Abstract
Background
We aimed to compare visual and refractive outcome following phacoemulsification and intraocular lens implant (IOL) and combined one-site phacotrabeculectomy.
Method
We performed a retrospective study of case records of patients who had temporal incision phacoemulsification with IOL or one-site phacotrabeculectomy, between June 1997 and June 2001. The patients were matched for age group, operating list and IOL type. All patients were operated on under local anesthesia by the same surgeon. Each arm of the study had 90 patients, age range 60 to 75 years. We collected pre- and postoperative visual acuity, pre- and postoperative refraction within six months after surgery, and intended refraction. The intraocular pressure control was not recorded, as it was not the aim of our study.
Results
In the phacotrabeculectomy group, 76.6% of patients achieved aimed spherical equivalent, 15.5% of patients had against-the-rule (ATR) astigmatism induced by the surgery, and 90% of the patients had best corrected visual acuity (BCVA) more than 6/12. In the temporal incision phacoemulsification group, 81.1% of patients achieved aimed spherical equivalent, 10% of the patients had induced ATR by the surgery and 95.55% of patients achieved BCVA more than 6/12.
Conclusion
In this study the visual outcome of the phacotrabeculectomy group did not differ significantly from the visual outcome of temporal approach phacoemulsification.
Background
Combined cataract extraction with intraocular lens (IOL) implantation and trabeculectomy is a management strategy for patients with co-existing cataract and glaucoma. Advantages of the combined procedure include:
Enhanced postoperative visual recovery (unpublished data)
Reduction of the morbidity of two successive operations (CitationEdwards 1980; CitationMurchison and Shields 1990; CitationAllan and Barrett 1993)
Reduction of cost (CitationMcCartney et al 1988)
Prevention of the postoperative intraocular pressure (IOP) spikes that often occur in glaucoma patients after a cataract surgery (CitationKrupin et al 1989; CitationZetterstrom and Eriksson 1994)
Decreased risk of bleb fibrosis and dysfunction with subsequent cataract surgery (CitationMcCartney et al 1988)
Cataract surgery is increasingly thought of as a refractive procedure, and emmetropia can be achieved with accurate choice of the IOL power and by ensuring minimal postoperative astigmatism (CitationNordon and Lusby 1995).
In this study, the refractive results of one-site trabeculectomy and cataract surgery were compared with refractive results of temporal incision cataract surgery alone. The IOP control was not analyzed here since this has been done in a previous study by the same author (PSP) (CitationJayamanne et al 1997).
Patients and method
This was a retrospective study of the case records of patients undergoing one-site phacotrabeculectomy in one group and temporal incision phacoemulsification in the second group. In order to reduce variables in the study groups, the patients were matched for their age (range 60–75 years), same operating lists and IOL type (Corneal Quattro®). All surgeries were performed by a single surgeon (PSP), between June 1997 and August 2001, on an outpatient basis. The patients were operated either under peribulbar or topical anesthesia. We collected pre- and postoperative visual acuities, pre- and postoperative refraction within 6 months of the surgery, intended refraction and complications.
Ethical committee approval was obtained to contact the patient’s optometrist where hospital records were incomplete. As this was a retrospective study, corneal topography was not performed and the astigmatic progression/decay over time was not analyzed.
All patients were operated under local anesthesia by a single surgeon (PSP). The following technique was utilized for the one-site phacotrabeculectomy:
A fornix-based conjunctival flap was lifted and the sclera was treated with light surface cautery.
A straight 2 mm partial depth incision 2 mm posterior to the limbus was made with a 15° blade.
A scleral tunnel was created with a diamond keratome and a paracentesis was made into the clear cornea with a 15° blade.
The diamond keratome was used to enter the anterior chamber at the corneal side of the scleral tunnel through which the phacoemulsification procedure was performed (CitationJayamanne et al 1997). The tunnel length for the scleral incision was 3.00 mm.
Following implantation of the foldable IOL, a 1.5 mm × 4.00 mm deep block of corneal tissue was excised. Peripheral iridectomy was performed. Thorough evacuation of viscoelastic was ensured and acetylcholine added.
The enlarged external scleral incision was secured with 10-0 nylon figure of eight suture.
The conjunctiva was reapposed at the limbus using a 10-0 nylon suture. Balanced salt solution was injected via the paracentesis.
The followingprocedure was used for the temporal incision phacoemulsification:
A two-step clear corneal incision was made temporally with a 2.3 mm diamond keratome. The tunnel length was between 1.5–1.75 mm.
A side port incision was then made 2–3 clock hours to the left of the main incision. A continuous circular capsulotomy under viscoelastic (Healon GV) was followed by hydrodissection and bimanual phacoemulsification of the nucleus.
