mm was placed with the epithelial side over the scleral flap. Six of 12 cases (50%) in the amnion group had limbus-based surgery, and the remaining six cases had fornix-based surgery. The amniotic membrane was sutured to the sclera at the corneoscleral limbus using 8-0 virgin silk. The fornix side of the amniotic membrane was inserted beneath the healthy conjunctiva posterior to the conjunctival incision line or scar line. Then two to three sutures were placed 5 mm from the limbus to fix the amniotic membrane to the sclera. The fornix end of the membrane was not sutured. Then the limbus-based conjunctival flap was closed, as was done in the nonamnionic group. The fornix-based flap was closed by interrupted sutures at the limbus.
Postoperatively, all patients received similar topical medical regimen; 0.1% topical betamethasone and 0.5% levofloxacin for six weeks to three months which was reduced within three months, depending on the degree of inflammation. Patients were examined monthly for the first 3 months, and every 2–3 months thereafter.
The success of these surgical procedures was compared using Kaplan-Meier lifetable analysis. Success was defined as a 30% reduction of the IOP from the preoperative IOP and maintenance below 21 mmHg with or without the use of antiglaucoma agents. When additional surgery was performed, the IOP control was judged as a failure regardless of IOP at the time of the decision.
Survival curves were constructed for the two groups. The significance of the differences in success was determined using the log rank test. When the IOP was higher than the targeted pressure in two consecutive examinations, the bleb was considered to have failed. When additional glaucoma surgery was performed, the IOP control was judged as a failure regardless of the IOP level at the time of the decision.
The significance of the differences in the demographic characteristics of the subjects and the incidence of surgical complications were determined using Mann-Whitney U tests and Fisher’s Exact probability tests. The IOP changes were evaluated using Mann-Whitney tests and Wilcoxon signed-rank tests. A P value of <0.05 was considered statistically significant.
Results
The demographic data of the patients are summarized in and . There were no significant differences in age, duration of follow-up, preoperative IOP, number of prior surgeries, number of prescribed antiglaucoma medications, and type of glaucoma between the nonamnion amnion groups.
Table 1 Patient demographics
Table 2 Type of glaucoma
The pretrabeculectomy (former trabeculectomy before revision) IOPs were 21.2 ± 4.0 mmHg in the nonamnion group and 21.8 ± 3.8 mmHg in the amnion group.
The mean prebleb revision IOP was 21.4 ± 6.5 mmHg in the nonamnion group and 21.8 ± 4.6 mmHg in the amnion group. The postoperative IOP at the last visit in the nonamnion group was 12.1 ± 5.5 mmHg and that in the amnion group was 16.0 ± 3.7 mmHg. In each group, the IOP was reduced significantly, although the IOP in the nonamniotic group was significantly lower than that in the amniotic group (P = 0.025). The number of postoperative antiglaucoma eye drops was 0.24 ± 0.60 in the nonamnion group and 0.58 ± 0.79 in the amnion group (P = 0.105).
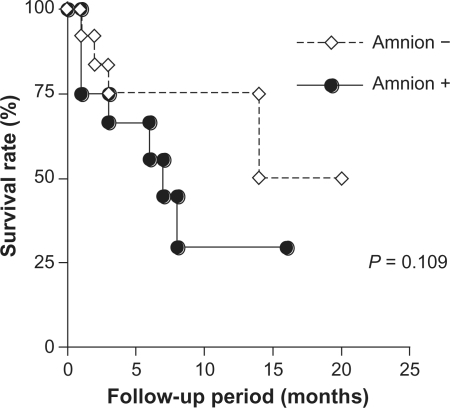
In the amnion group, Kaplan-Meier lifetable analysis showed that the success rate was 58.3% after six months and 21.9% after one year. The success rate in the nonamnion group was 74.8% from six months to one year after surgery. This difference in the surgical outcome was not significant (P = 0.109, see ).
Figure 1 Kaplan-Meier survival curves of the amnion and nonamnion transplant groups. A plot of the cumulative probabilities against time that the intraocular pressure was 30% lower than at baseline.
At the final visit, five eyes had survived in the amnion group according to our criterion for success. Two had a fornix-based conjunctival flap, and three had a limbus-based flap.
The postoperative complications are listed in . Two cases of hyphema were seen in the nonamnion group and one in the amnion group. Leakage at the wound edge developed in one case in the nonamnion group and three cases in the amnion group. Conjunctival sutures were used to repair the wound leakage. Hyphema, shallow anterior chamber, and choroidal detachment resolved without any intervention.
Table 3 Postoperative complications
Late complications of trabeculectomy such as hypotonic maculopathy, late bleb leak, bleb-associated infection, and corneal decompensation were not found in any of our patients.
