Abstract
Purpose:
To determine the efficacy and safety of treating predominantly hemorrhagic age-related macular degeneration (AMD) with transconjunctival sutureless vitrectomy (TSV), tissue plasminogen activator (tPA), sulphur hexafluoride (SF6), and intravitreal bevacizumab.
Methods:
Retrospective study, consecutive case series. Patients with acute hemorrhagic AMD treated with 25- or 23-gauge TSV, subretinal or intravitreal tPA, fluid-air-SF6 exchange and intravitreal injection of bevacizumab. All operations were performed within the first 5 days after the start of symptoms, which consisted of visual acuity (VA) loss and central scotoma.
Results:
Fifteen eyes from 15 patients were included. The patients’ mean age was 79.6 years, and the mean follow-up was 11.8 months. Five patients (33%) were receiving oral anticoagulant treatment. At baseline, the mean VA (logMAR values) was 1.5 (20/640 Snellen equivalent). At the last follow-up visit, the mean VA was 1.1 (20/250) (P < 0.0001; paired t-test). The submacular hemorrhage was successfully displaced in all the cases. Complications consisted of three cases of vitreous hemorrhage and a tear or the retinal pigment epithelium. Twelve cases (80%) did not require further treatment during the follow-up period.
Conclusion:
A surgical approach with 25- or 23-gauge TSV, tPA, SF6 and intravitreal bevacizumab is an efficacious and safe procedure in patients with hemorrhagic AMD. Early treatment is advisable for obtaining the optimal outcome.
Introduction
Submacular hemorrhages can arise from retinal or choroidal circulation associated with age-related macular degeneration (AMD), arterial macroaneurysms and severe traumas. Several factors, such as a release of toxins, tractional forces acting on the retina and a diffusion barrier created by the hemorrhage can promote photoreceptor damage and a loss of visual acuity (VA).Citation1
To date, intravitreal injections of anti-vascular endothelial growth factor (anti-VEGF) drugs have been the gold standard for the treatment of choroidal neovascularization (CNV) secondary to AMD. Notwithstanding, clinical trials used for drug approval, such as the MARINA and ANCHOR studies of ranibizumab, excluded patients with predominantly hemorrhagic lesions.Citation2
In contrast, the Submacular Surgery Trial did not report favorable results in patients with subfoveal hemorrhagic lesions secondary to neovascular AMD.Citation3
Photodynamic therapy (PDT) with verteporfin has been proven, with limited success, in these patients as well.Citation4
Peyman and colleaguesCitation5 were the first to report the success of a subretinal injection of tPA in five patients with submacular hemorrhages related to arterial macroaneurysms and AMD. They claimed that tPA administration reduced the surgical manipulation of the retina and allowed a smaller retinotomy to drain the blood.
Since then, several techniques have been described. Some have proposed pneumatic displacement of the hemorrhage combined with subretinal tPA and gas.Citation6,Citation7 Olivier and colleaguesCitation8 published a study of 29 eyes in 28 patients, using this technique to treat thick submacular hemorrhages secondary to AMD. They achieved a total displacement of the subfoveal blood in 25 cases and 17 eyes gained ≥2 lines of VA. Reported complications included two cases of vitreous hemorrhage that cleared within 4 weeks.
Other authors have proposed that intravitreal injections of tPA and expansile gas can be used without vitrectomy.Citation9 Chen and colleaguesCitation10 used this treatment to obtain satisfactory results in 104 eyes, although they reported eight cases of vitreous hemorrhage and three cases of retinal detachment.
Other techniques described in the literature include pneumatic displacement without tPACitation11 and the preoperative intravitreal injection of tPA.Citation12
A recent study found favorable results with a triple injection of tPA, gas, and bevacizumab without vitrectomy.Citation13
The aim of the present study was to determine the efficacy and safety of the treatment of hemorrhagic AMD with 25- or 23-gauge transconjunctival sutureless vitrectomy (TSV), tPA, sulphur hexafluoride (SF6), and intravitreal bevacizumab.
Methods
This is a retrospective study comprised of consecutive case series of patients with submacular, predominantly hemorrhagic lesions (blood ≥ 50% of total lesion size) secondary to neovascular AMD. Patients were operated at the Institut de la Màcula i de la Retina and at the Hospital Universitari de Bellvitge between May 2007 and November 2008. All the included patients had been diagnosed of neovascular AMD. Based on clinical features of previously treated patients and status of the fellow eye we did not identify any polypoidal choroidal vasculopathy or any other cause of submacular hemorrhage.
