Abstract
Purpose:
To compare the kinetics and speed of kill of Streptococcus pneumoniae and Haemophilus influenzae on exposure to three topical ophthalmic antibiotic solutions.
Materials and methods:
Bacterial conjunctivitis isolates of S. pneumoniae and H. influenzae were exposed to 1:1000 dilutions of moxifloxacin 0.5%, tobramycin 0.3%, gentamicin 0.3%, and water (control). At 15, 30, 60, 120, and 180 minutes after exposure, aliquots were collected, cells were cultured, and viable cell counts were determined using standard microbiological methods.
Results:
Moxifloxacin achieved 99.9% kill (3-log reduction) at approximately 2 hours for S. pneumoniae and at 15 minutes for H. influenzae. Tobramycin and gentamicin did not achieve 3-log reduction of S. pneumoniae during the 180-minute study period. An increase in bacterial growth was noted for these isolates. Gentamicin took more than 120 minutes to achieve the 3-log reduction of H. influenzae and tobramycin did not reach the 3-log reduction of this pathogen during the 180-minute study period.
Conclusion:
Moxifloxacin killed S. pneumoniae and H. influenzae in vitro faster than tobramycin and gentamicin, suggesting its potential clinical benefit as a first-line treatment for bacterial conjunctivitis to minimize patient symptoms and to limit the contagiousness of the disease.
Introduction
Conjunctivitis is a common disease, with considerable social and economic consequences due to disruption of usual patient and/or caregiver activities, such as lost days of school and/or work. Conjunctivitis can be caused by many ocular pathogens, but is mainly bacterial or viral in origin, with approximately 78% to 80% of cases being bacterial in origin.Citation1 Bacterial conjunctivitis is particularly common in children, with Streptococcus pneumoniae and Haemophilus influenzae being the most common causative organisms.Citation2 The disease is characterized by mucopurulent discharge, conjunctival injection, and morning matting of the lids.
The optimal treatment of bacterial conjunctivitis has been under debate for years. Opinions range from no treatment at allCitation3 to treatment with new-generation fluoroquinolones. Citation4 Although bacterial conjunctivitis is a self-limited disease lasting 7 to 14 days,Citation2 initial therapy that offers a quick eradication of the causative pathogen is preferred.Citation5 This rapid eradication minimizes contagiousness and allows for quick return to normal daily routines.Citation6 In addition to bactericidal activity, an ophthalmic antibiotic should be safe, cost-effective, and have a favorable dosing regimen.
Aminoglycosides are a group of antibiotics derived from various species of Streptomyces that interfere with the function of bacterial ribosomes. From the early to late 1980s, prior to the use of ophthalmic fluoroquinolones, aminoglycosides were used frequently as a treatment for bacterial conjunctivitis. Included in this group of ocular antibiotics are tobramycin ophthalmic solution 0.3% (Tobrex®; Alcon Laboratories, Inc., Fort Worth, TX, USA) and gentamicin ophthalmic solution 0.3% (Genoptic®; Allergan, Inc., Irvine, CA, USA). The decreasing use of aminoglycosides is a result of the increasing resistance of Gram-positive organisms to this class of antibiotics and the increasing incidence of adverse ocular reactions.Citation7–Citation9 Since the 1990s, fluoroquinolones have gained widespread acceptance in the treatment of bacterial conjunctivitis because of the speed with which they eradicate bacteria. Fourth-generation fluoroquinolones provide the best coverage against Gram-positive organisms, including resistant strains, while maintaining coverage against Gram-negative organisms comparable to the earlier fluoroquinolones.Citation10,Citation11
Despite the advantages of topical fluoroquinolones, clinicians have had some reservations regarding their use. Some have been concerned with speculative side effects, which may be attributed to side effects based on product labeling for systemic use. Some believe the use of topical fourth-generation fluoroquinolone antibiotics would lead to erosion of their clinical effectiveness to a greater degree than if the newer antibiotics were held in reserve and used only for patients who did not respond to initial therapy.Citation4 Results from in vitro studies indicate that resistance to fourth-generation fluoroquinolones develops via multiple-step mutations.Citation12 Therefore, fourth-generation fluoroquinolones maintain their clinical effectiveness because the probabilities of development of resistant strains in this class are much reduced. Additionally, clinicians may be less likely to prescribe newer antibiotics because of the perceived increase in cost,Citation6 despite the more rapid kill, which can minimize the duration of symptoms and decrease contagion.
