Abstract
Objectives:
To evaluate success rates in the correction of astigmatism with toric and spherical soft contact lens fitting.
Methods:
30 patients with soft toric lenses having more than 1.25 D of corneal astigmatism (25 eyes; Group A) or having 0.75–1.25 D of corneal astigmatism (22 eyes; Group B) and 30 patients with soft spheric lenses having 0.75–1.25 D of corneal astigmatism (28 eyes; Group C) or less than 0.75 D of corneal astigmatism (23 eyes; Group D) were included in the study. Corrected and uncorrected monocular visual acuity measurement with logMAR, biomicroscopic properties, autorefractometry and corneal topography were performed for all patients immediately before and at least 20 minutes after the application of contact lenses. Success of contact lens fitting was evaluated by three parameters: astigmatic neutralization, visual success, and retinal deviation.
Results:
After soft toric lens application, spheric dioptres, cylindric and keratometric astigmatism, and retinal deviation decreased significantly in Groups A and B (P < 0.05). In Group C, spheric dioptres and retinal deviation decreased (P < 0.05), while cylindric and keratometric astigmatism did not change significantly (P > 0.05). In Group D, spheric dioptres, retinal deviation, and cylindric astigmatism decreased (P < 0.05). Keratometric astigmatism did not change significantly (P > 0.05) and astigmatic neutralization even increased.
Conclusions:
Visual acuity and residual spherical equivalent refraction remained between tolerable limits with the use of toric and spheric contact lenses. Spherical lenses failed to mask corneal toricity during topography, while toric lenses caused central neutralization and decrease in corneal cylinder in low and moderate astigmatic eyes.
Introduction
The goal of soft contact lens application is to achieve excellent vision with overall lens comfort. Astigmats represent approximately one-third of potential contact lens wearers. The proportion of toric soft lenses prescribed has been much lower than this.Citation1,Citation2 For astigmatic eyes, soft spheric (42.5%), soft toric (21.9%), and rigid gas permeable (35.6%) lenses have been preferred in the previous studies.Citation3 Morgan et al have reported a doubling in the use of toric soft lenses to 27% of new fits over a five year period In the UK.Citation4
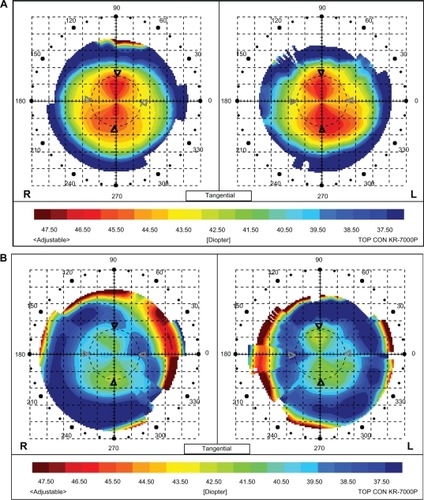
Figure 1 Spheric, cylindric, keratometric and retinal deviation mean values in diopters according to the groups before contact lens application.
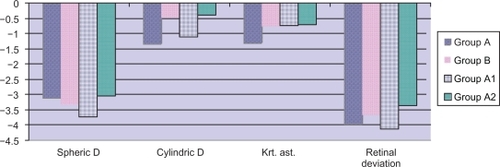
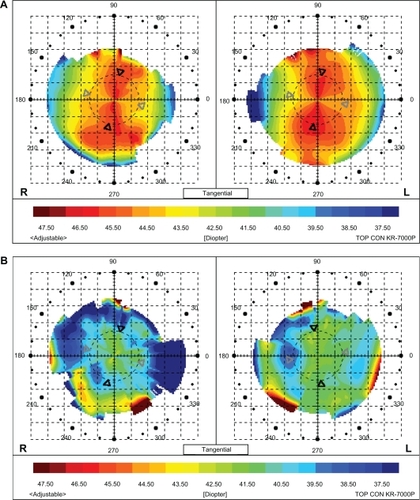
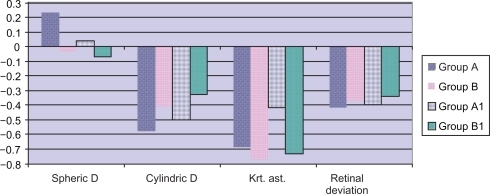
Figure 2 Spheric, cylindric, keratometric and retinal deviation mean values in diopters according to the groups after contact lens application.