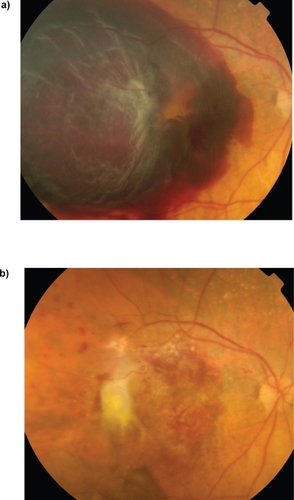
A single surgeon (LA) operated on all of the recruited patients within the first 5 days after the beginning of the symptoms, which consisted of VA loss and a central scotoma. A 25- or 23-gauge TSV was performed under retrobulbar anesthesia with posterior hyaloid dissection. In cases with a thick submacular hemorrhage, two or three retinotomies were performed with subretinal injection of tPA (concentration of 125 mg/mL of balance salt solution) using a 39-gauge tip cannula. Subsequently, a fluid-air-20% SF6 exchange was performed with a final intravitreal injection of bevacizumab. In cases with a flat submacular hemorrhage, an intravitreal injection of tPA was administered after the fluid-air-gas exchange. A thick hemorrhage was defined as one causing a significant bulging and elevation of the macular surface from the posterior pole plane ().
Figure 1 Female aged 89 years (patient no. 5). Baseline fundus photograph (a) and 2 months after the surgery (b). Visual acuity improved from 20/1000 to 20/400. No further treatment was needed during the 12-month follow-up.
Patients were left lying on their back for 1 hour after the surgical procedure, and were subsequently instructed to keep a face-down position for 3 days. Follow-up visits were performed 24 hours and 1 week after the surgery, and then monthly. They included VA measurement using Early Treatment Diabetic Retinopathy Study (ETDRS) charts, anterior segment examination, intraocular pressure measurement, funduscopic examination and retinographies. Additional fluorescein angiography (FA) and optical coherence tomography (OCT) scans were performed at the investigator’s discretion.
During follow-up examinations, patients who exhibited CNV activity were treated, as usual, with intravitreal injections of anti-VEGF agents.
Results
The present study included 15 eyes of 15 patients; 10 women (67%) and five men (33%). The affected eye was right in eight cases (53%) and left in seven cases (47%). Six patients (40%) were phakic, eight patients (53%) were pseudophakic and one patient (7%) was aphakic. Eleven patients (73%) had an advanced AMD in the fellow eye and one patient (7%) had lost vision in the other eye due to a neovascular glaucoma secondary to a central retinal vein occlusion ().
Table 1 Characteristics of patients included in the study
The mean age of the patients was 79.6 years (standard deviation [SD]: 8.6 years; range: 62–94 years). The mean follow-up after the surgery was 11.8 months (SD: 8.3 months; range: 3–24 months).
Eight patients (53%) had been previously treated in the study eye with PDT or intravitreal injections of anti-VEGF drugs ().
Five patients (33%) were receiving treatment with oral anticoagulant drugs for heart arrhythmia. Four of the five patients under coumadin therapy were among the cases with the most massive bleeds ().
Three of the operations (20%) were performed using 23-gauge TSV and 12 cases (80%) using 25-gauge TSV. Combined cataract surgery consisting of phakoemulsification plus intraocular lens was performed in two cases (13%).
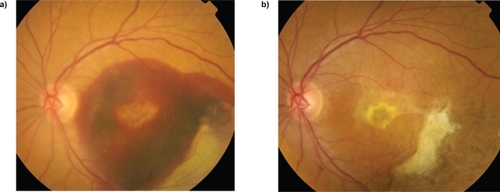
In eight cases (53%) with thick submacular hemorrhage we performed subretinal injection of tPA (), and in the other seven cases (47%), characterized by flat submacular hemorrhage, an intravitreal injection of tPA was administered after the fluid-air-gas exchange ().
Figure 2 Female aged 76 years (patient no. 8). Baseline fundus photograph (a) and 12 months after the surgery (b). Visual acuity improved from 20/800 to 20/200. No further treatment was needed during the 20-month follow-up.
Lesion size ranged from 15 mm2 (5.5 disc areas) to 41 mm2 (15 disc areas). The mean lesion size was 33.1 mm2 (SD: 4.2 mm2) in the patients with thick submacular hemorrhages and 19.4 mm2 (SD: 3.3 mm2) in the patients with flat submacular hemorrhages.