Moxifloxacin ophthalmic solution 0.5% (Vigamox®; Alcon Laboratories, Inc.) is a fourth-generation, 8-methoxy fluoroquinolone with a diazabicyclononyl ring at C7 position. The antibacterial action of moxifloxacin results from inhibition of the DNA gyrase and topoisomerase IV,Citation13,Citation14 whereas earlier-generation fluoroquinolones inhibited either DNA gyrase or topoisomerase IV. Moreover, the mechanism of action of the fourth-generation fluoroquinolones is different from that of macrolides, aminoglycosides, or tetracyclines, allowing moxifloxacin to be active against organisms that are resistant to these antibiotics.
The purpose of this study was to compare the time required in vitro for tobramycin and gentamicin (aminoglycosides) and moxifloxacin (fourth-generation fluoroquinolone) to kill S. pneumoniae and H. influenzae, the most common causative organisms of bacterial conjunctivitis in children.
Materials and methods
Bacterial isolates of S. pneumoniae and H. influenzae were isolated from patients who had bacterial conjunctivitis. Minimum inhibitory concentrations (MIC) of these two isolates for selected antibiotics were determined by broth micro dilution methods recommended by the National Committee for Clinical Laboratory Standards (NCCLS).
Kinetics of kill testing was used to compare the rates of kill of S. pneumoniae and H. influenzae by three ophthalmic products developed to topically treat bacterial conjunctivitis: moxifloxacin ophthalmic solution 0.5%, tobramycin ophthalmic solution 0.3%, and gentamicin ophthalmic solution 0.3%. Each product was tested at a 1:1000 dilution to approximate the concentrations remaining in the tear film 30 to 60 minutes after antibiotic instillation in the eye.Citation4
S. pneumoniae growing logarithmically at 35 °C in cationadjusted Mueller-Hinton broth and H. influenzae growing logarithmically in Haemophilus Test Media broth were exposed to the diluted ophthalmic antibiotic products. At 15, 30, 60 minutes after exposure, aliquots of treated cells were withdrawn and serially diluted in cold phosphate-buffered saline with peptone. Aliquots containing S. pneumoniae (0.1 mL each) were spread onto trypticase soy agar plates supplemented with 5% sheep blood to determine the number of surviving colony-forming units per mL (CFU/mL). Likewise, 0.1 mL aliquots containing H. influenzae were spread onto chocolate agar plates. Plates were incubated at 35 °C for 24 hours and viable cell count was determined using standard methods.
Results
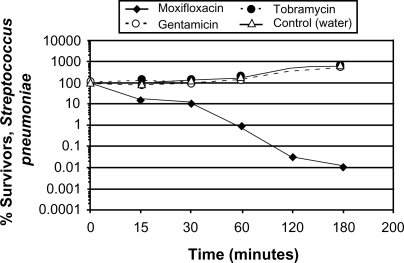
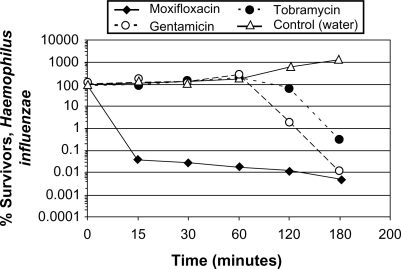
Kinetics of kill studies of moxifloxacin, tobramycin, and gentamicin were conducted with S. pneumoniae (MCC 40211) and H. influenzae (MCC 95018). The MIC susceptibility profiles of these isolates to selected antibiotics are presented in , which is similar to profiles previously reported in the literature.Citation4,Citation6,Citation15 The kinetics of kill data for the two isolates are presented in and as percent survivors from initial CFU/mL.
