Abstract
Purpose
To report corneal lamellar grafting to repair the late-onset complications after MMC trabeculectomy.
Methods
Multiple case reports.
Results
A 76-year-old male with primary open-angle glaucoma (POAG) and a 55-year-old male with late developmental glaucoma complicated by bleb leaks from a microhole 10 and eight years after surgery, respectively. Severe ciliochoroidal detachment and a shallow anterior chamber were persistent in one case and bleb-related infection recurred in another. Additionally, a 46-year-old male with POAG had hypotony maculopathy with a giant ischemic bleb 18 months after surgery. Although these patients were quite resistant to medical and surgical treatments, they were successfully treated by corneal lamellar grafting without complications.
Conclusions
Tectonic corneal lamellar grafting is a reliable and final surgical method to improve severe cases of hypotony maculopathy or bleb leak after mitomycin C trabeculectomy.
Introduction
Mitomycin C (MMC) trabeculectomy is still used worldwide as a convenient and effective method to reduce intraocular pressure (IOP) in glaucomatous eyes that cannot be controlled with maximum tolerated doses of medications.Citation1–Citation7 Soon after ChenCitation1 introduced MMC as an adjunctive agent during trabeculectomy, cases of hypotony associated with a shallow-to-flat anterior chamber or ciliochoroidal detachment were often seen because of the strong antifibroblastic effect of MMC.Citation8–Citation10 Once such complications occurred, they tended to persist for long periods. MMC trabeculectomy with laser suture lysisCitation11–Citation13 or non-penetrating filtering surgeryCitation14,Citation15 were recommended to decrease postoperative complications related to hypotony in the early phase. Although these reliable modifications greatly reduced the occurrence of hypotony maculopathy, this complication still occurs. In addition, late-onset hypotony after MMC trabeculectomy often occurs with a bleb leak because of microhole formation.Citation16–Citation20 While a bleb leak as a result of microhole formation may result in hypotony, a shallow anterior chamber, or ciliochoroidal detachment, it is thought to be related closely to blebitis or endophthalmitis as the most severe complications after MMC trabeculectomy.Citation21,Citation22
We treated three patients who had severe complications associated with MMC trabeculectomy with corneal lamellar grafting. Two patients had bleb leaks from a microhole and another had a rare case of slow-onset hypotony maculopathy. We present these cases and discuss corneal lamellar grafting as a reliable and final surgical treatment for severe hypotony or bleb leaks after MMC trabeculectomy.
Case reports
Case 1
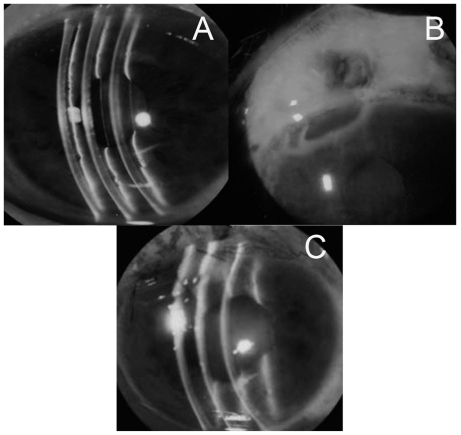
A 76-year-old Japanese male with POAG underwent MMC trabeculectomy in his left eye in July 1994 (at 65 years of age). The surgical method for MMC trabeculectomy was followed as previously reported.Citation23 MMC was applied at 0.02 mg/mL for five minutes. His postoperative left IOPs were kept between 9 and 12 mmHg. In December 2004, he visited our clinic complaining of left conjunctival infection and blurred vision. His left eye had associated leakage from a microhole of the bleb with Seidel’s phenomenon (), a shallow anterior chamber of Grade 1 by Spaeth’s classificationCitation24 (), and a marked circumferential ciliochoroidal detachment.
Figure 1 Case 1 was complicated by a shallow anterior chamber (A) because of bleb leakage with Seidel’s phenomenon (B). After corneal lamellar grafting, the anterior chamber had kept deep (C) and the IOP had also increased.
We tried several medical and surgical treatments, including administration of an oral carbonic anhydrase inhibitor, injection of autologous blood into the bleb, and repeated bleb reformation with compression sutures, but they provided only temporal relief. Finally, we decided to perform corneal lamellar grafting.
