Abstract
Objective:
To determine the prevalence of dry eye symptoms and signs in children with juvenile idiopathic arthritis (JIA).
Patients and methods:
A total of 192 children with JIA: 48 oligo-, 39 extended oligo-, 79 polyarthritis, and 26 with other types of arthritis (eight juvenile spondyloarthritis, five juvenile psoriatic arthritis, three mixed connective tissue diseases, two systemic onset arthritis, and eight undetermined arthritis) were interviewed for dry eye symptoms and tested with Schirmer test with anesthetic. Two thirds of the patients were female and the mean age of the patients was 13.1 years (range 10–16) and the mean duration of arthritis was six years (SD 4, 4). Thirty-one percent of the patients had a history of uveitis. Dry eye was defined as Schirmer test score ≤ 5 mm in five minutes. The type of arthritis, a history of uveitis, and the ocular and systemic medication used were evaluated for their correlation with dry eye symptoms and signs by using chi-square tests and the Mann–Whitney Monte Carlo analysis.
Results:
Altogether 17% of this cohort had decreased basal tear secretion. The most common symptoms of dry eye were discharge secretion, itching, and watering. The intensity of symptoms and signs did not correlate. The type of arthritis, a history or presence of uveitis, and the medication used did not correlate with the occurrence of dry eyes.
Conclusion:
Dry eye symptoms and signs are common in JIA, and Schirmer test with anesthetic is a useful tool in evaluating these patients.
Introduction
The most common extra-articular manifestation of juvenile idiopathic arthritis (JIA) is chronic insidious uveitis occurring in 20% of patients.Citation1 The widely known risk factors of uveitis are a young age at the onset of arthritis, oligoarthritis, and positive antinuclear antibodies (ANA).Citation2 Less known is the role of dry eye syndrome in JIA. Severe aqueous tear deficiency leading to keratoconjunctivitis sicca (KCS) is assumed to be rare in childhood. Sjögren’s syndrome (SS) with symptoms of dry eyes and dry mouth is seldom seen in children: the prevalence is assumed to be about 5% in juvenile rheumatic diseases.Citation3–Citation5
Because some of our JIA patients complained of discomfort in their eyes, we decided to screen for possible dry eye symptoms and signs by biomicroscopy, the Schirmer test with anesthetic, and by making a symptoms inquiry to a large clinic-based cohort of 192 consecutive JIA patients in their early teens.
Patients and methods
The study was conducted at The Rheumatism Foundation Hospital, Heinola, Finland, which is a tertiary center for rheumatic patients for the whole country and a secondary center for those living in the neighborhood.
All the JIA children, born in 1990–1995, whose diagnoses of JIA were made by a pediatric rheumatologist at this hospital and who were examined between September 2005 and December 2006, were included in this study. The diagnosis of arthritis was made according to International League of Associations for Rheumatology classification and the diagnosis of uveitis was made according to the International Uveitis Study Group guidelines.Citation6,Citation7 The patients were systematically and regularly (every 2 to 6 months) sent for an ophthalmologic evaluation for detection/exclusion of insidious uveitis, as recommended.Citation1,Citation2 The examination for dry eye symptoms and signs was performed once to every patient during these visits.
Every patient underwent a comprehensive ophthalmologic examination including the best corrected visual acuity, biomicroscopy, examination of the posterior parts of the eyes with a 90 diopter Volk lens, as well as an inspection of the outer parts of the eyes and eye lids. The corneal surface was examined in biomicroscopy by authors KK or KS-K with/without staining with fluorescein to look for the dry spots of the cornea, marginal tear meniscus, and stability of the tear film.
A registered nurse (PS) was responsible for the patient interview and the Schirmer test. A Schirmer test was performed after the biomicroscopy of the eyes. Five minutes after the instillation of anesthetic drops (Oftan ObucainR, Santen, Finland) in both eyes, 35-mm regular Schirmer test strips were placed in the outer third of the inferior fornix of both eyes while the patient was in a sitting position. The test was regarded as positive if the strips became moist ≤5 mm downwards from the eye lid margins in five minutes.
The patients were asked about their dry eye symptoms: itching, smarting, foreign body sensation, watering, discharge secretion, and redness, which were graded 0–3, maximum 18; 0 no symptoms, 1 mild, 2 moderate, 3 severe symptoms.
A re-inquiry of symptoms and signs was made to 158 patients in connection with their subsequent visits 6 to 18 months later.
Statistics
Statistical significance between groups was evaluated by Mann–Whitney test (Monte Carlo p-value), chi-square test or Fisher–Freeman–Halton test.
Ethics
The study protocol was approved by the local Institutional Ethics Committee.