Soft spheric contact lenses with uniform thickness will contour the corneal astigmatism, resulting in an astigmatic front surface of the soft contact lens. Contact lens thickness can affect lens flexure and astigmatic neutralization. Central thicknesses of the lenses used today are considered to have insignificant resistance to bending.Citation5 To correct corneal astigmatism, toric soft contact lenses with non-uniform thickness profiles are designed and produced using different techniques.Citation6,Citation7
There have been many developments in toric lens technology and modeling, giving clinicians the advantages of larger parameter ranges, frequent displacement, and improved clinical performance. No significant differences have been observed with respect to contrast sensitivity thresholds, Snellen acuity thresholds, or subjective preferences between spectacles and toric hydrogel lenses.Citation8 Disposable toric contact lenses provide good visual acuity and are considered to be appropriate for correcting astigmatism.Citation9 Nevertheless, a recent wearer survey showed the high levels of lens performance expected by toric lens wearers were not being achieved, especially when comparing comfort and vision ratings.Citation10
Adaptation to corneal astigmatism depends on the ratio of astigmatism to the total refractive error. However, tolerance of astigmatism may increase in correlation with the increased spheric error.Citation6 A question in correcting spherocylindric refractive error with soft toric and soft spheric lenses is whether the increase in visual acuity is due to the neutralisation of refraction, or that the higher tolerance of patients is making us think that we are successful. Theoretically, soft toric lenses should totally neutralise the corneal astigmatism, while spheric soft lenses may partially neutralize it, mainly because of the thickness of these lenses. Since topographic maps may show changes on the front surface of a soft contact lens, corneal topography may be beneficial in assessing the degree of effectiveness of spherical and toric contact lenses.
In our study, the purpose was to determine how successful we are in correcting spherocylindric refractive errors with soft toric and spheric lenses by objective and subjective criteria, and to compare these two types of lenses in low and moderate astigmatic cases.
Materials and methods
30 patients with soft toric lenses having more than 1.25 D of corneal astigmatism (25 eyes; Group A) or having 0.75–1.25 D of corneal astigmatism (22 eyes; Group B) and 30 patients with soft spheric lenses having 0.75–1.25 D of corneal astigmatism (28 eyes; Group C) or less than 0.75 D of corneal astigmatism (23 eyes; Group D) were included in the study. Specifications of the toric and spherical contact lenses used are summarized in .
Table 1 Specifications of toric and spherical contact lenses
Patients willing to use contact lenses were chosen and those having ocular surface diseases or functional deficit of the tear film were excluded. Written, informed consent was provided from the patients. Corrected and uncorrected monocular visual acuity measurement with logMAR, biomicroscopic properties, autorefractometry and corneal topography with a placido disk-based corneal mapping system, transferring data to color mapping software measurements (Topcon KR 7000P, Topcon Corporation, Tokyo, Japan) were performed for all patients immediately before and at least 20 minutes after the application of contact lenses.
Optimum fitting for corneal coverage, horizontal and vertical centration and movement was achieved, as suggested by Young,Citation11 using spherical lenses fitted to the mean spherical equivalent prescription. The scribe marks on the toric soft lenses were located between 0–10° from the lens marking location after lens settling.
During the biomicroscopic evaluation, centralization, axial rotation, and deposits on the contact lenses were noted. The orientation of the lens was assessed with the slit lamp and the rotations were recorded with reference to lazer markings.
Success of contact lens fitting was evaluated by three parameters:
Astigmatic neutralization: In order to compare the effective neutralization of different diopters of corneal astigmatism, residual astigmatism after contact lens application was divided by the initial or total corneal astigmatism determined before contact lens application, and expressed as a percentage using the the following formula: residual/total cylinder %.