Although appearance of the bleb is an important factor that predicts IOP results and bleb-related complications, we did not evaluate bleb appearance in this study. All of the subjects had had ocular surgery several times and had cicatricial conjunctiva.
Discussion
Kaplan-Meier lifetable analyses showed that the success rate in the nonamniotic group was 74.8% from six months to one year after the surgery. The mean IOP was reduced significantly from 21.4 ± 6.5 mmHg to 12.1 ± 5.5 mmHg in the nonamnion group (P < 0.001). These findings are in good agreement with those of Hara and ShiratoCitation13 who reported that an IOP under 21 mmHg was achieved in 53.4% without medication and in 60.2% with and without medication at 60 months following conventional bleb revision surgery. Anand and AroraCitation14 reported that the probability of maintaining an IOP between 5 and 18 mmHg or a 20% decrease from the preoperative IOP was 64% at three years after conventional revision surgery. Earlier studies reported that the success rate of bleb revision was around 60% although there were some differences in the criteria for success. Thus, our results in the nonamnion group are in good agreement with these earlier findings.
While bleb revision with adjunctive MMC is an effective treatment in cases of bleb failure, glaucoma surgeons have been recently examining the effectiveness of amnion membrane transplantation. The amniotic membrane is made of strong and stable collagen, and has good anti-inflammatory, antifibrotic, and antiangiogenic properties. In glaucoma filtration surgery, the healing response is characterized by fibroblast outgrowth, and the fibrosis has been reported to be delayed more by an amniotic membrane than with conventional conjunctival closure.Citation5
For amniotic membrane transplantation, Fujishima et alCitation4 transplanted the amniotic membrane under a scleral flap and sutured it to the sclera. For the 14 eyes of the 13 patients with treatment-resistant glaucoma, the IOP was reduced to <20 mmHg after surgery in 13 eyes. Drolsum et alCitation6 used a large amniotic membrane, and sutured it to the scleral surface, and one end was positioned under the scleral flap and the other end was secured to subconjunctival tissue. The mean preoperative IOP was 32.2 mmHg, and the mean postoperative IOP was 16.4 mmHg. Although there were differences in the methods and definition of success, they reported that amniotic membrane transplantation was good for the revision of failed glaucoma filtering blebs.Citation4–Citation6
These reports encouraged us to try to use the amniotic membrane for bleb revision. One year after starting the use of amniotic membranes, we evaluated the efficacy of amniotic membrane transplantation to repair failed filtration blebs, and compared that with conventional bleb revision. Kaplan-Meier lifetable analyses showed that bleb revision with amniotic membrane transplantation was not better than conventional bleb revision with MMC in our cases. In fact, the postoperative IOP was significantly higher in the amnion-transplanted group than in the nonamnion-transplanted group. These results suggest that a subconjunctival placement of amniotic membrane does not improve the filtration in high-risk eyes. These poorer results using amniotic membranes for bleb revision discouraged us from recruiting new patients. So the number of the amnion group is smaller than the nonamnion group.
In the amnion group, six cases (50%) were fornix-based, and all of the cases in the nonamnion group were limbus-based because a fornix-based conjunctival flap allowed us to fix the amniotic membrane at the edge easier than a limbus-based flap. Earlier studiesCitation15,Citation16 reported that a fornix-based conjunctival flap and a limbus-based flap did not significantly alter the IOP-lowering effect of trabeculectomy. In our small amnion group, the success rates in the limbus-based group and fornix-based group were not significantly different. The IOP control results seemed to be unrelated to the surgical technique of handling the conjunctiva.
There are others who are more uncertain about the usefulness of amniotic membranes. Budenz et alCitation17 stated that amniotic membrane transplantation did not offer an effective alternative to conjunctival advancement for repair of a leaking filtering bleb. The postoperative IOP in their amniotic membrane transplantation group was relatively higher than in the conjunctival advancement group, although the difference was not statistically significant. Demir et alCitation18 concluded that amniotic membrane transplantation can depress wound healing in a rabbit model of glaucoma. However, the amniotic membrane was less effective than MMC.
Li et alCitation19 described the usefulness of amniotic membrane transplantation for the repair of conjunctival buttonholes during trabeculectomy with MMC. They also discussed better ways to use amniotic membrane use during glaucoma surgery. They concluded that amniotic membrane transplantation was useful when used as a platform for re-epithelialization as opposed to tissue replacement for conjunctiva after bleb excision. They reported on the importance of the way the amniotic membrane was handled to obtain good surgical results. Recently, Sheha et alCitation7 reported that amniotic transplantation in trabeculectomy with MMC for refractory glaucoma had achieved better IOP reduction than trabeculectomy with MMC alone. Although we sutured the amniotic membrane over the scleral flap, they placed a single layer of amniotic membrane under and around the scleral flap. All of these findings indicate that improvements in the surgical procedures for handling and placing the amniotic membrane are needed. For example, if the amniotic membrane is placed beneath the scleral flap, our outcome might have been improved.