Table 1 Minimum inhibitory concentration (μg/mL) of Streptococcus pneumoniae and Haemophilus influenzae isolates to selected antibiotics
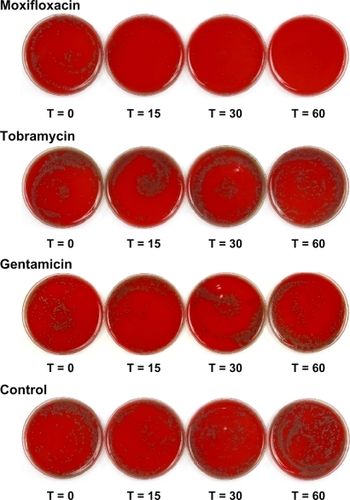
Streptococcus pneumoniae
Use of 1:1000 dilution of moxifloxacin 0.5% (5 μg/mL) for S. pneumoniae resulted in a 99% reduction in the percentage of surviving CFU within 60 minutes of exposure and 99.9% reduction (3-log reduction) in the percentage of surviving CFU within 120 minutes of exposure. 1:1000 dilutions of tobramycin 0.3% (3 μg/mL) and gentamicin 0.3% (3 μg/mL) showed an increase in bacterial growth over the 180-minute study period (). Plate photographs showed that moxifloxacin achieved almost complete eradication of bacterial growth 60 minutes after exposure, whereas tobramycin and gentamicin showed an increased bacterial growth at 60 minutes when compared with baseline (Time 0) ().
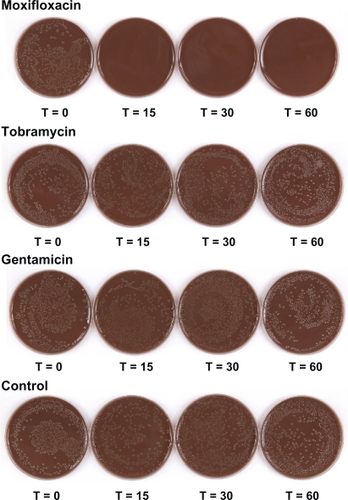
Haemophilus influenzae
Use of 1:1000 dilution of moxifloxacin 0.5% (5 μg/mL) for H. influenzae resulted in a greater than 99.9% reduction in the percentage of surviving CFU within 15 minutes of exposure (). 1:1000 dilutions of both tobramycin 0.3% (3 μg/mL) and gentamicin 0.3% (3 μg/mL) showed an increase in bacterial growth during the first 60 minutes of the study period. Gentamicin achieved a 3-log reduction of viable cell counts within 180 minutes of exposure, whereas tobramycin did not achieve the 3-log reduction during the 180-minute study period. Plate photographs showed that moxifloxacin achieved almost complete eradication of bacterial growth within 15 minutes after exposure, whereas tobramycin and gentamicin showed an increased bacterial growth at 60 minutes when compared with baseline (Time 0) ().