Results
The demographic data of the patients are described in Table . The group of “other arthritis” consisted of eight patients with juvenile spondyloarthritis, five with juvenile psoriatic arthritis, three with mixed connective tissue disease, two with systemic onset arthritis, and eight with undetermined arthritis. Most of the patients, 91% (174/192), had active arthritis at the time of the study. The mean age of the patients at the onset of JIA was 7.1 years (range 1–15) and at the time of the study 13.1 years (range 10–16) after the mean follow-up time of six years (SD 4.4).
Table 1 Demographic data of 192 patients with juvenile idiopathic arthritis (JIA)
Chronic uveitis had been a feature of the disease in 61 cases (31%). Most of these, 44 (72%), had ongoing topical corticosteroid treatment (dexamethasone or prednisolone acetate) for uveitis and 13 had undergone cataract or glaucoma surgery.
A total of 17% (32/192) of the patients had decreased basal tear secretion (Schirmer value ≤5 mm in five minutes after anesthetic drops) in both eyes and their mean symptom score was 5.3 (range 0–11).
Twenty percent of the patients with a history of uveitis and 15% of those without had Schirmer test result ≤5 mm in both eyes (p = 0.45) and the mean score of symptoms 6.1 (range 1–11) and 4.9 (range 0–11), respectively. These patients did not significantly differ from each other with regard to the dry eye symptoms or signs (p = 0.62). The mean Schirmer values according to the eye with a smaller tear secretion were 11.0 (range 0–29, SD 8.6) in patients with a history of uveitis and 13.0 (range 0–35, SD 10) in patients without uveitis.
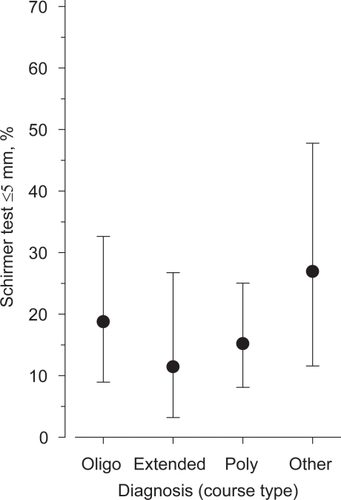
As many as 35% (67/192) of the whole study group had the Schirmer test value ≤10 mm in five minutes in both eyes and the mean symptom score of 5.3 (range 0–14). The Schirmer test results in the four patient groups did not markedly (p = 0.34) differ from each other as seen in Figure .
Figure 1 The occurrence of low Schirmer test values ≤5 mm in both eyes in the four different diagnostic groups of 192 juvenile idiopathic arthritis patients.
The medical therapy was not associated with decreased tear secretion. Fifty-seven (93%) of the 61 patients with a history of uveitis and 116 (89%) of those without uveitis used disease-modifying antirheumatic drugs (DMARDs) at the time of the study (Table ). Methotrexate was used as often in patients with low Schirmer test values as in those with normal results. Biologic agents were similarly used in both groups and so was systemic glucocorticoid treatment.
Table 2 Treatment of 192 juvenile idiopathic arthritis patients at the time of ophthalmic screening. A combination of drugs was frequently used
Altogether 94% of the patients reported one or more of the dry eye symptoms. The occurrence of eye symptoms in patients with decreased tear secretion as compared to those with normal tear secretion is described in Table . The 32 patients with low Schirmer test values (≤5 mm) in both eyes had the mean intensity of symptoms at 5.3 (range 0–11) compared to the value of 5.2 (range 0–16) in the 160 with the Schirmer test value >5 mm (ns).
Table 3 The occurrence of eye symptoms in 192 juvenile idiopathic arthritis patients with positive and negative Schirmer test values in both eyes
Most of the patients in our study had normal tear film stability when evaluated by biomicroscopy between blinks. None of the patients had filaments on the cornea, although in some cases a few dry spots were seen in the lower corneal epithelium after staining with fluorescein.
Discussion
A total of 17% of the patients had the Schirmer test value ≤5 mm and 35% had ≤10 mm in both eyes. The number of patients with low basal tear secretion was somewhat higher among children with uveitis than among those without a history of uveitis (20% vs. 15%) but the difference was not significant. The course type of arthritis or the medication used had no impact on dry eyes.
In adult-onset SS dryness of the eyes occurs in up to 90% of patients.Citation3,Citation4,Citation10 This disease is rare in childhood, which may explain the fact that there are few papers concerning the dry eye problem in JIA.Citation8 In our earlier epidemiologic study of young adults with JIA, 40% of the patients with uveitis and 26% (ns) of those without had dry eye symptoms and the Schirmer test with anesthetic ≤10 mm/5 min in either eye.Citation11 In the present study no great difference was found in the Schirmer test with cut-off value ≤10 mm/5 min (41% vs. 35%, respectively) between patients with or without a history of uveitis. Perhaps the longer duration of uveitis and arthritis in the former study explains it.
