Abstract
Purpose:
To report a severe ocular complication initiated ten days after intravitreal administration of bevacizumab (Avastin®), in a patient with exudative age-related macular degeneration (AMD).
Patients and method:
Case report.
Results:
Ten days after intravitreal injection of 1.25 mg Avastin®, the patient manifested acute loss of vision with excruciating pain. An extensive choroidal detachment was evident in close contact with the lens, which necessitated an emergency sclerotomy with reconstruction of the anterior chamber. Four months later, the eye proceeded to phthisis bulbi. Five months after the injection, the patient complained of mild pain, photophobia, and visual acuity deterioration from the fellow eye. The diagnosis of sympathetic ophthalmia was suggested and treated with intravitreal injections of triamcinolone acetonide every three months with good response, complicated by elevation of intraocular pressure which we managed with Ahmet valve implantation.
Conclusion:
Serious ocular complications after intravitreal of Avastin® can not be excluded, including massive choroidal hemorrhage and sympathetic ophthalmia of the fellow eye.
Introduction
Intravitreal administration of bevacizumab (Avastin®; Genentech, Inc., San Francisco, CA), a humanized monoclonal antibody to vascular endothelial growth factor (VEGF), has been reported to help in age-related macular degeneration (AMD)Citation1–Citation3 and in regression of retinal and iris neovascularization.Citation4,Citation5
Case report
A 75-year-old male without history of ocular surgical intervention had an intravitreal injection of 1.25 mg bevacizumab (Avastin®) in the right eye (RE) because of exudative age-related macular degeneration. The patient had mild hypertension and was on metoprolol 50 mg tablets (Lopressor ®) bid. The patient did not have bleeding tendency, history of liver disease, and was not on anticoagulants.
Ten days after intravitreal injection, he manifested acute loss of vision with excruciating pain in the RE and he was admitted to our hospital. On presentation, his best-corrected visual acuity was no light perception (NLP) in the RE and 3/10 from the left eye (LE). The patient had an unbearable continuous excruciated pain in his RE. The conjunctiva was congestive, the cornea edematous, and the anterior chamber (AC) was collapsed (). An extensive choroidal detachment was evident in close contact with the lens (, ).The intraocular pressure in the patient’s RE was 55 mmHg, while he was on oral carbonic anhydrease inhibitor, drops of Xalatan® once daily (latanoprost), and Cosopt® bid (fixed combination of dorsolamide hydrochloride and timolol maleate). The intraocular pressure of the patient’s LE was 14 mmHg. The fundus examination of the LE revealed extensive confluent soft drusen at the posterior pole.
Figure 1 A) Right eye on presentation. The conjunctiva was congestive, the cornea edematous, and the anterior chamber collapsed. B) Extensive choroidal detachment was evident in close contact with the lens. C) Extensive choroidal detachment revealed by a B-scan image. D) B-scan image two months later. E) Four months later, right eye phthisis bulbi.
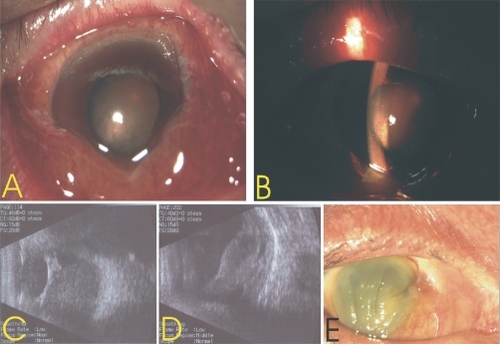
The intravenous administration of carbonic anhydrease inhibitor and hyperosmotic agent failed to reduce the intra-ocular pressure and to alleviate the pain. An emergency sclerotomy with reconstruction of the AC with viscoelastic was performed two days later. Two months later, the eye was painless, hypotonous, and there was detachment, residual subretinal fibrosis, and hemorrhage (). Four months later, the RE proceeded to phthisis bulbi ().
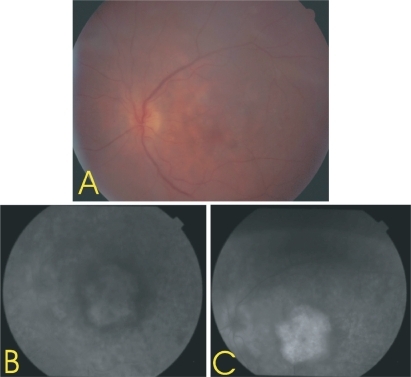
Five months after the injection, the patient complained of mild pain, photophobia, and visual acuity deterioration in his fellow eye. On presentation his best-corrected visual acuity in the LE was 1/20, and the fundus examination revealed extensive confluent drusen at the posterior pole with edema of the optic disc and flare and cells in the vireous. A fundus photograph () and fluorescein angiography were inconclusive due to dense cataract (, ). The diagnosis of sympathetic ophthalmia was suggested. Since the patient had a subtotal gastrectomy for uncontrollable bleeding from peptic ulcer 15 years ago, activated by an excessive salicylates intake, we opted for only topical and parabulbar steroids. Ten days later, the patient experienced significant visual improvement. Three months later, his best-corrected visual acuity in the left eye was 2/10 while he still was under treatment.