Discussion
The most appropriate antibiotic therapy for patients with contagious bacterial conjunctivitis should eliminate infection quickly to minimize both the signs and symptoms and the spread of the disease. The antibiotic also should be safe, well-tolerated, have a convenient dosing regimen to encourage adherence, and be cost-effective.Citation16
The economic burden of bacterial conjunctivitis is substantial and involves both direct and indirect costs. The direct costs of treating patients with bacterial conjunctivitis in the United States was estimated at approximately $765 million in 2005.Citation17 Currently, there is no consensus among state health officials regarding students’ absence(s) due to bacterial conjunctivitis. The issue of whether or not to require a child’s absence from school if the student is found to have bacterial conjunctivitis has to do with more than just the likelihood that the child will infect others. Students’ absenteeism affects their academic performance, the schools’ State and Federal funding, and employers’ productivity due to lost work time by parents or caregivers.Citation5 It is estimated, depending on the state and the school district, that schools lose approximately $32 to $42 of State and/or Federal funding per student per missed school day (excused or unexcused).Citation18,Citation19 The 2009 United States Department of Labor’s Wage and Hour Division (WHD) federal minimum wage laws indicate that a minimum-wage earning parent or caregiver who loses one working day to care for a child with bacterial conjunctivitis loses between $41.20 and $68.4 in wages, depending on the minimum wage set by the state.Citation20 Therefore, the cost-effectiveness of an antibiotic, not simply the unit price, is an important measure that allows clinicians to choose the ideal antibiotics.Citation5
This current study investigated the kinetics of kill of moxifloxacin 0.5%, a commonly prescribed fourth-generation fluoroquinolone antibiotic, and two aminoglycoside antibiotics (tobramycin and gentamicin) on S. pneumoniae and H. influenzae, the two most commonly isolated organisms in bacterial conjunctivitis in children.Citation2 The antibiotics were diluted 1:1000 to represent the concentration of the antibiotic in the eye 30 to 60 minutes after instillation.Citation4 Moxifloxacin demonstrated a more rapid bacterial kill than either one of the aminoglycosides, achieving 99.9% kill (bactericidal effect) of S. pneumoniae within 120 minutes of exposure and 99.9% kill of H. influenzae within 15 minutes of exposure. Aminoglycosides did not kill S. pneumoniae during the 180-minute study period, and their speed of bacterial kill of H. influenzae was much slower than that of moxifloxacin. Similar kinetics of kill studies conducted separately against H. influenzae with moxifloxacin ophthalmic solution 0.5% and fusithalmic acid 1.0% demonstrated similar results (data not shown). Moxifloxacin eradicated H. influenzae within 15 minutes while fusithalmic acid was unable to kill the bacteria during the 60-minute study period. Collectively, the findings from these in vitro studies suggest that moxifloxacin might eradicate rapidly S. pneumoniae and H. influenzae in patients with bacterial conjunctivitis, possibly translating into faster symptom resolutionCitation5,Citation21 and a reduced chance of disease transmission. This may lead to a decrease in the number of days needed to achieve resolution of symptoms and the economic benefits of a reduction in the rate of school absenteeism by affected children and in the loss of work days by parents and/or caregivers.
There are some limitations to in vitro kinetics of kill studies. First, these studies report results based on a constant concentration of active product rather than the changing concentrations that are expected in the eye after instillation of the antibiotic. Second, kinetics of kill studies are conducted after a single exposure to antibiotics; therefore, the application of this model for bacteria exposed to multiple daily doses of antibiotic is unknown. For these reasons, results of in vitro kinetics of kill studies should be confirmed in clinical studies, although few comparative clinical studies are available. Granet et alCitation5 demonstrated that moxifloxacin 0.5% dosed 3 times daily cured bacterial conjunctivitis faster and more effectively than polymyxin B sulfate/trimethoprim dosed 4 times daily, with H. influenzae being the most commonly isolated organism in that study.
Conclusion
Kinetics of kill studies with moxifloxacin ophthalmic solution 0.5% support a greater speed of kill against S. pneumoniae and H. influenzae than with the aminoglycosides, tobramycin ophthalmic solution 0.3% and gentamicin ophthalmic solution 0.3%. Rapid bacterial eradication of pathogenic bacteria is a favorable characteristic of an antibiotic because it minimizes the spread of the disease and provides quicker clinical resolution, of which have tremendous socioeconomic impact on children and their families.
Acknowledgements
The study was conducted at Alcon Research, Ltd., Fort Worth, TX, USA.
Editorial assistance in the preparation of this manuscript was provided by Heba Costandy, MD, MS, of H H Consulting, Inc. Support for this assistance was provided by Alcon Research, Ltd.
Disclosures
Jamison T, Dajcs JJ, Gross RD, and Cockrum P are employees of Alcon Research, Ltd. and Drs Wagner, Granet, and Lichtenstein are consultants for Alcon Research, Ltd. None of the authors has any proprietary or financial interest in moxifloxacin, tobramycin or gentamicin.
