Abstract
Purpose:
To report a case of a 25-year-old woman with previously treated peripheral T-cell lymphoma (PTCL) presenting with a recurrent lower eyelid lesion.
Patients and method:
Case report.
Results:
A 25-year-old young woman with previously treated PTCL noted an induration in the skin of her left lower eyelid. Upon diagnosis of a chalazion, antibiotic eye drops and ointments as well as steroid eye drops were administered. However, the condition worsened rapidly and swelling of the lower eyelid became remarkable. An excisional biopsy revealed that the palpebral lesion was diagnosed as recurrence of PTCL. Electron irradiation was applied as a radical treatment, and the prognosis was satisfactory without recurrence at 10 months after the last irradiation.
Conclusions:
Although lymphoma isolated to the ocular adnexa is rare, it should always be included in the differential diagnosis of any patient presenting with progressive swelling of the eyelid or ocular region.
Introduction
Peripheral T-cell lymphoma (PTCL) represents a broad spectrum of disease with several different manifestations. PTCL often occurs in the extremities, but rarely in the eyelid. Periocular involvement by PTCL usually occurs in the setting of the Sézary syndrome or mycosis fungoides, which is a variant of PTCL.Citation1–Citation4 We report a case of a 25-year-old young woman with previously treated PTCL presenting with a recurrent lower eyelid lesion.
Case report
The patient’s history dates back to 2006 when she had multiple skin lesions that were diagnosed as PTCL and subsequently excised. Submandibular and parotid lymph nodes were palpable, but there was no swelling of the liver or spleen. Blood tests were negative for adult T-cell leukemia antibody and human immunodeficiency virus (HIV) antibody and soluble interleukin-2 receptor was within normal range. No other lesion was detected by gallium scintigraphy or systemic computed tomography. A bone marrow trephine biopsy did not show the involvement of lymphoma. Immunostaining revealed the cells to be positive for CD3 and CD5, but negative for CD30, CD10, and CD75. Based on the findings, the patient was classified as PTCL Stage IVB according to the new World Health Organization classification.Citation5 As the patient was chemorefractory against initial treatment with combined cyclophosphamide, deoxorubicin, vincristine, and prednisone, she underwent allogenic stem cell transplantation from a matched non-sibling donor in March 2007 after salvage treatment with cyclophosphamide, cytosine arabinoside, etoposide, and dexamethasone. Transplant-conditioning therapy was cyclophosphamide, 2900 mg/day for three days, plus total body irradiation for three days (total 12 Gy). Graft-versus-host disease prophylaxis was provided with cyclosporine A and prednisolone. Cyclosporin levels were maintained between 300 and 400 μg/L until tapering was initiated. Initial dose of prednisolone was 17.5 mg per oral.
In January 2008, the patient presented to our department to check for any ocular manifestations of the graft-versus-host disease. At that time, significant superficial punctate keratopathy was noted in both eyes. Systemic skin and eyelids were macroscopically normal. Systemic lymph nodes were not palpable, and there was no swelling of the liver or spleen. The superficial punctate keratopathy significantly improved with eyedrops containing hyaluronan.
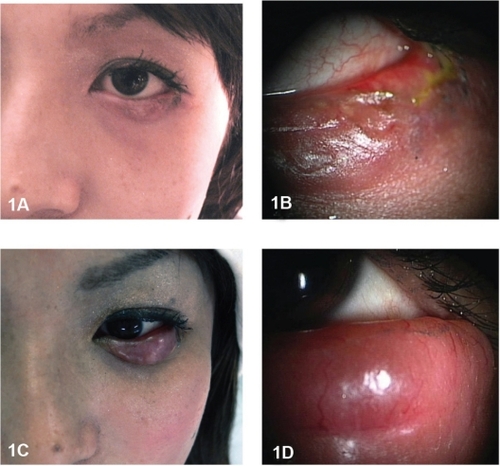
On July 11, 2008, the patient noted an induration in the skin of her left lower eyelid (). Conjunctival congestion and pain were present. Upon diagnosis of an acute chalazion, conservative management was used. However, the condition worsened rapidly, and swelling of the lower eyelid became remarkable ().
Figure 1 A) Patient with chalazion-like induration of the left lower eyelid on July 11, 2008. B) High magnification of the lower eyelid with chalazion-like presentation. C) After one month, induration of the lower eyelid became rapidly enlarged. Note a diffuse, erythematous, thickened lower eyelid. D) High magnification of the thickened lower eyelid.