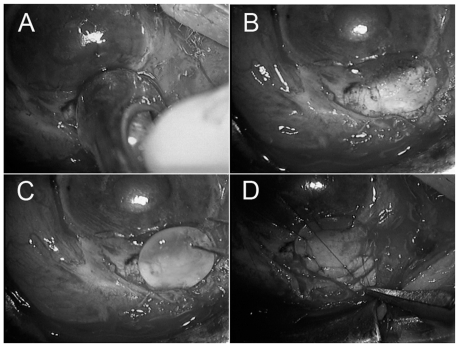
After the anterior chamber formation with hyalonate and conjunctival incision, surgical debridement was performed on scarred conjunctiva and soft tissues on the sclera. Half-layered corneoscleral tissues, including the area of weakened spongy sclera, were dissected away using a corneal trephine 5.5 mm in diameter (). Clean, healthy edges of the dissection were regularized (). Then, donor corneal tissue was used to repair the corneoscleral defect. A round lamellar preserved corneal piece, 5.5 mm in diameter and 0.8 mm thick, was made using a corneal trephine. The piece was sutured exactly to the patient’s cleaned-up corneoscleral area with 10-0 nylon (). A total of eight sutures were placed and made water tight. The conjunctiva was left free except for both edges, which were grafted and sutured with 10-0 nylon. An antibiotic, ofloxacin, and a steroid, 0.1% betamethasone, were prescribed as postoperative medications to be taken four times a day. Oral prednisolone was prescribed at 30 mg per day and then tapered off at the end of the three-week postoperative period.
Figure 2 Using a corneal trephine (5.5 mm diameter), half-layered corneoscleral tissues was dissected away (A). Clean, healthy edges of the dissection were regularized (B). Then a donor’s lamellar, round, preserved corneal piece with 5.5 mm diameter and 0.8 mm thickness was placed (C) and was sutured exactly to the patient’s corneoscleral area with 10-0 nylon (D).
His left IOP increased to 48 mmHg on the second day. The IOPs were controlled between 15 and 18 mmHg with topical medications. The left anterior chamber remained deep without subsequent ciliochoroidal detachment.
Case 2
A 55-year-old Japanese male diagnosed with late developmental glaucoma received MMC trabeculectomy by a procedure similar to that used in case 1 in 1992 (at 42 years of age). His left IOP was kept between 5 and 8 mmHg without medication. When blebitis with bleb leak from a microhole occurred in his left eye in December 2000, medical treatments were effective. After blebitis recurred in March 2001, the bleb resection and autologous free conjunctival patch grafting were performed after administration of an oral carbonic anhydrase inhibitor and injection of autologous blood into the bleb. In 2004, bleb leak from a microhole recurred and the IOP decreased to 5 mmHg. We performed corneal lamellar grafting using the same procedure as in case 1. After increasing to 27 mmHg on the next day, the IOPs were maintained between 10 to 13 mmHg with topical medications, and no leakage or blebitis occurred again after the surgery.
Case 3
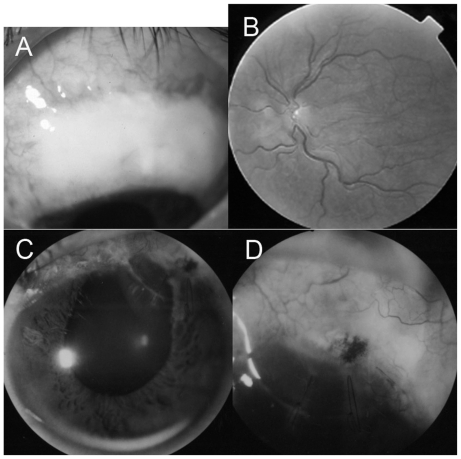
A 46-year-old Japanese male with POAG underwent MMC trabeculectomy in both eyes in April 1996 (at 42 years of age). The postoperative IOP decreased to 11 mmHg at three months, 7 mmHg at six months and 4 mmHg at 12 months. Finally, his left IOP was 3 mmHg with a giant ischemic bleb () and typical hypotony maculopathy () at 18 months post surgery. The corrected visual acuity was 20/20 at three months and 4/20 at 18 months. Although we tried several medical and surgical treatments, including oral carbonic anhydrase inhibitors, conservative injection of autologous blood, surgical compression sutures, and direct conjunctival cover, his hypotony maculopathy never improved. Finally, we performed corneal lamellar grafting following the same procedure as described for case 1 () at 40 months after the initial MMC trabeculectomy. Similarly the IOP increased up to 46 mmHg on the next day, but decreased to 22 mmHg within a week with oral and topical medications. The hypotony maculopathy improved within two weeks. The corrected visual acuity increased to 10/20 at 12 months and 18/20 at 60 months after the corneal grafting. His left IOP has remained between 14 and 18 mmHg only with topical medications, and his left visual field defect has shown no notable progression.