The submacular hemorrhage was successfully displaced in all cases. At baseline, the mean VA (logMAR values) was 1.5 (SD: 0.2) (20/640 Snellen equivalent). At the last follow-up visit, the mean VA was 1.1 (SD: 0.3) (20/250 Snellen equivalent) (P < 0.0001; paired t-test). The mean VA (ETDRS) improved from 9.4 letters to 28.2 letters with a mean change of +18.7 letters (P < 0.0001; paired t-test). Eleven patients (73%) gained 15 or more letters of VA.
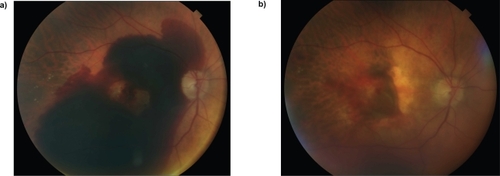
Complications consisted of three cases (20%) of vitreous hemorrhage that spontaneously resolved after 2–3 weeks. Additionally, one patient (7%) had a tear of the retinal pigment epithelium (RPE) ().
Figure 3 Male aged 83 years (patient no. 3). Baseline fundus photograph (a) and 2 weeks after the surgery showing a tear of the retinal pigment epithelium (b).
Twelve cases (80%) did not require further treatment during the follow-up period. Three cases (20%) were treated with additional intravitreal injections of anti-VEGF drugs ().
Table 2 Main results of the study
Discussion
The present study found a favorable outcome of managing predominantly hemorrhagic lesions, secondary to AMD, with TSV combined with tPA, SF6, and intravitreal bevacizumab. The submacular hemorrhage was successfully displaced in all cases, and the mean VA significantly improved after surgical treatment.
Recently, Meyer and colleaguesCitation13 published a study using a triple intravitreal injection of tPA, gas and bevacizumab without vitrectomy in 19 patients with acute subretinal hemorrhages. The initial size of the lesion was 1–3 disc diameters. In our study, lesion size was bigger, ranging from 15 mm2 (5.5 disc areas) to 41 mm2 (15 disc areas). In their study, the mean VA improved significantly from 20/133 at baseline to 20/74 at 3 months. In our study, the mean VA improved from 20/640 to 20/250. However, the mean ETDRS VA improvement was very similar in both studies (3.7 lines in their study compared with 3.6 lines in ours). Thus, a surgical approach in large lesions can obtain comparable results to a triple intravitreal injection procedure in smaller hemorrhagic lesions.
In our study, 33% of patients received oral anticoagulants. It is known that this medication significantly increases the risk of an intraocular hemorrhage in wet AMD patients.Citation14
We decided to perform a posterior vitrectomy to minimize the risk of vitreoretinal tractions that could be associated with the single administration of intravitreal injections. In addition, a surgical approach seems advisable taking into account the large size of the lesions included in our study. Current systems of microincisional TSV allow efficacious, safe and swift surgery with minimal eye trauma and discomfort for the patient. However, we do not think that 25 g or 23 g vitrectomy may achieve better anatomical or functional outcome compared with that using 20 g instruments.
In cases of thick submacular hemorrhages, we injected subretinal tPA as previously described by Olivier and colleagues.Citation8 In cases of flat submacular hemorrhages, we decided to perform an intravitreal tPA injection to reduce possible damage to photoreceptors and RPE cells associated with subretinal manipulation. The final results were better in the patients with flat submacular hemorrhages than in the patients with thick hemorrhages. This could be related to the smaller lesion size in the patients with flat hemorrhages.
We used SF6 because we believe that a short-acting gas is sufficient to obtain an adequate pneumatic displacement of the submacular hemorrhage.
In accordance with an experimental study published by Lüke and colleagues,Citation15 we decided to administer a final intravitreal injection of bevacizumab. Their study showed that tPA and bevacizumab are compatible drugs with no evidence of retinal toxicity. Moreover, the potent antiangiogenic effect associated with bevacizumab could be beneficial for reducing CNV activity. In fact, 80% of patients in our study did not require further treatment during the follow-up period. However, no strong evidence suggests bevacizumab is associated with more prompt or thorough lesion regression.
The only complications we detected were three cases of mild vitreous hemorrhage that spontaneously cleared within the first few weeks. It is logical that the liquefied subretinal blood enters the vitreous cavity to get reabsorbed posteriorly. None of our patients had a retinal tear or retinal detachment.