Once cortex aspiration was complete the corneal incision was enlarged to 3.2–3.5 mm and a foldable Corneal Quattro IOL was implanted in the capsular bag.
The viscoelastic was removed from the anterior chamber and from behind the IOL.
All patients received subconjunctival cefuroxime. Postoperatively, all patients received the same topical medication (guttae. prednisolone forte 1% tid) for three weeks.
Results
This was a retrospective study of two patient groups. Complete data was collected for 180 patients: 90 who had undergone phacotrabeculectomy, and 90 who had phacoemulsification alone. Demographics of the patients enrolled in the study are illustrated in .
Table 1 Patient demographics
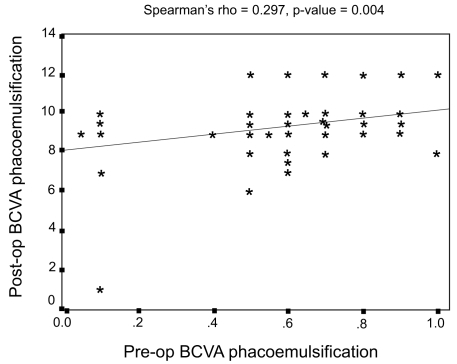
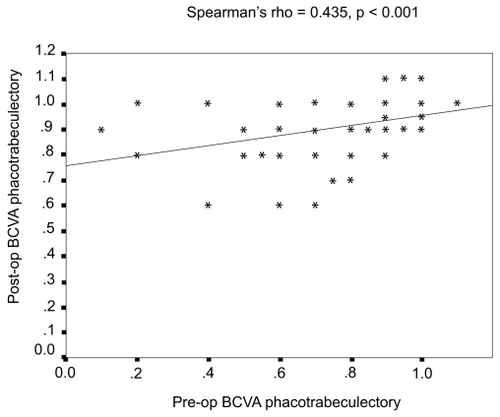
Best corrected visual acuity (BCVA) was recorded pre- and postoperatively in both groups. In the phacoemulsification group, 68 (75.5%) patients had preoperative BCVA of worse than 6/12. 86 (95.5%) of the patients in this group achieved postoperative BCVA of better than or equal to 6/12 (), of which 41 (45.5%) patients achieved 6/6 and 34 (37.7%) achieved 6/9.
In the phacotrabeculectomy group 81 (90%) of the patients achieved postoperative BCVA of better than or equal to 6/12 (35 patients achieved 6/6 and 31 patients achieved 6/9). However, in this group, only 28 (31.1%) patients had preoperative BCVA of < 6/12 (). The patients in the combined surgery group were chosen not primarily because of their poor visual acuity, but for their uncontrolled IOP.
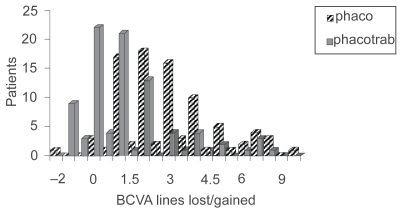
In the phacoemulsification group, only 4 patients had coexistent eye disease (1 patient had retinitis pigmentosa, 1 patient had glaucoma, and 2 patients had diabetic retinopathy). In the phacotrabeculectomy group, no patient had any other coexistent eye disease, apart from glaucoma and cataract. The postoperative complications are listed in . The BCVA lines lost/gained for each group are presented in .
Table 2 Postoperative complications
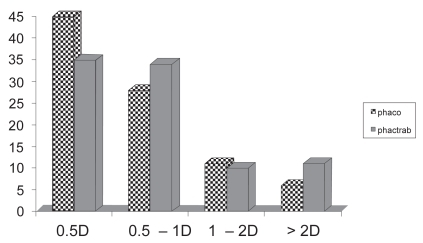
In the phacoemulsification group, 73 (81.1%) of the patients achieved their preoperative intended refraction, compared to 69 (76.6%) patients in the phacotrabeculectomy group. In both groups, the mean spherical equivalent achieved after surgery was within ± 1D of the mean spherical equivalent of the intended refraction ().
Table 3 Pre- and postoperative mean spherical equivalent in the study groups
In the visual outcome is presented as defocused equivalent (DE). This demonstrates that there is no statistical significant difference in the visual outcome between the 2 groups.
Table 4 Statistics for the visual outcome presented as DE: Independent samples test
The intended refraction was defined as the refraction intended to be achieved with the choice of IOL, according to biometry. In this study, it was considered that the intended refraction was achieved when the postoperative spherical equivalent was within ± 1D of the intended refraction. shows the breakdown of the results with the regards to the spherical equivalent.