Figure 3 Case 3 had a giant ischemic bleb (A) and hypotony after MMC trabeculectomy. His left fundus showed typical hypotony maculopathy (B). After corneal lamellar grafting, the anterior chamber had remained deep (C) and the IOP had increased because of complete closure of the scleral cleft (D).
Discussion
Cases 1 and 2 had complicated bleb leaks from a microhole. Case 1 had combined hypotony with the shallow anterior chamber and circumferential ciliochoroidal detachment while bleb-related infections recurred in case 2. The occurrence of bleb leaks had been increasing because of the use of antifibrolytic agents, 5-fluorouracil, or MMC, and to time progress after filtering surgeries.Citation20 Bleb-related infections, blebitis, or endophthalmitis, are reported to be the most severe complications after MMC trabeculectomy and are closely related to bleb leaks.Citation21,Citation22 Microholes can supply a route for bacteria from the ocular surface into the bleb and eye. Case 3 was a rare case of slow-onset hypotony maculopathy with a large ischemic bleb. Generally, hypotony maculopathy after MMC trabeculectomy results from persistent overfiltration, ciliochoroidal detachment, hyposecretion of aqueous humor or leakage from an epithelial defect, a microhole, or insufficient sutures from the early postoperative periods.Citation8–Citation10 The IOPs were over 10 mmHg in the early postoperative phase, but both the IOPs and visual acuity decreased slowly over 18 months in case 3. An experiment has shown that the anti-fibrotic effects of MMC can continue for the long term.Citation25
The treatments for hypotony with overfiltration or bleb leak are summarized in Citation24,Citation26 which was modified slightly from Azuara-Blanco.Citation26 These therapies give a range of choices, ranging from conservative to surgical treatments. For initial conservative methods, a pressure eye patch and an oral carbonic anhydrase inhibitor are often recommended. Bleb injection of autologous blood,Citation27 bandage contact lenses, and topical application of a chemical irritant,Citation28 may be the next corrective steps. symblepharon rings or Simmons shell, laser therapy with argon or Nd:YAG laser,Citation29 cryotherapy, and diathermy have also been reported as treatment methods before surgical procedures. We tried a pressure eye patch, oral carbonic anhydrase administration and bleb injection of autologous blood in all cases, but with minimal effects. As a next step, we should consider relatively conservative surgical methods, such as compression sutures over the bleb, direct resuture, or scleroconjunctival suture of the scleral flap. In particular, the bleb leak from a microhole generally requires surgical treatmentCitation30,Citation31 as in cases 1 and 2. Microholes are made repeatedly because of the very thin and weak ischemic bleb wall. Compression sutures had no notable effects in cases 1 and 3. We tried direct sutures of the sclera flaps but the MMC-treated sclera was too weak to suture in cases 2 and 3. Therefore, we considered performing patch grafting. The materials for patch grafting include the autologous conjunctivaCitation32 or amniotic membranes.Citation33 The autologous conjunctiva is the most common and easiest to handle of the materials for patch grafting. It is recommended for primary surgery but not for more resistant and more complicated cases. Although almost two-third of cases with conjunctival grafting have maintained a low IOP, the effect is imperfect and bleb leakage often recurs.Citation32 More recently, amnionic membranes have been used as patch grafts to reduce stromal melting and promote re-epithelialization in extensive infectious scleral and corneoscleral ulcers.Citation34 Amniotic membranes are not yet commercially available and several procedures are necessary to use this membrane clinically in Japan. The other common materials for anterior segment reconstruction are preserved sclera,Citation35,Citation36 pericardium,Citation37 and dura matter.Citation38 Scleral tissue is not readily available in Japan and caution must be taken to avoid immunogenicity. For the cases presented here, a preserved cornea is the most suitable grafting tissueCitation39–Citation41 because we had to close the scleral cleft completely and enable their IOPs to increase for recovery from long-term treatments. Similar to our report, Ti and TanCitation41 reported 20 cases with severe scleral melting after pterygium surgery that were treated with lamellar corneal grafting, and noted that corneal tissue has some constructive advantages over scleral tissue and allows lamellar dissection for a better graft-host fit. For these types of cases, Kosmin and WishartCitation36 treated with full thickness scleral grafting and Mistlberger et alCitation40 with dissection by an Excima laser and lamellar corneal grafting. Mistberger noted that a corneal graft is better than the scleral graft because there is less vascularization and scar formation after corneal grafting than after scleral grafting. Our method slightly differed from those reported previously because the corneal graft completely covered the filtering site when placed over the cornea and sclera.