Figure 2 Dense cataract obscures details. A) Color fundus photograph of the left eye five months after the intavitreal injection of Avastin® in the right eye. B, C) Fluorescein angiography five months after the intavitreal injection of Avastin® in the right eye.
Finally the patient overcame his fears and let us to proceed with intravitreal injections of triamcinolone acetonide every three months with a good responseCitation6,Citation7 complicated by an elevation of intraocular pressure, which we managed with an Ahmet valve implantation. Now, 11 months later, his best corrected vision is 1/10.
Discussion
Systemic administration of bevacizumab causes serious and, in some cases, fatal adverse reactions. Hemoptysis has occurred in patients with non-small cell lung cancer treated with chemotherapy combined with Avastin®.Citation8 In a small study, the incidence of serious or fatal hemoptysis was 31% in patients with squamous histology and 4% in patients with adenocarcinoma receiving Avastin® compared to cases treated with chemotherapy alone. It is advised that patients with a history of recent hemoptysis should not receive Avastin®.Citation8
When data were pooled from two randomized phase II studies utilizing bevacizumab with 5-FU/leucovorin, and also in a third treatment arm of bevacizumab/5-FU/LV of a randomized phase III study, a few toxicities were uniformly encountered in all of the above studies.Citation9 The reported toxicities were grade 3 (medically manageable) hypertension (3%–16%), hemorrhage (2%–9.3%), gastrointestinal perforation (1.5%), arterial thromboembolism (3.8%), wound-healing problems (1%–2%), and proteinuria (1%–2%).Citation9
The reported ocular complications of intravitreal injection for ARMD so far, are tears of retinal pigment epitheliumCitation10–Citation13 and complications related to the injection site mainly, as conjunctival hyperemia and subconjunctival hemorrhage.Citation14
Our case demonstrates a serious ocular complication initiated ten days after intravitreal administration of Avastin® in a patient with exudative AMD.
Disclosure
The authors report no conflicts of interest in this work.
References
- RosenfeldPJMoshfeghiAAPuliafitoCAOptical coherence tomography findings after intravitreal injection of bevacizumab (Avastin) for neovascular age-related macular degenerationOphthalmic Surg Lasers Imaging20053633133516156152
- AveryRLPieramiciDRabenaMIntravitreal bevacizumab (Avastin) for neovascular age-related macular degenerationOphthalmology200611336337216458968
- SpaideRLaudKFineHTreatment of chroidal neovascularization secondary to age-related macular degenerationRetina20062638339016603955
- AveryRRegression of retinal and iris neovascularization after intravitreal bevacizumab (Avastin) treatmentRetina20062635235316508438
- DavidorfFMouserGDerickRRapid improvement of rubeosis iridis from a single Bevacizumab (Avastin) injectionRetina20062635435616508439
- OzdemirHKaracorluMKaracorluSIntravitreal triamcinolone acetonide for treatment of sympathetic ophthalmiaGraefes Arch Clin Exp Ophthalmol200524373473615756580
- JonasJBSpandauUHRepeated Intravitreal triamcinolone acetonide for chronic sympathetic ophthalmiaActa Ophthalmol Scand20068443616704716
- JohnsonDHFehrenbacherLNovotnyWFRandomized phase II trial comparing bevacizumab plus carboplatin and paclitaxel with carboplatin and paclitaxel alone in previously untreated locally advanced or metastatic non-small-cell lung cancerJ Clin Oncol2004222184219115169807
- SaifMWMehraRIncidence and management of bevacizumab-related toxicities in colorectal cancerExpert Opin Drug Saf2006555356616774493
- NicolòMGhiglioneDCalabriaGRetinal pigment epithelial tear following intravitreal injection of bevacizumab (Avastin)Eur J Ophthalmol20061677077317061236
- ShahCPHsuJGargSJFischerDHKaiserRRetinal pigment epithelial tear after intravitreal bevacizumab injectionAm J Ophthalmol20061421070107217157598
- KookDWolfANeubauerASRetinal pigment epithelial tears after intravitreal injection of bevacizumab for AMD. Frequency and progressOphthalmologie2008105158164
- GargSBrodRKimDLaneRGMaguireJFischerDRetinal pigment epithelial tears after intravitreal bevacizumab injection for exudative macular degenerationClin Experiment Ophthalmol20083625225618412594
- CostaRAJorgeRCalucciDCardilloJAMeloLAScottIUIntravitreal bevacizumab for shoroidal neovascularization caused by AMD (IBeNA Study): results of a phase 1 dose-escalation studyInvest Ophthalmol Vis Sci2006474569457817003454