Abstract
This case report describes the effect of simultaneous pancreas kidney transplant (SPK) on the diabetic retinopathy (DR) of two male type 1 diabetic patients. The literature on the effect of SPK on DR is reviewed and the evidence surrounding visual function outcomes is discussed.
Introduction
Pancreas transplants were first used as a treatment for type 1 diabetes in 1966. The initial aim of the operation was to improve the quality of life of patients by removing the need for repeat blood sugar monitoring and insulin injection. Operative results have been successful producing, in those with functioning grafts, not only insulin-independence but also euglycemia with normal glycosylated hemoglobin (HbA1C), improvement of lipid profiles and normal hypoglycemia responses.Citation1 Besides these primary benefits, pancreas transplant has been shown to ameliorate the secondary complications of diabetes mellitus including nephropathy, neuropathy, and retinopathy.Citation1 The effect on retinopathy, however, is disputed.Citation2 Pancreas transplant alone (PTA), simultaneous pancreas kidney transplants (SPK), and pancreas transplant after kidney transplant are available options. The dogma is that transplants are beneficial for the treatment of retinopathy when carried out early. Two cases illustrating unexpected late recovery of visual acuity (VA) after SPK in advanced disease are presented and the literature on the effect of transplantation on diabetic retinopathy (DR) is reviewed.
Case reports
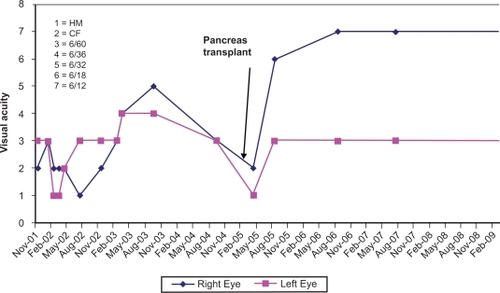
A 40-year-old asthmatic man with type 1 diabetes mellitus for fourteen years presented with subacute blurred vision of counting fingers (CF) in his right eye and 6/60 in his left. He had bilateral vitreous hemorrhages with florid proliferative diabetic retinopathy and angle neovascularization. Bilateral cryoretinopexy was followed by bilateral vitrectomies and endolaser to try and prevent blindness. Two months after treatment, his VA was CF in the right and hand movements (HM) on the left. Over the ensuing 18 months he required further sequential surgeries including bilateral cataract surgery, vitreous washout and supplemental indirect retinal laser, which stabilized the VA to 6/60 in both eyes (). Two years later he received a successful SPK. Bilateral Yag laser capsulotomies were undertaken three years later. The combination of capsulotomy and SPK resulted in stable DR with vision in his right eye recovering to 6/12 despite having being registered blind ().
Table 1 Table to show change in visual acuity over time with important clinical events noted
The second patient was first seen in 2002, aged 40 years with a 20-year history of type 1 diabetes mellitus presenting with bilateral proliferative retinopathy and macular edema. He had extensive laser treatment to both eyes. His diabetic control had always been poor as had his attendance at eye appointments. In 2003 a sudden drop in VA from 6/9 to 6/36 in his left eye prompted re-attendance. Bilateral cystoid edema was found and coincided with a diagnosis of systemic hypertension (systolic pressures in excess of 200 mmHg). He received grid and focal laser treatment and left intravitreal injection of Kenalog. VA improved to 6/18 in his left eye (LE). In 2004 and 2005 he underwent right and then left vitrectomy and delamination for severe proliferative retinopathy resulting in premacular hemorrhage in his right eye (RE) and left disc vessels and macular edema reducing vision to HM right and 6/60 left.
By March 2005, VA had improved to 6/9 RE and 6/18 LE. Six months later VA dropped to 6/60 LE due to chronic cystoid macular edema for which another intravitreal steroid injection was given. In March 2006 he underwent left cataract surgery with intraocular lens implantation yielding VA 6/9 RE and 6/24 LE. Hypertension remained a problem causing papilledema in December 2006. A SPK was done in January 2007 and review in February showed markedly improved disc appearances. By December 2007, VA was 6/9 RE and 6/12 LE with stable DR since the transplant with resolution of the macular edema. His quality of life was remarkably improved.
Both patients, as well as ophthalmology review, had been referred to the diabetic service due to poor diabetic control and raised HbA1c levels. The diabetes was managed, in both cases, with the expected combination of insulin plus best medical management with adjuncts such as antihypertensives.