Table 1 Treatments for hypotony with hyperfilteration or a leaking bleb after MMC trabeculectomy
Although a corneal or sclera patch must be used to close the scleral cleft and to free these cases from long-term complications, the biggest issue was the loss of the IOP-lowering effect of trabeculectomy. Fortunately, IOPs in all cases were maintained with topical medications, despite a temporary rise just after the surgery. When elevated postoperative IOPs cannot be controlled with medications, repeated MMC trabeculectomy may be difficult because of conjunctival conditions and other problems. A Seton shunt operation in the other operative area or cyclophotocoagulation can be considered in this condition.
Corneal lamellar grafting is a reliable and final surgical method to improve severe cases of hypotony maculopathy or bleb leak after MMC trabeculectomy.
Disclosures
The authors report no conflicts of interest in this work.
References
- ChenCWEnhanced intraocular pressure controlling effectiveness of trabeculectomy by local application of mitomycin-CTrans Asia Pacific Acad Ophthalmol198391172177
- KitazawaYTaniguchiTNakanoYShiratoSYamamotoT5-Fluorouracil for trabeculectomy in glaucomaGrafes Arch Clin Exp Ophthalmol19872256403405
- SinghKMehtaKShaikhNMTrabeculectomy with intraoperative mitomycin C versus 5-fluorouracil. Postoperative randomized clinical trialOphthalmology2000107122305230911097613
- PalmerSSMitomycin C as adjunct chemotherapy with trabeculectomyOphthalmology19919833173212023752
- BeckersHJKindersKCWebersCAFive-year results of trabeculectomy with mitomycin CGrafes Arch Clin Exp Ophthalmol20032412106110
- FontanaHNouri-MahdaviKLumbaJRalliMCaprioliJTrabeculectomy with mitomycin C: Outcomes and risk factors for failure in phakic open-angle glaucomaOphthalmology2006113693093616647135
- ShigeedaTTomidokoroAChenYNShiratoSAraieMLong-term follow-up of initial trabeculectomy with mitomycin C for primary open-angle glaucoma in Japanese patientsJ Glaucoma200615319519916778640
- ShieldsMBScroggsMWSloopCMSimmonsRBClinical and histopathologic observations concerning hypotony after trabeculectomy with adjunctive mitomycin CAm J Ophthalmol199311666736838250068
- Suemori-MatsushitaHOkabeIYamamotoTHypotonic maculopathy following trabeculectomy with mitomycin CNippon Ganka Gakkai Zasshi1995993312317 Japanese7732923
- LiebmannJMRitchRRitchRShieldsMBKrupinTComplications of glaucoma filtering surgeryThe Glaucomas2nd edSt. Louis, MOCV Mosby199617031706
- GeijssenHCGreveELPrevention of hypotony after trabeculectomies with mitomycinDoc Ophthalmol199385145498181425
- MorinelliENSidotiPAHeuerDKLaser suture lysis after mitomycin C trabeculectomyOphthalmology199610323063148594519
- KapetanskyFMLaser suture lysis after trabeculectomyJ Glaucoma200312431632012897576
- DemaillyPLavatPKretzGJeanteur-LunelMNNon-penetrating deep sclerectomy (NPDS) with or without collagen device (CD) in primary open-angle glaucoma: Middle-term retrospective studyInt Ophthalmol1997201–31311409112177
- FukuchiTSudaKNakatsueTHaraHAbeHMidterm results and the problems of nonpenetrating lamellar trabeculectomy with mitomycin C for Japanese glaucoma patientsJpn J Ophthalmol2007511344017295138
- AnandNAraraSClowersMMitomycin C augmented glaucoma surgery: Evolution of filtering bleb avascularity, transconjunctival oozing, and leaksBr J Ophthalmol200692217518016424529
- BelyeaDADanJAStamperRLLiebermanMFSpencerWHLate onset of sequential multifocal bleb leaks after glaucoma filtration surgery with 5-fluorouracil and mitomycin CAm J Ophthalmol1997124140459222231
