Abstract
We present a case of an 18 year old white male with Burkitt’s lymphoma who was operated on for hydrocephalus and subsequently referred for evaluation of new onset diplopia. On examination, his visual acuity (VA) was 20/20 in both eyes with a right superior oblique palsy. His pupillary reaction to light was intact while on near gaze there was no constriction of the pupils, bilaterally. The other two responses of the near gaze triad ie, convergence and accommodation were present. These findings were suggestive of an Inverse Argyll Robertson pupil (IARP), a rare entity in the literature. We could not find a specific cause attributable to this manifestation in this patient, though we feel it may be secondary to infiltration from Burkitt’s lymphoma and/or compression from elevated intracranial pressure of the efferent pupillary near reflex pathway.
Argyll Robertson Pupil syndrome is characterized by absence of pupillary light reflex with retention of pupillary constriction to near vision (CitationThompson 1987). It is described with neurosyphilis and peripheral neuropathies. There is also one case report of light-near dissociation associated with malignant lymphoma (CitationLapresle and Man 1979). Inverse Argyll Robertson Pupil (IARP), absence of pupillary constriction to near stimuli with retention of pupillary light reflex, has rarely been described. CitationChrousos and colleagues (1985) reported a child with absence of complete near reflex triad.
We are reporting a patient with no pupillary constriction on near gaze with presence of accommodation and convergence of near gaze triad and intact light reflex. This is the first reported case of IARP in a patient with Burkitt’s lymphoma.
Case report
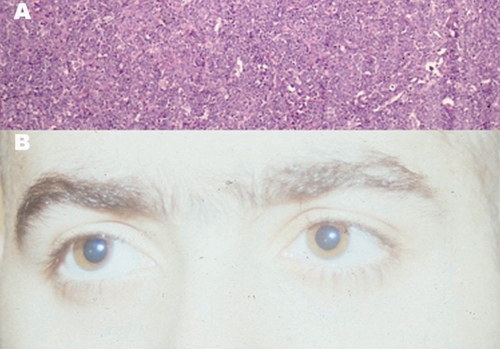
An 18-year-old Caucasian male was admitted for headache and abdominal pain, without diarrhea, of 3 weeks duration. Past medical history was unremarkable. An exploratory laparotomy with lymph node biopsy was performed. The diagnosis of Burkitt’s lymphoma, Stage D, noncleaved diffuse type was established (). Chemotherapy was initiated with cyclophosphamide, Oncovin®, methotrexate, and prednisone (COMP).
Figure 1 (A): Lymph node biopsy: Showing the typical ‘Starry sky appearance’ seen in Burkitt’s lymphoma. (B): Primary gaze: Showing right eye hypertropia. Size of the pupil 3 mm.
Computed tomography (CT) scans with and without contrast and magnetic resonance imaging (MRI) of the head was obtained secondary to the presence of headache in order to evaluate for central nervous system involvement. The studies demonstrated noncommunicating hydrocephalus without focal deficits or infiltrates. Spinal tap revealed an opening pressure of 41 cm H2O. Cerebrospinal fluid (CSF) analysis revealed normal protein and glucose levels with 220 WBC’s per high-powered field, which exhibited malignant morphologic characteristics. The CSF tested negative for cryptococcal antigen and Venereal Disease Research Laboratory (VDRL) test, with no growth on bacterial and fungal cultures. Subsequent bone marrow biopsy and HIV testing were also negative. Based on elevated opening pressure and the presence of hydrocephalus on neuro-imaging, the patient underwent ventricular-peritoneal shunting. Despite improvement in the hydrocephalus, ten days after the shunting procedure the patient developed diplopia for which the ophthalmology service was consulted.
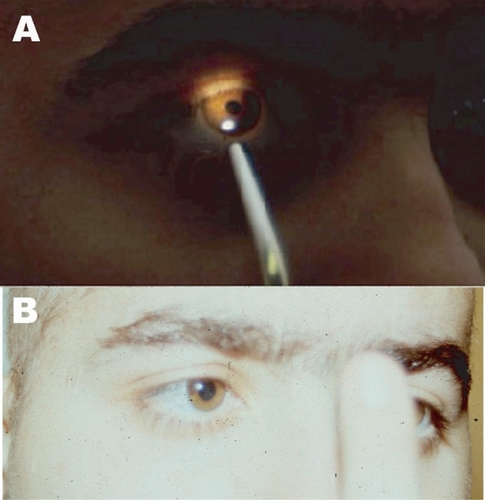
On examination visual acuity was 20/20 in both eyes at near. There was 6 diopters of accommodation by objective retinoscopy. Patient had hypertropia of the right eye (), maximal on left gaze with Beilschowsky test positive confirming right superior oblique palsy. Visual fields, color vision and optokinetic nystagmus were normal. Slit-lamp examination and fundoscopy were normal with no involvement of optic nerves. Pupils were 3 mm, equal, and reactive to light (). Near point of convergence was 8 cm. The pupillary response of the near reflex was absent (). This was tested several times with full patient cooperation. Base out prisms (used to induce convergence) failed to evoke pupillary constriction.
Figure 2 (A): Light reflex: Constriction of the pupil on projection of flash of light. (B): Near reflex: Convergence but no constriction of pupil on near reflex.
The patient was kept under observation. His general condition deteriorated and fourteen days later he developed a right 3rd cranial nerve palsy and expired two days later. An autopsy could not be performed for reasons beyond our control.
Discussion
The patient’s symptom of diplopia can be attributed to the palsy of the right superior oblique muscle. The long intracranial course of the trochlear nerve renders it vulnerable, which in this case was most likely affected by the elevated intracranial pressure. Incidently, the patient had no pupillary constriction on near gaze with preserved accommodation and convergence; the light reflex, however, was also maintained. These reflexes are mediated by the oculomotor nerve and associated parasympathetic fibers originating from the Edinger-Westphal nucleus (CitationBron et al 1997), however, the basis of this finding is difficult to explain. It has been suggested that neurons in the primate pretectal olivary nucleus are solely related to the pupillary light reflex and that the cortical projections to this pretectal nucleus are related to this reflex and do not play a role in the pupillary near response (CitationZhang et al 1996).
The differential diagnosis of this finding is difficult, as IARP itself is a rare clinical entity. CSF testing confirmed the absence of neurosyphilis and meningitis, leaving the presence of malignant-appearing white blood cells (WBCs) as the primary abnormality in addition to the elevated opening pressure. Thus, we propose that infiltration from the Burkitt’s lymphoma and/or increased intracranial pressure due to hydrocephalus may have caused compression over the anatomical pathway serving the efferents of the near pupillary reflex. The elevated intracranial pressure was most likely secondary to impaired CSF absorption at the arachnoid villi, which is most likely related to the presence of malignant WBCs in the CSF. An autopsy on this patient could have assisted in clarifying the pathology behind this manifestation.
References
- BronJTripathiRCTripathiBJ1997Wolf’s Anatomy of the Eye and Orbit8th edColumbiaLippincott Williams and Wilkins
- ChrousosGAO’NeillJFCoganDG1985Absence of the near reflex in a healthy adolescentJ Pediatr Ophthalmol Strabismus227673989645
- LapresleJManHX1979Argyll Robertson in a case of malignant lymphoma with ciliary involvementRev Neurol13551525531408
- ThompsonHSMosesRA1987The PupilAdler’s Physiology of the EyeSt. LouisThe CV Mosby Co31617
- ZhangHClarkeRJGamlinPD1996Behaviour of luminance neurons in the pretectal olivary nucleus during the pupillary near responseExp Brain Res112158628951418