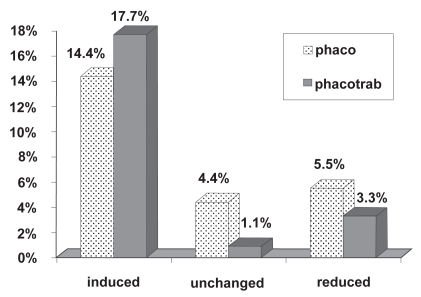
Preoperatively, 63 patients (70%) had astigmatism in the phacoemulsification group, compared with 62 patients (68.8%) in the phacotrabeculectomy group. Postoperatively, 69 patients (76.6%) had astigmatism in both groups. shows the percentage distribution of different types of astigmatism pre- and postoperatively in the phacoemulsification and phacotrabeculectomy groups respectively. We constructed a 95% confidence interval (CI) for the differences in binomial proportions based on inverting two 1-sided tests. This difference is not statistically significant (p > 0.05). The astigmatic changes following surgery were analyzed and are illustrated in and . As this study is retrospective, K readings were not available in all the patients included in the study. Therefore, for the astigmatic analysis, only the refraction results were used.
Table 5 Astigmatic results of the phacoemulsification group and phacotrabeculectomy group
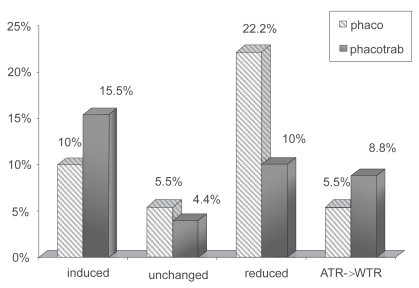
Analyzing the postoperative against-the-rule (ATR) astigmatism in the phacoemulsification group, 20 (22.2%) patients had reduced ATR, in 5 (5.5%) patients the ATR astigmatism remained unchanged, and in 5 (5.5%) patients the ATR astigmatism changed to with-the-rule (WTR) astigmatism.
The corresponding results for the phacotrabeculectomy group are as follows: 14 (15.5%) patients had surgically induced ATR astigmatism, in 4 (4.4%) patients ATR astigmatism remained unchanged, and in 9 (10%) patients the ATR astigmatism was reduced. In 3 (3.3%) patients ATR astigmatism changed to WTR astigmatism.
Discussion
Cataract surgery is increasingly considered a refractive procedure, as emmetropia can be achieved with accurate choice of IOL power and minimal postoperative astigmatism. Self-sealing incisions have a relaxing effect in the incision axis (CitationNielsen 1995). Therefore, it is recommended that in cases of WTR astigmatism, a superior incision should be performed, and in cases of ATR astigmatism, a temporal incision is preferred. However, because of the ATR drift of the superior incision, some authors (CitationFine and Hoffman 1996) perform a temporal incision whatever the preoperative astigmatism.
Cataract and glaucoma are two common conditions with an increasing prevalence with age, and it is not therefore unusual that they coexist in a number of patients. The surgical treatment of patients with cataract and glaucoma has changed considerably in the era of small incision cataract surgery. Additionally, patients’ expectations have increased, expecting both good visual recovery and long term intraocular pressure control.
Combined small incision cataract surgery and trabeculectomy has proved to be a suitable procedure in patients with medically uncontrolled glaucoma and cataract (CitationWedrich et al 1995; CitationWeitzman and Caprioli 1995). The combined procedure preserves the advantages of small incision phacoemulsification ie, low induced astigmatism, early refractive stabilization, and rapid visual rehabilitation. The likelihood of subsequent filtration failure may be reduced due to reduced tissue dissection, thus reducing the stimulus to wound healing (CitationAllan and Barrett 1993) or may be increased due to the increased inflammation of the dual procedure (CitationPark et al 1997).
Small incision, one-site versus two-site phacotrabeculectomy studies mainly compare IOP control (CitationJayamanne et al 1997; CitationPark et al 1997; CitationSayyad et al 1999). The results of IOP control following one-site phacotrabeculectomy have been reported in a different study by the same author (PSP) (CitationJayamanne et al 1997).
In previous studies comparing refractive results of combined procedures, the extra-capsular method was used for cataract extraction rather than phacoemulsification (CitationEdwards 1980; CitationMurchison and Shields 1990).
Few studies (CitationAllan and Barrett 1993; CitationWishart and Austin 1993; CitationVernon et al 1999) that analyzed the postoperative induced astigmatism in one-site phacotrabeculectomy compared with phacoemulsification alone did not find statistically significant difference between the two groups.
This study compares the refractive results of phacoemulsification and one-site phacotrabeculectomy, and shows that the difference in postoperative induced astigmatism, both overall and by sub groups in the two types of surgery, was not statistically significant (95% CI, p > 0.05). These results are similar with the published literature (CitationAllan and Barrett 1993; CitationWishart and Austin 1993; CitationVernon et al 1999).