According to a report from India, 12% of 50 JIA children had KCS.Citation9 Their patient cohort was different from the one in the present study, as most of the patients were male, had polyarthritis and a fifth of the cohort had systemic-onset arthritis. Children with corticosteroid treatment or topical treatment for uveitis were excluded. Their cut-off value in the Schirmer test was ≤10 mm in five minutes. A study from Turkey describes the occurrence of KCS in 64 JIA patients and controls.Citation10 Dry eye symptoms and signs with the cut-off value ≤5 mm were found in 12.5% and 10.9% of the patients, respectively, compared to 1.5% and 1.5% of the controls. Also, in that study patients with systemic glucocorticoid treatment, topical ocular treatment and previous ocular laser or surgical treatment were excluded.
In the present study, we included all the 192 consecutive JIA patients born in 1990–1995 who visited both a pediatric rheumatologist and an ophthalmologist during the study period and who thus formed a cross-sectional age group. In our study, the mean duration of arthritis was six years, and the majority of the patients had ongoing medical treatment for arthritis. Chronic asymptomatic anterior uveitis was also a frequent feature of the disease in the study group (31%). Patients with JIA complain of aches or discomfort in their joints less often than adults. Perhaps that is the reason why they seldom spontaneously report any symptoms of dry eyes if not particularly asked about them. The lack of association between signs and symptoms of dry eyes in JIA children has earlier been reported by Nichols and colleauges.Citation12 Because the treatment was applied according to the intensity of symptoms of dryness only a small proportion of the patients needed artificial tears. A re-inquiry was made to 158 patients at their further control visits and 23% (36) of them had used artificial tears; 50% (18/36) of them had the Schirmer test result ≤5 mm/5 min in either eye, whereas 21% (26/122) of those who had not used artificial tears, had the same test result.
We describe here the practical screening of dry eyes by the Schirmer test with an anesthetic and by a symptoms inquiry as a part of clinical examination of JIA patients. In connection with the Schirmer test, patients were also instructed on of the use of the treatment modalities for dry eyes. More extensive tests may be needed only in cases with low Schirmer value combined with marked symptoms or signs of dry eyes. Rose Bengal dye is very irritating to dry eyes and we seldom use it nowadays. More extensive testing was also limited because of the young age of the patients.
Dry eye symptoms and signs are common in JIA. A symptoms inquiry and Schirmer test with anesthetic are useful tools for pediatric rheumatologists/rheumatologists in managing these patients.
Disclosure
The authors report no conflicts of interest in this work.
References
- KanskiJJUveitis in juvenile chronic arthritis: incidence, clinical features and prognosisEye198826416453256502
- KotaniemiKSavolainenAKarmaAAhoKMajor review. Recent advances in uveitis of juvenile idiopathic arthritisSurv Ophthalmol20034848950214499817
- PetroutsosGPaschidesCAKarakostasKXPsilasKDiagnostic tests for dry eye disease in normal and dry eye patients with and without Sjögren’s syndromeOphthalmic Res1992243263311287511
- ChudwinDSDanielsTEWaraDWSpectrum of Sjögren’s syndrome in childrenPediatrics198198213217
- PiperHDouglasKMJTreharneGjPrevalence and predictors of ocular manifestations of RA: is there a need for routine screening?Musculoskelet Care20075102117
- PettyRESouthwoodTRRevision of the proposed classification criteria for juvenile idiopathic arthritis: Durban 1997J Rheumatol199825199119949779856
- Bloch-MichelENussenblattRBInternational uveitis study group recommendations for the evaluation of intraocular inflammatory diseaseAm J Ophthalmol19831032342353812627
- JainVSinghSSharmaAKeratoconjunctivitis sicca is not uncommon in children with juvenile rheumatoid arthritisRheumatol Int20012015916211411961
- AkinciACakarNUncuNKeratoconjunctivitis sicca in juvenile rheumatoid arthritisCornea20072694194417721292
- ModyGMHillJCMeyersOLKeratoconjunctivitis sicca in rheumatoid arthritisClin Rheumatol198872372413262029
- KotaniemiKArkela-KautiainenMHaapasaariJLeirisalo-RepoMUveitis in young adults with juvenile idiopathic arthritis: a clinical evaluation of 123 patientsAnn Rheum Dis20056487187415897307
- NicholsKKNicholsJJMitchellGLThe lack of association between signs and symptoms in patients with dry eye diseaseCornea20042376277015502475