We observed a single tear of the RPE after resolution of the submacular hemorrhage. It was not clear whether the tear was present preoperatively or developed after the surgery. RPE rips have been described in large submacular hemorrhages in wet AMD patients.Citation16
All operations were performed within the first 5 days after the patients first experienced symptoms. Olivier and colleaguesCitation8 reported an average submacular hemorrhage duration of 23 days before surgery. Meyer and colleaguesCitation13 reported a mean duration of symptoms of 9 days (range: 4–12 days). We believe that optimal results in these cases are dependent upon early surgery to avoid irreversible damage to photoreceptors and RPE cells.
Limitations of this study are that it was retrospective, noncomparative, nonrandomized and included few patients with a limited follow-up. It is difficult to enroll a large number of cases with this macular disorder.
In conclusion, this small study has shown efficacy and safety in the management of predominantly hemorrhagic AMD lesions with an early TSV with tPA, gas and intravitreal bevacizumab.
Larger multicenter randomized studies are warranted to determine the real therapeutic effect of this surgical approach.
Disclosure
The authors have no financial or proprietary interest in any product mentioned in this article and received no financial support in this work.
References
- HochmanMASeeryCMZarbinMAPathophysiology and management of subretinal hemorrhageSurv Ophthalmol1997421952139406367
- RosenfeldPJBrownDMHeierJSRanibizumab for neovascular age-related macular degenerationN Engl J Med20063551419143117021318
- BresslerNMBresslerSBChildsALSubmacular Surgery Trials (SST) Research Group. Surgery for hemorrhagic choroidal neovascular lesions of age-related macular degeneration: ophthalmic findings: SST report no. 13Ophthalmology20041111993200615522364
- AhmadSBearellySStinnettSSCooneyMJFekratSPhotodynamic therapy for predominantly hemorrhagic lesions in neovascular age-related macular degenerationAm J Ophthalmol20081451052105718400198
- PeymanGANelsonNCJrAlturkiWTissue plasminogen activating factor assisted removal of subretinal hemorrhageOphthalmic Surg1991225755821961614
- HaupertCLMcCuenBWIIJaffeGJPars plana vitrectomy, subretinal injection of tissue plasminogen activator, and fluid-gas exchange for displacement of thick submacular hemorrhage in age-related macular degenerationAm J Ophthalmol200113120821511228297
- SinghRPPatelCSearsJEManagement of subretinal macular haemorrhage by direct administration of tissue plasminogen activatorBr J Ophthalmol20069042943116547320
- OlivierSChowDRPackoKHMacCumberMWAwhCCSubretinal recombinant tissue plasminogen activator injection and pneumatic displacement of thick submacular hemorrhage in age-related macular degenerationOphthalmology20041111201120815177972
- HassanASJohnsonMWSchneidermanTEManagement of submacular hemorrhage with intravitreous tissue plasminogen activator injection and pneumatic displacementOphthalmology19991061900190610519583
- ChenCYHooperCChiuDManagement of submacular hemorrhage with intravitreal injection of tissue plasminogen activator and expansile gasRetina20072732132817460587
- OhjiMSaitoYHayashiALewisJMTanoYPneumatic displacement of subretinal hemorrhage without tissue plasminogen activatorArch Ophthalmol1998116132613329790631
- OshimaYOhjiMTanoYPars plana vitrectomy with peripheral retinotomy after injection of preoperative intravitreal tissue plasminogen activator: a modified procedure to drain massive subretinal haemorrhageBr J Ophthalmol20079119319816916872
- MeyerCHSchollHPEterNHelbHMHolzFGCombined treatment of acute subretinal haemorrhages with intravitreal recombined tissue plasminogen activator, expansile gas and bevacizumab: a retrospective pilot studyActa Ophthalmol20088649049418221499
- TilanusMAVaandragerWCuypersMHVerbeekAMHoyngCBRelationship between anticoagulant medication and massive intraocular hemorrhage in age-related macular degenerationGraefes Arch Clin Exp Ophthalmol200023848248510943671
- LükeMJanuschowskiKWargaMThe retinal tolerance to bevacizumab in co-application with a recombinant tissue plasminogen activatorBr J Ophthalmol2007911077108217383998
- BiesterSBartz-SchmidtKUGeliskenFRetinal pigment epithelial tear after subretinal rtPA and intravitreal air for the displacement of a large submacular hemorrhageRetinal Cases and Brief Reports2009316263