Literature review
The beneficial effect of pancreas transplant on DR is debated with an increasing body of evidence supporting its efficacy. Improvements seem to be time dependent becoming significant after approximately three years.Citation2 In a comparison of successful and failed pancreas transplants at two years no significant difference was found in degree of retinopathy.Citation3 However after three years those with functioning grafts had no further progression of their retinopathy whilst 70% of those with failed transplants had higher grade disease by five years.Citation3 No difference was found in VA. In two other studies, stabilization of DR in a 25 SPK patient case seriesCitation4 and improvements in the microcirculation of the eyeCitation5 in SPK versus kidney transplant alone (KTA) occurred by three years. This is in comparison to our findings where stable improvement in the presented cases occurred after only two years and one year, respectively.
A shorter follow-up period does seem to be associated with a lack of positive findings in other studies, for example, one year after successful SPK versus KTA, despite a significant drop in HbA1C with SPK, there was no difference between grade of retinopathy in the two groups.Citation6 Immunosuppression therapy was the same and blood pressure fell similarly in both cases.Citation6 Another study showed no difference at two years in the stage of DR when comparing successful and unsuccessful pancreas transplant recipients,Citation7 but less deterioration was seen in the successful group after three years.Citation7 No change was seen in VA.Citation7 In comparison, one small study showed improvement in DR after only one year when comparing functioning and nonfunctioning pancreas transplants,Citation8 in agreement with the cases presented here but another study of SPK failed to show an effect despite long follow-up times.Citation9 The majority of patients in this latter study had severe proliferative DR pre-transplant, most receiving laser treatment.Citation9 Despite the lack of improvement, DR grade and VA were stabilized by SPK up to the end of the 10 year study.Citation9
The grade of disease pre-pancreas transplant may influence the response to transplant. In a comparison of diabetics with and without PTA a significant difference was found between the number of patients with stabilized or improved grade of diabetic retinopathy and macular edema except in grade 5 diabetic retinopathy.Citation10 14% of those with proliferative retinopathy pre-transplant had worsening disease despite successful graft with an average 30-month follow-up (none less than a year).Citation10 There was no significant improvement in VA, intraocular pressures or cataract incidence across all grades.Citation10 Another study of 30 SPK patients and 12 KTA patients also failed to show a difference in VA, and concluded that the disease at outset was too advanced to be amenable to benefit.Citation11 A rodent study, designed to examine the effect of DR grade pre-transplant using rats at different stages of DR, also supported this theory.Citation12 Sixty rats were split into four groups: healthy controls, untreated alloxan-induced diabetic, treated with pancreas transplant two weeks post-induction of diabetes, and treated with transplant 12 weeks post-induction. In comparison with diabetic controls, within one year early pancreas transplant (two weeks versus 12 weeks) significantly reduced cataract prevalence whilst later transplant did not. Microscopy also showed improved structure of the retina and its blood supply in the early transplant group in comparison with diabetic controls and late transplant rats. The late transplant group showed progression of retinopathy.Citation12 Contrarily, both cases presented here had high grade proliferative DR at presentation but showed marked improvement.
The microcirculation of the conjunctiva, when examined with intravital microscopy, has been shown to benefit from pancreas transplant.Citation13 Significant improvement in microangiopathic changes were seen in PTA and SPK when compared with type 1 diabetics with and without KTA. In fact normalization occurred at > 1 year post-SPK but the correlation with VA or disease stage was not studied.Citation13 The change was attributed to reversal of morphological adaptation to glycosylation including arteriole length per area and diameter.Citation13 Structural changes were related to improvement in function with vascular perfusion increasing in relation to length per area. Whether the conjunctival microcirculation can be used as a model for the retinal microcirculation is debatable. However the significant difference found at 18 months post-SPK was seen in none of the controls showing that immunosuppression and normalization of uremia may not factor in preventing microangiopathy progression post transplant.Citation13
A study comparing controls, type 1 diabetics, SPK and KTA patients measured oxygen pressure, re-oxygenation time and velocity of the microcirculation.Citation5 All three parameters showed significant improvement after the third year post-transplant with near normalization of re-oxygenation time. This result may indicate that nerve regeneration and repair is also occurring allowing improved relaxation of the smooth muscle in the vessel walls.Citation5 The study also showed that KTA did not influence DR confirming uremia is not of primary importance and also that the size of the improvement of the microcirculation was proportional to the initial readings, ie, that the less diseased the microcirculation was the larger the improvement it made after pancreas transplant.Citation5
