Abstract
Purpose
To report a case of visually significant band keratopathy associated with ocular inflammation and systemic hypercalcemia which markedly decreased in severity after treatment of these underlying factors.
Methods
Retrospective case report.
Results
A 53-year-old Asian female with granulomatous panuveitis in the left eye presented with diffuse band keratopathy through the central cornea. The serum calcium was elevated. The patient was treated with topical prednisolone acetate 1% and oral prednisone with marked improvement in inflammation. The band keratopathy lessened in severity with clearing of the central cornea and improvement in visual acuity.
Conclusions
Early medical treatment of underlying factors may allow reversal of band keratopathy.
Introduction
The term band keratopathy describes the precipitation of calcium salts in Bowman’s layer in a band-like distribution across the central cornea. There are several local and systemic causes of band keratopathy, the most common ocular condition being intraocular inflammation and the most common systemic condition being hypercalcemia (CitationNajjar et al 2004) Treatment of symptomatic band keratopathy is typically surgical; treatment of the underlying cause can prevent further calcium deposition but does not usually reverse the corneal findings. We herein report a case of band keratopathy associated with ocular inflammation and systemic hypercalcemia, which markedly improved after treatment of the underlying factors.
Case report
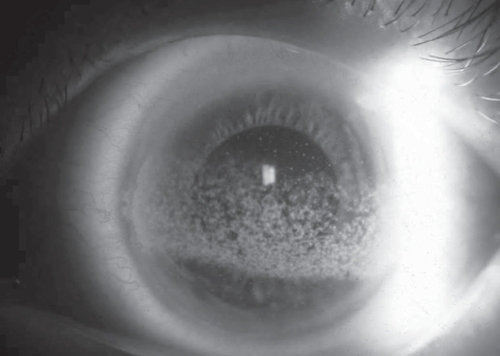
A 53-year-old Asian female presented with intermittent pain and decreased vision in the left eye. Her past ocular history was significant for retinal detachment repair in the right eye five months prior. Her left eye was noted to be normal at the time of surgery. She reported a slow visual decline in her left eye starting six weeks after the surgery on her right eye. Her past medical history was significant for chronic active interstitial pneumonitis diagnosed by lung biopsy four years prior, rheumatoid arthritis, hypothyroidism, and a recent diagnosis of hypercalcemia (12.7 mg/dL) believed to be secondary to excessive calcium intake. On presentation, visual acuity was 9/200 in the right eye and 20/100 in the left eye. Intraocular pressures were normal bilaterally. Slit-lamp examination revealed a cataract in the right eye without uveitis; the left eye had diffuse band keratopathy through the central cornea (), prominent mutton-fat keratic precipitates, 1+ anterior chamber cell, and 2+ vitritis. Dilated funduscopic examination revealed a cup-to-disc ratio of 0.3 in both eyes with peripapillary atrophy. A high scleral buckle was seen with a flat retina in the right eye. The view into the left eye was hazy due to band keratopathy and vitritis but the retina appeared flat with no areas of vasculitis or choroiditis. The patient was treated with hourly topical prednisolone acetate 1% with improvement in inflammation. A work up was obtained including a fluorescent treponemal antibody (FTA), rapid plasma regain (RPR), human leukocyte antigen B27 (HLAB27), and chest imaging but was unrevealing as to the etiology of the uveitis. The patient had also been previously evaluated for sarcoidosis due to pulmonary symptoms. A lung biopsy was consistent with chronic active interstitial pneumonitis; there was no evidence of sarcoidosis on biopsy.
The patient returned two months later and reported an improvement in visual acuity and resolution of ocular discomfort. Medications included prednisolone acetate 1% five times daily to the left eye and prednisone 10 mg per day, which had been initiated by the patient’s primary care physician 2 weeks prior due to shortness of breath. The serum calcium was 11.8 mg/dL. Visual acuity was 7/200 in the right eye and 20/35 in the left eye. Slit lamp examination was significant for new mild, peripheral band keratopathy in the right eye and improving band keratopathy in the left eye. There was trace anterior chamber inflammation in the right eye and 1+ vitritis in the left eye. Dilated funduscopic examination of the left eye revealed inactive-appearing chorioretinal lesions along the superotemporal and inferotemporal arcades. Topical prednisolone acetate 1% was slowly tapered in the left eye; no local therapy was instituted in the right eye as the patient was asymptomatic and vision was stable.
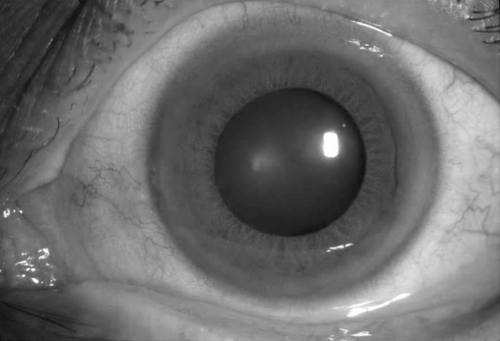
The patient returned two months and reported further improvement in vision in the left eye. Medications included prednisolone acetate 1% once daily in the left eye and prednisone 10 mg daily. The serum calcium was normal. Visual acuity was 7/200 in the right eye and 20/25 in the left eye. Slit lamp examination was significant for stable band keratopathy in the right eye and a marked improvement in band keratopathy () in the left eye. No ocular inflammation was noted in either eye.
Discussion
We herein describe a case of transient band keratopathy associated with ocular inflammation and mild systemic hypercalcemia. Although it is unclear which of the two factors was responsible for the band formation, we postulate that the ocular inflammation played a more dominant role as the uveitis was more severe and the systemic hypercalcemia was relatively mild. In addition, the time course of the band development closely mirrored that of the ocular inflammation. Specifically, band keratopathy was noted in the right eye in the setting of ocular inflammation and normalizing calcium levels. Clearing of the left central cornea occurred 4 months after treatment of ocular inflammation and normalization of serum calcium.
Transient band keratopathy has been described in patients with systemic hypercalcemia due to renal failure (CitationFeist et al 1992), sarcoidosis (CitationJohnston et al 1995), and pituitary adenoma (CitationAlonso Santiago and Ramirez Fe 2002) In the first two cases, the serum calcium level was higher than that found in our patient (18 mg/dL and 14.2 mg/dL, respectively). A mild anterior uveitis was noted in the patient with transient band keratopathy associated with sarcoidosis. The calcium level in the patient with a pituitary adenoma (CitationAlonso Santiago and Ramirez Fe 2002) was similar to that of our patient (12.2 mg/dl).
In summary, we present a case of transient band keratopathy associated with moderate ocular inflammation and mild hypercalcemia. This case suggests that early and aggressive treatment of the inflammation may result in reversal of band keratopathy. Chelation of band keratopathy should be deferred until an adequate course of anti-inflammatory therapy has been undertaken.
Disclosure
The authors have no conflicts of interest.
References
- Alonso SantiagoMARamirez FeC2002[Transient band keratopathy associated with hypercalcemia]Arch Soc Esp Oftalmol772111411973663
- FeistRMTesslerHChandlerJW1992Transient calcific band-shaped keratopathy associated with increased serum calciumAm J Ophthalmol113459611558127
- JohnstonRLStanfordMRVermaS1995Resolution of calcific band keratopathy after lowering elevated serum calcium in a patient with sarcoidosisBr J Ophthalmol791050
- NajjarDMCohenEJRapuanoCJ2004EDTA chelation for calcific band keratopathy: results and long-term follow-upAm J Ophthalmol13710566415183790