- GreenfieldDSLiebmannJMJeeJRitchRLate-onset bleb leaks after glaucoma filtering surgeryArch Ophthalmol199811644434479565040
- HuCYMatsuoHTomitaGClinical characteristics and leakage of functioning blebs after trabeculectomy with mitomycin-C in primary glaucoma patientsOphthalmology2003110234535212578779
- MatsuoHTomidokoroASuzukiYShiratoSAraieMLate-onset transconjunctival oozing and point leak of aqueous humor from filtering bleb after trabeculectomyAm J Ophthalmol2002133445646211931778
- MochizukiKJikiharaSAndoYHoriNYamamotoTKitazawaYIncidence of delayed onset infection after trabeculectomy with adjunctive mitomycin C or 5-fluorouracil treatmentBr J Ophthalmol199781108778839486030
- MuckleyEDLehrerRALate-onset blebitis/endophthalmitis: Incidence and outcomes with mitomycin COptom Vis Sci200481749950415252348
- FukuchiTHayakawaYHaraHAbeHCornal endothelial damage after trabeculectomy with Mitomycin C in two patients with glaucoma with cornea guttataCornea200221330030411917180
- SpaethGLSpaethGLGlaucoma surgeryOphthalmic Surgery: Principles and PracticePhiladelphia, MAWB Saunders1982335343
- NuytsRMFeltenPCPelsEHistopathologic effects of mitomycin C after trabeculectomy in human glaucomatous eyes with persistent hypotonyAm J Ophthalmol199411822252378053469
- Azuara-BlancoAKatzLJDysfunctional f iltering blebsSurv Ophthalmol1998432931269763136
- SmithMFMagauranRDoyleJWTreatment of postf iltration bleb leak by bleb injection of autologous bloodOphthalmic Surg19942596366377831011
- ZaltaAHWiederRHClosure of leaking blebs with cyanoacrylate tissue adhesiveBr J Ophthalmol19917531701732012785
- GeyerOManagement of large, leaking, and inadvertent filtering blebs with the neodymium: YAG laserOphthalmology199810569839879627645
- BudenzDLChenPPWeaverYKConjunctival advancement for late-onset f iltering bleb leaks: Indications and outcomesArch Ophthalmol199911781014101910448743
- LoaneMEGalanopoulosAThe surgical management of leaking filtering blebsCurr Opin Ophthalmol199910212112510537762
- WilsonMRKotas-NeumannRFree conjunctival patch for repair of persistent late bleb leakAm J Ophthalmol199411755695748172260
- SoongHKMeyerRFWolterJRFistula excision and peripheral grafts in the treatment of persistent limbal wound leaksOphthalmology198895131363278258
- MaDHWangSFSuWYTsaiRJAmniotic membrane graft for the management of scleral melting and corneal perforation in recalcitrant infectious scleral and corneoscleral ulcersCornea200221327528311917176
- MelamedSAshkenaziIBelcherDCBlumenthalMDonor scleral graft patching for persistent filtration bleb leakOphthalmic Surg19912231641652030901
- KosminASWishartPKA full-thickness scleral graft for the surgical management of a late filtration bleb leakOphthalmic Surg Lasers19972864614689189949
- ScheinODThe use of processed pericardial tissue in anterior ocular segment reconstructionAm J Ophthalmol199812545495529559742
- BrandtJDPatch grafts of dehydrated cadaveric dura mater for tube-shunt glaucoma surgeryArch Ophthalmol199311110143614398216025
- SoongHKMeyerRFWolterJRFistula excision and peripheral grafts in the treatment of persistent limbal wound leaksOphthalmology198895131363278258
- MistlbergerABiowskiRGrabnerGRepair of a late-onset filtering bleb leak using a corneal graft shaped with an Excimer laserOphthalmic Surg Lasers200132542843111563789
- TiSTanDTHTectonic corneal lamellar grafting for severe scleral melting after pterygium surgeryOphthalmology200311061126113612799236