References
- GigliottiFWilliamsWTHaydenFGHendleyJOBenjaminJDickensMEtiology of acute conjunctivitis in childrenJ Pediatr19819845315366970802
- WeissABrinserJHNazar-StewartVAcute conjunctivitis in childhoodJ Pediatr1993122110148419593
- RosePWHarndenABrueggemannABPereraRSheikhACrookDChloramphenicol treatment for acute infective conjunctivitis in children in primary care: a randomised double-blind placebo-controlled trialLancet2005669479374315993231
- LichtensteinSJDorfmanMKennedyRStromanDControlling contagious bacterial conjunctivitisJ Pediatr Ophthalmol Strabismus2006431192616491721
- GranetDBDorfmanMStromanDCockrumPA multicenter comparison of polymyxin B sulfate/trimethoprim ophthalmic solution and moxifloxacin in the speed of clinical efficacy for the treatment of bacterial conjunctivitisJ Pediatr Ophthalmol Strabismus200845634034919043945
- LichtensteinSJWagnerRSJamisonTBellBStromanDWSpeed of bacterial kill with a fluoroquinolone compared with nonfluoroquinolones: clinical implications and a review of kinetics of kill studiesAdv Ther20072451098111118029337
- NorrbySREmerging antibiotic resistance in gram positive bacteria: return to the preantibiotic era?Hong Kong Med J19951129135
- AndersonRJKimbroughRLennonKAdverse drug reactions: ocular sensitivity reaction to neomycinJ Pharm Pract199692vvii
- Ophthalmic moxifloxacin (vigamox) and gatifloxacin (zymar)The Medical Letter20044611792527
- AldridgeKEAshcraftDSComparison of the in vitro activities of Bay 12-8039, a new quinolone, and other antimicrobials against clinically important anaerobesAntimicrob Agents Chemother19974137097119056020
- WoodcockJMAndrewsJMBoswellFJBrenwaldNPWiseRIn vitro activity of BAY 12–8039, a new fluoroquinoloneAntimicrob Agents Chemother19974111011068980763
- Alcon Laboratories Inc. Vigamox (moxifloxacin hydrochloride ophthalmic solution) 0.5%. [Package insert] 2008.
- OgawaGSHyndiukRAThe fluoroquinolones: new antibiotics in ophthalmologyInt Ophthalmol Clin199333459688258498
- DrlicaKMechanism of fluoroquinolone actionCurr Opin Microbiol19992550450810508721
- AsbellPAColbyKADengSMcDonnellPMeislerDMRaizmanMBOcular TRUST: nationwide antimicrobial susceptibility patterns in ocular isolatesAm J Ophthalmol2008145695195818374299
- KowalskiRPYatesKARomanowskiEGKarenchakLMMahFSGordonYJAn ophthalmologist’s guide to understanding antibiotic susceptibility and minimum inhibitory concentration dataOphthalmology200511211198716183128
- SmithAFWaycasterCThe annual cost of bacterial conjunctivitis in the United States: Evidence from an economic modeling approach13th Annual ISPOR Meeting2008May 3–7Toronto, CanadaValue in Health 2008113A291
- Pupil Accounting. San Diego Unified School District. Available from: http://www.sandi.net/pupil_acct/ Accessed November 19, 2009.
- Big plans on campus. Business Week, Fall 2004. Available from: http://www.businessweek.com/magazine/content/04_44/b3906650.htm Accessed November 19, 2009.
- Minimum wage laws in the states. United States Department of Labor’s Wage and Hour Division (WHD), July 24, 2009. Available from: http://www.dol.gov/esa/minwage/america.htm#Texas Accessed August 31, 2009.
- MatherRKarenchakLMRomanowskiEGKowalskiRPFourth generation fluoroquinolones: new weapons in the arsenal of ophthalmic antibioticsAm J Ophthalmol2002133446346611931779