Visual success: Visual acuity, corrected with contact lenses and glasses in logMAR, was compared. Difference in visual acuity less than 2.0 lines was accepted as successful application, and the success rate was determined subjectively.
Mean retinal deviation (absolute spherical equivalent fraction): To simplify the combined effect of spheric and cylindirical power, residual refractive errors of the patients based on autorefractometry were formulated as described by Poyor et al.Citation12 Deviation was calculated by taking the mean of the absolute values of the principal meridians in diopters. Axial rotation was not taken into consideration.
Mean retinal deviation values were calculated for each of the groups before and after contact lens application and termed “total” and “residual” retinal deviations respectively. Residual retinal deviation values less than 0.50 D were accepted as successful. Success rates were evaluated for each group by defining the (individual) residual/total retinal deviation value ratio for each case.
Statistical analysis
The data were entered into a Microsoft® Excel® spreadsheet and analyzed using SPSS (version 15.0) statistical software. Measures of central tendencies, including means, standard deviations, and ranges were calculated by descriptive analysis. A repeated measure analysis of variance (ANOVA), paired samples test, and appropriate post hoc t-test comparisons were performed using the method described by Tukey. The appropriate mean square error from the analysis of variance, P < 0.05, was accepted as statistically significant.
Results
98 eyes of 60 patients were included in the study. Mean age was 25.9 years (± 8.4) in Group A, 29.4 years (± 8.7) in Group B, 25.07 years (±4.5) in Group C, 23.3 years (± 5.5) in Group D (P = 0.712). The female/male ratio was 15/10 in Group A, 12/10 in Group B, 15/13 in Group C, and 14/9 in Group D.
A summary of mean baseline spectacle spheric power and mean cylinder and keratometric astigmatism is presented in . Total mean retinal deviations were 3.27 D (±3.24) in Group A, 4.37 D (±3.0) in Group B, 3.52 D (±2.2) in Group C, and 3.30 D (±1.7) in Group D (P = 0.458).
Table 2 Spectacle spheric, cylindric, keratometric and retinal deviation mean values in diopters according to the groups before contact lens application
Mean spheric, cylindric and keratometric values in diopters according to the groups measured over contact lenses, after contact lens application are presented in .
Table 3 Spheric, cylindric, keratometric and retinal deviation mean values in diopters, astigmatic neutralization and visual acuity (Snellen lines) according to the groups after contact lens application
The average percent corneal astigmatic neutralization from the contact lenses were −52% (±28%) in Group A, −53% (±26%) in Group B, −94% (±25%) in Group C, and 126% (±16%) in Group D (P = 0.000). The minus sign represents a decrease in the contact lens surface cylinder compared with the original corneal surface power.
Means of the visual acuities corrected with glasses were 0.02 logMAR (±0.04) in Group A, 0.005 logMAR (±0.002) in Group B, 0.0 logMAR (±0.0) in Group C, and 0.0 log-MAR (±0.0) in Group D (P = 0.065). Means of the visual acuities corrected with contact lenses were 0.02 logMAR (±0.01) in Group A, 0.025 logMAR (±0.04) in Group B, 0.015 logMAR (±0.01) in Group C, and 0.0 logMAR (±0.0) in Group D (P = 0.106).
Residual mean retinal deviations after contact lens fitting were 0.04 D (±0.40) in Group A, 0.11 D (±0.53) in Group B, 0.26 D (±0.43) in Group C, and 0.20 D (±0.25) in Group D (P = 0.240). The average of the ratios of residual/total mean retinal deviation was: 0.25 D (±0.34) in Group A, 0.17 D (±0.21) in Group B, 0.12D (±0.07) in Group C, and 0.18 (±0.41) in Group D (P = 0.415).
During the statistical analysis, after soft toric lens application, spheric dioptres, cylindric and keratometric astigmatism, and retinal deviation decreased significantly in Groups A and B (P = 0.0). In Group C, spheric dioptres (P = 0.012) and spherical equivalent refraction (P = 0.0) decreased. While cylindric (P = 0.547) and keratometric (P = 0.286) astigmatism did not change significantly.