Amniotic membranes have antifibrotic effects. However, the antifibrotic effects are not as potent as that of MMC.Citation18 The ability of amniotic membrane transplantation to suppress the fibroblast proliferation of the conjunctiva in eyes with refractory glaucoma may not be strong enough to maintain a functional bleb. This can be another reason for the mixed results of amniotic membrane transplantation in glaucoma-filtering surgery. To use the amniotic membrane for bleb revision before the bleb becomes severely scarred may be one of the methods that might improve the surgical results.
There were no severe complications such as hypotonic maculopathy, late bleb leaks, and bleb-associated infection in our cases. Other reports of amniotic membrane transplantation have also reported no damaging complications.Citation9–Citation11
Conclusion
The revision of a failed filtering bleb with adjunctive MMC is an effective way of lowering IOP. The use of amniotic membrane transplantation did not enhance the surgical outcome in our cases. Establishing better ways to handle amniotic membrane may also be a key factor in improving surgical results.
Acknowledgements
We thank Dr Duco Hamasaki for editing this manuscript.
Disclosure
The authors have no financial or proprietary interest in any material or method mentioned in this study.
References
- CairnsJETrabeculectomy. Preliminary report of a new methodAm J Ophthalmol1968666736794891876
- SturmerJBroadwayDCHitchingsRAYoung patient trabeculectomy. Assessment of risk factors for failureOphthalmology19931009289398510908
- AnandNAroraSSurgical revision of failed filtration surgery with mitomycin C augmentationJ Glaucoma20071645646117700288
- FujishimaHShimazakiJShinozakiNTrabeculectomy with the use of amniotic membrane for uncontrollable glaucomaOphthalmic Surg Lasers1998294284319599369
- BartonKBudenzDLKhawPTGlaucoma filtration surgery using amniotic membrane transplantationInvest Ophthalmol Vis Sci2001421762176811431440
- DrolsumLWillochCNicolaissenBUse of amniotic membrane as an adjuvant in refractory glaucomaActa Ophthalmol Scand20068478678917083539
- ShehaHKheirkhahATahaHAmniotic membrane transplantation in trabeculectomy with mitomycin C for refractory glaucomaJ Glaucoma20081730330718552616
- TsengSCLiDQMaXSuppression of transforming growth factor-beta isoforms, TGF-beta receptor type II, and myofibroblast differentiation in cultured human corneal and limbal fibroblasts by amniotic membrane matrixJ Cell Physiol199917932533510228951
- DuaHSGomesJAKingAJThe amniotic membrane in ophthalmologySurv Ophthalmol200449517714711440
- PrabhasawatPBartonKBurkettGComparison of conjunctival autografts and amniotic membrane grafts for pterygium excisionOphthalmology19971049749859186439
- ChenHJPiresRTTsengSCAmniotic membrane transplantation for severe neurotrophic corneal ulcersBr J Ophthalmol20008482683310906085
- Nagai-KusuharaANakamuraMFujiokaMLong-term results of amniotic membrane transplantation-assisted bleb revision for leaking blebsGraefe Arch Clin Exp Ophthalmol2008246567571
- HaraTShiratoSSurgical revision of failed filtering bleb with mitomycin CNippon Ganka Gakkai Zasshi19971015165199209140
- AnandNAroraSSurgical revision of failed filtration surgery with mitomycin C augmentationJ Glaucoma20071645646117700288
- GrehnFMautheSPfeifferNLimbus-based versus fornix-based conjunctival flap in filtering surgery. A randomized prospective studyInt Ophthalmol1989131391432744943
- el SayyadFel-RashoodAHelalMFornix-based versus limbal-based conjunctival flaps in initial trabeculectomy with postoperative 5-fluorouracil: Four-year follow-up findingsJ Glaucoma1999812412810209729
- BudenzDLBartonKTsengSCAmniotic membrane transplantation for repair of leaking glaucoma filtering blebsAm J Ophthalmol200013058058811078836
- DemirTTurgutBAkyolNEffects of amniotic membrane transplantation and mitomycin C on wound healing in experimental glaucoma surgeryOphthalmologica200221643844212566889
- LiGO’HearnTYiuSAmniotic membrane transplantation for intraoperative conjunctival repair during trabeculectomy with mitomycin CJ Glaucoma20071652152617873712