A higher proportion of patients had postoperative WTR astigmatism in both groups (). This was mainly due to changes from ATR or oblique astigmatism. As previously reported, there could be various causes for WTR astigmatism following trabeculectomy. One study (CitationHugkulstone 1991) suggests the possibility of tight sutures and a posteriorly placed wound gape from the internal sclerostomy as the cause. In another study, CitationCunliffe and colleagues (1992) postulated that the internal sclerostomy allows the corneal edge of the trabeculectomy to sink slightly, thus decreasing the vertical radius of the cornea. Excessive cauterization has been suggested as a cause of increase in WTR astigmatism by CitationRosen and colleagues (1992). Wound-healing process was considered to be active in the process of inducing WTR astigmatism in a study conducted by CitationHong (1998).
Conclusion
Since this study was performed retrospectively, we recognized the following limitations:
Postoperative keratometry was not performed.
Astigmatic decay over time was not analyzed.
Preoperative and postoperative astigmatism indicates the manifest refraction, rather than K readings.
No vector analysis was undertaken for discussing changes in astigmatism.
Allowing for the above mentioned limitations of the study, we conclude that the results of this study indicate that the visual and refractive results of one-site phacotrabeculectomy compare favorably with temporal incision phacoemulsification.
Disclosure
SGF designed the study and advised on the writing up of manuscript; DV and KM collected the data and wrote the manuscript; PSP performed the surgery; AH performed the statistical analysis. All authors read and approved the final manuscript. The authors report no conflicts of interest.
References
- AllanBDBarrettGD1993Combined small incision phacoemulsification and trabeculectomyJ Cataract Refract Surg19197102
- CunliffeIADaplingRBWestJ1992A prospective study examining the changes in factors that affect visual acuity following trabeculectomyEye6618221289140
- EdwardsRS1980Trabeculectomy combined with cataract extraction: a follow-up studyBr J Ophthalmol6472047426599
- FineIHHoffmanRS1996Refractive aspects of cataract surgeryCurr Opin Ophthalmol721510160431
- HongYJChoeCMLeeYG1998The effect of Mitomycin C in postoperative corneal astigmatism in trabeculectomy and a triple procedureOphthalmic Surg Lasers2948499640570
- HugkulstoneCE1991Changes in keratometry following trabeculectomyBr J Ophthalmol7521782021587
- JayamanneDGRKostakisAPhelanPS1997The outcome of 2.3 mm incision combined phacoemulsification trabeculectomy and lens implantation of non-foldable intraocular lensesEye119149246284
- KrupinTFietlMEBishopKI1989Postoperative intraocular pressure rise in open-angle glaucoma patients after cataract or combined cataractfiltration surgeryOphthalmology96579842748112
- McCartneyDLMemmenJEStarkWJ1988The efficacy and safety of combined trabeculectomy, cataract extraction and intraocular lens implantationOphthalmology95754623211476
- MurchisonJFJrShieldsMB1990Limbal-based conjunctival flaps in combined extracapsular cataract surgery and glaucoma filtering procedureAm J Ophthalmol109709152346201
- NielsenPJ1995Prospective evaluation of surgically induced astigmatism and astigmatic keratotomy effects of various self sealing small incisionJ Cataract Refract Surg214387722901
- NordonLTLusbyFW1995Refractive aspects of cataract surgeryCurr Opin Ophthalmol63640
- ParkHJWeitzmanMCaprioliJ1997Temporal corneal phacoemulsification combined with superior trabeculectomyArch Ophthalmol115318239076202
- RosenWJMannisMJBrandtJD1992The effect of trabeculectomy on corneal topographyOphthalmic Surg2339581513535
- El SayyadFHelalMEl-MaghrabyA1999One site versus two site phacotrabeculectomy: a randomized studyJ Cataract Refract Surg2577829888081
- VernonSAZambarakjiHJPotgieterF1999Topographic and keratometric astigmatism up to 1 year following small flap trabeculectomy (microtrabeculectomy)Br J Ophthalmol837798210381662
- WedrichAMenapaceRRadaxU1995Long term results of combined trabeculectomy and small incision cataract surgeryJ Cataract Refract Surg2149547722902
- WeitzmanMCaprioliJ1995Temporal corneal phacoemulsification combined with separate incision superior trabeculectomyOphthalmic Surg2627137651702
- WishartPKAustinMW1993Combined cataract extraction and trabeculectomy: phacoemulsification compared with extracapsular techniqueOphthalmic Surg24814218115095
- ZetterstromCErikssonA1994Changes in intra-ocular pressure following phacoemulsification and implantation of posterior chamber lensEur J Implant Refract Surg6503