In Group D, spheric dioptres and spherical equivalent refraction (P = 0.0) and cylindric astigmatism (P = 0.045) decreased, while keratometric astigmatism (P = 170) did not change significantly, and astigmatic neutralization even increased.
Among the different lens types used, in Groups A, B, and D, we did not observe statistical difference for spheric, cylindric dioptres, keratometric astigmatism, or retinal deviation, while in Group C, we observed significant difference only for the ratios of residual/total mean retinal deviation (P = 0.008).
In our study, less than two rows of spectacle-contact lens difference for visual performance and less than 0.50 D of retinal deviation as objective criteria, were accepted as a successful response. 100% of eyes in Groups A, B, and D and 96% of eyes in Group C had 2.0 or less line loss in visual acuity (P > 0.05). All these patients had low residual mean retinal deviation values (>0.50 D). The percentage of patients having less than 0.50 D of residual retinal deviation was 80% in Group A, 95% in Group B, 78% in Group C, and 95% in Group D ().
Table 4 Visual success and residual retinal deviation success rates according to the groups
When we considered less than one row of spectacle-contact lens difference for visual performance in Groups A, B, C, and D, success percentages were 80%, 100%, 78.2%, and 82% respectively.
When we compared our patients with low astigmatism between 0.75–1.25 D in Groups B and C using toric and spheric lenses respectively, we observed significant difference in residual corneal astigmatism (P = 0.005) and astigmatic neutralization (P = 0.048). Although not significant statistically, visual success rate (<2 line loss) was lower in Group C (96%) than Group B (100%) (P = 0.674), and residual retinal deviation success (<0.50 D) was lower in Group C (78%) than Group B (95%) (P = 0.551). The astigmatic neutralization value was 53% (±26%) in Group B and 94% (±25%) in Group C.
The evaluation of topographic data showed that, after toric lens application, the astigmatism on the anterior surface was neutralized and the bow tie appearance was dispersed through the periphery depending on the residual astigmatism in Groups A and B. However, after spheric lens application in Groups C and D, bow tie appearance was projected nearly equally on the anterior surface topography, compared to values obtained before contact lens application (–).
Discussion
The dioptric power of a soft contact lens on the eye is a function of its off-eye power, lens flexion on the eye, lens hydration and corneal topography. Though patient satisfaction and subjective visual data point out important clues, confirming these data more objectively by autorefraction and topography will be useful in our overall evaluation. The success of the fitting technique can be assessed in consideration of manifest refraction with the toric and spheric soft contact lens in situ on the eye. We calculated mean retinal deviation in order to predict loss of visual acuity using residual refractive error. Mean retinal deviation is a geometric optical calculation method that describes the amount of defocus at the plane of the retina and combines the three components of spheric power, cylindric power and axis into a single dioptric measure by taking the mean of the absolute values of the principal meridians. Since this value gives us deviation from the retinal plane; it should not be mixed up with spherical equivalent. Spherical equivalent specifies the mean point between the main meridians instead of retinal deviation. The relationship between visual acuity loss and optical errors was used to predict the effect on visual acuity. This method was previously applied to a sample of 457 Focus® toric soft contact lenses. It found that 83.5 ± 1.7% of the lenses were accurate enough to deliver one line or less of loss in visual acuity.Citation12
There is no appreciable neutralization of corneal astigmatism with spherical soft lenses and, possibly, there is an increase in surface irregularity. A spherical contact lens used for a patient with less than 0.75 D cylinder led to a 21%–24% increase in the contact lens surface cylindrical power compared to the original corneal surface power, while a spherical contact lens applied on a toric cornea led to 89% increase in corneal cylindric value. Toric contact lenses fitted into toric corneas led to a 34%–38% decrease in the corneal cylindric dioptres.Citation13
Flexure of toric hydrogel contact lenses is explained by the Linear Regression Hypothesis, which implies that partial flexure due to different meridians might lead to the minus tear lens formation and residual refractive astigmatism.Citation14 McCarey and co-workers have observed that the toric soft contact lens neutralized the cylinder component 37% by topography and 57% by manifest refraction.Citation13 In this study, our results are in agreement with previous studies: corneal astigmatic neutralization values were −52% (± 28%) to −53% (±26%) for soft toric lenses in Groups A to B and −94% (±25%) to 126% (±16%) for soft spheric lenses in Groups C and D.