On August 25, 2009, the patient underwent an excisional biopsy of the palpebral lesion after informed consent. A retention cyst in chalazion was not detected during the intraoperative microscopic examination. Pathological examination demonstrated that medium-sized lymphoma cells with round nuclei () had infiltrated subcutaneously. Immunostaining revealed the cells to be positive for CD3 (). Considering these results, the palpebral lesion was diagnosed as recurrence of PTCL.
Figure 2 A) Light micrograph of hematoxylin and eosin stained eyelid biopsy specimen. Lymphoma cells were infiltrated into the subcutaneous tissue. P, palpebral skin; Bar = 200 μm. B) High magnification of the lymphoma cells infiltrated in the orbicular muscles (arrows). Bar = 100 μm. C) Light micrograph of eyelid biopsy specimen immunostained with CD3 antibody. CD3 positive lymphoma cells were distributed in the subcutaneous tissue. Bar = 100 μm. Photographs of eyelids before D) and after irradiation E) The eyelid tumor was dramatically improved after irradiation.
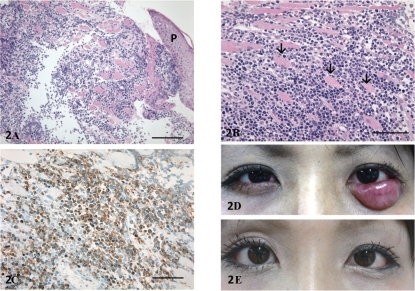
As the lesion was limited to the left lower eyelid, 25.2 Gy electron irradiation was applied as a radical treatment. Globe shielding was used to help prevent radiation retinopathy. The eyelid tumor was dramatically improved after irradiation (, ). The prognosis was satisfactory without recurrence at 10 months after the last irradiation.
Discussion
Ocular manifestations of PTCL can include both intraocular and extraocular conditions.Citation1–Citation4 Cook and colleaguesCitation6 reported that eyelid ectropion was the most common findings in their patients with PTCL, though other ocular manifestations, including eyelid thickening or edema, placoid tumor, tight skin, blepharitis, and corneal abnormalities, were also found. Stenson and RamsayCitation7 found eyelid tumors in eight of 30 consecutive patients with mycosis fungoides diagnosed by biopsy. Isolated PTCL of the eyelid is rare.Citation8,Citation9 Gilbertson and colleaguesCitation1 reported a case of a 38-year-old acquired immunodeficiency syndrome (AIDS) patient with isolated eyelid PTCL, and found only eight previous reports of isolated PTCL, most diagnosed as mycosis fungoides. In this type of lymphoma, relapses are common and can produce an indolent course. Kirsch and colleagues reported a patient with multiple recurrences of systemic T-cell lymphoma after initial presentation with only an eyelid mass that was treated with systemic chemotherapy and local radiation.Citation4
The present case was a single episode of lymphoma of the eyelid with clinical symptoms resembling a chalazion. However, an excisional biopsy of the current lesion confirmed the recurrence of the actual tumor and so ruled out a chalazion. The current case still requires close follow-up observation, particularly of the skin around the lesion. When radiation therapy is used for eyelid lesions, great care must be taken with ocular side effects, including xerophthalmia and radiation retinopathy.Citation6 Although lymphoma isolated to the ocular adnexa is rare, it should always be included in the differential diagnosis of any patient presenting with progressive swelling of the eyelid or ocular region, particularly with a history of lymphoma.
Disclosures
The authors report no conflicts of interest in this work.
References
- GibertsonEOHuntSJSpellmanMCCutaneous T-cell lymphoma of the eyelid in a patient with acquired immunodeficiency syndromeCutis1996564374408804850
- MeekinsBProiaADKlintworthGKCutaneous T-cell lymphoma presenting as a rapidly enlarging ocular adnexal tumorOphthalmology198592128812933877264
- HendersonJWBanksPMYeattsRPT-cell lymphoma of the orbitMayo Clin Proc1989649409442796404
- KirschLSBrownsteinSCodereFImmunoblastic T-cell lymphoma presenting as an eyelid tumorOphthalmology199097135213572243687
- JaffeESHarrisNLSteinHVardimanJMPathology and Genetics of Tumors of Haematopoietic and Lymphoid TissuesLyon, FranceIARC Press2001
- CookBEJrBartleyGBPittelkowMROphthalmic abnormalities in patients with cutaneous T-cell lymphomaOphthalmology19991061339134410406618
- StensonSRamsayDLOcular findings in mycosis fungoidesArch Ophthalmol1981992722777469864
- MitoHKakizakiHTsujiHPeripheral T-cell lymphoma of the eyelidJpn J Ophthalmol20065038839016897229
- IngEHsiehEMacdonaldDCutaneous T-cell lymphoma with bilateral full-thickness eyelid ulcerationCan J Ophthalmol20054046746816116511