Many variables change after pancreas transplant including euglycemia, physiological levels of insulin, improved lipid pro-files, blood pressure, and urea levels. No study showed that KTA was effective in reducing the grade of DR whereas PTA and SPK were both effective, despite a similar fall in blood pressure in all transplant patients and normalization of uremia in KTA. Therefore, although uremia and hypertension are known to exacerbate DR, correcting these factors alone in not enough to improve DR. Some evidence that good glucose control is key was provided by a large randomized prospective study of 1441 insulin-dependent diabetics studied over 6.5 years.Citation14 Half the patients had mild DR before the study and the other half no DR. Patients were randomly assigned to either intensive or normal insulin therapy.Citation14 A statistically significant affect on primary prevention and progression rate in the secondary prevention group was found consistently in all subgroups not affected by either sex, blood pressure, age, duration of insulin-dependent diabetes mellitus, weight, initial grade of DR, or HbA1C.Citation14 The group concluded that intensive insulin therapy, whether due to euglycemia or euinsulinemia, delays the onset and slows the progression of DR after three years and the difference continues to get more marked with time.Citation14
Visual acuity loss in DR can be caused by a range of processes currently recognized including macular ischemia, macular edema, epiretinal membrane formation, and vitreous hemorrhage. Before any retinopathy is apparent, however, using electrophysiological tests, the neuronal network has been found to be impaired.Citation15 Therefore the new paradigm in the pathophysiology of DR is considering the disease as a primary neuronal disease rather than one of the retinal microcirculation. It is postulated that the unique physiology of the retina makes the neural networks particularly prone to oxidative stress such as its high metabolic demands, use of glycolysis, sparse vascularity, and low oxygen tension.Citation15
When the VA fails to improve following treatment and angiography (indicating a compromised capillary circulation), the prognosis for vision is considered poor. Perhaps in young patients, like those in the present series, the photoreceptor visual potential remains viable and resumes its importance when SPK removes the oxidative stress. It is proposed that this allows remodeling of the microcirculation, once the chronic inflammation resolves, preventing the accumulation of cytokines (resulting in apoptosis and ischemia) and promoting the resolution of edema.Citation15 Normal neuronal structure and function can then recover.
Despite the lack of evidence of the effect of pancreas transplant on VA and some evidence suggesting that late disease is irreversible we have presented two cases of end-stage DR demonstrating improvement in VA after SPK. A prospective assessment of SPK and visual function in diabetic retinopathy would be valuable in providing visual prognosis and potentially elucidate the mechanisms of recovery in visual function.
Disclosures
The authors report no conflicts of interest in this work.
References
- SutherlandDEGruessnerRWDunnDLLessons learned from more than 1,000 pancreas transplants at a single institutionAnn Surg2001233446350111303130
- BandelloFViganoCSecchiAEffect of pancreas transplantation on diabetic retinopathy: a 20-case reportDiabetologia199134Suppl 1S92S941936706
- RamsayRCGoetzFCSutherlandDEProgression of diabetic retinopathy after pancreas transplantation in insulin-dependent diabetes mellitus patientsN Engl J Med198831842082143275895
- UlbigMKampikAThurauSLandgrafRLandWLong-term follow-up of diabetic retinopathy for up to 71 months after combined renal and pancreatic transplantationGraefe’s Arch Clin Exp Ophthalmol1991229242245
- AbendrothDSchmandJLandgrafRIllnerWDLandWDiabetic microangiopathy in type 1 (insulin-dependent) diabetic patients after successful pancreatic and kidney or solitary kidney transplantationDiabetologia199134Suppl 1S131S1341936678
- WangQKleinRMossSEThe influence of combined kidney-pancreas transplantation on the progression of diabetic retinopathy. A case seriesOphthalmology1994101107110768008349
- RamsayRCGoetzFCSutherlandDEProgression of diabetic retinopathy after pancreas transplantation for insulin-dependent diabetes mellitusNew Eng J Med19883182082143275895
- KonigsrainerAMillerKSteurerWDoes pancreas transplantation influence the course of diabetic retinopathy?Diabetologia199134Suppl 1S86S881936704
- ChowVCCPaiRPChapmanJRDiabetic retinopathy after combined kidney-pancreas transplantationClin Transplantation199913356362
- GiannarelliRCoppelliASartiniMSPancreas transplant alone has beneficial effects on retinopathy in type 1 diabetic patientsDiabetologia200649122977298217021920
- SpadellaCTMachadoJLMLercoMMOrtolanEVPSchelliniSAGregorioEATemporal relationship between successful pancreas transplantation and control of ocular complications in alloxan-induced diabetic ratsTrans Proc2008402518523
- CheungATPerezRVChenPCImprovements in diabetic microangiopathy after successful simultaneous pancreas-kidney transplantation: a computer-assisted intravital microscopy study on the conjunctival microcirculationTransplantation199968792793210532529
- The Diabetes Control and Complications Trial Research GroupThe effect of intensive treatment of diabetes on the development of and progression of long-term complications in insulin-dependent diabetes mellitusN Eng J Med1993329977986
- ParisiVUccioliLVisual electrophysiological responses in persons with type 1 diabetesDiabetes Metab Res Rev2001171121811241887
- AntonettiDABarberAJBronsonSKDiabetic retinopathy: seeing beyond glucose-induced microvascular diseaseDiabetes2006552401241116936187