The anterior surface of the eye has the largest refractive index in the optical system. When a toric lens is applied, its anterior surface becomes most important refractive surface. Theoretically, soft toric contact lenses are manufactured for neutralization of ocular surface toricity. That is why in situ topographic maps show relatively spheric or equivalent or opposite power anterior surface toricity in residual astigmatism.Citation7,Citation13 Corneal topography is a beneficial method for the objective evaluation of spheric and toric lens behaviour in situ, such as the effect of soft lens flexure on the eye, lid effect, optical quality, and lens cleaning techniques.Citation15 Topographic evaluation is as important as flourescein pattern evaluation in gas permeable contact lenses, as it can also point out manufacturing faults or surface irregularities of lenses. Soft lenses drape the cornea, and keratometry may allow us to check the central bearing area of contact lenses. Significant correlations between toricity of the front surface of the contact lens and that of the cornea has been observed by means of keratometry and photoelectric keratoscopy.Citation16
We used a placido disc-based corneal mapping system and observed that toric lenses caused central neutralization and dispersion of bow tie appearance through the periphery, which led to the formation of an island shape. On the other hand, with soft spheric lenses, the previous bow tie appearance persisted centrally, which implied that the neutralization process was inadequate.
An often-quoted strategy for correcting low degrees of astigmatism with soft lenses is to increase the thickness of the lens or use a higher modulus material, considering that a thicker or stiffer lens may drape less on the cornea and so mask more astigmatism. Hovewer, no significant effect of lens thickness has been reported for the majority of patients.Citation17–Citation19 Research by Cho and WooCitation17 examined whether thicker or thinner lenses provided better acuity with high- and low-contrast logMAR charts. Using lenses that have center thicknesses of 0.06 mm and 0.12 mm, they noted that the thicker lenses provided better acuity, though this difference was not statistically significant. Likewise, a higher modulus spherical silicone hydrogel material has been shown to have no significant impact on the amount of astigmatism masked when compared to a hydrogel soft contact lens.Citation20 In this study, we used spheric hydrogel contact lenses with center thicknesses between 0.08 mm and 0.1 mm, and similar to other reports, lens thickness had no influence on the amount of astigmatism masked.
There remains some disagreement as to when to fit soft toric lenses. Dabkoski et alCitation21 found that low to moderate myopes with low astigmatism (0.75 DC to 1.25 DC) had significantly better acuity with toric lenses than with the spherical equivalent. Richdale et alCitation22 evaluated the acuity of myopic astigmats wearing both soft spherical and toric lenses from four manufacturers. For these patients, whose astigmatism was between −1.25 DC and −2.00 DC, soft torics improved their acuity by about two Snellen lines in both bright and dim light compared to spherical lenses. For low-cylinder patients, the bright light results were more modest, yielding only a few letters more, but in dim light their acuity improved by just over one line. Recently, aspheric soft lenses have been promoted for the correction of low levels of astigmatism. Morgan et alCitation23 evaluated high- and low-contrast acuity with spectacles, aspheric soft lenses and toric soft lenses in patients with refractive astigmatism of −0.75 DC or −1.00 DC. They used variable pupil sizes to simulate different lighting conditions. They found that high-contrast and low-contrast visual acuity are superior with toric soft contact lenses and spectacles versus aspheric soft contact lenses for larger pupils by approximately a half-line or more, which is considered to be clinically significant. Superior vision can be achieved for low astigmatic contact lens wearers using toric soft rather than aspheric soft contact lenses.
In our study, less than two rows of spectacle – contact lens difference for visual performance and less than 0.50 D of retinal deviation, as objective criteria, were accepted as a successful response. For the highly astigmatic Group A (>1.25 D), residual mean retinal deviation success was low (80%), but visual success rates were encouraging (100%) after soft toric lens application.
When we compared our patients with low astigmatism (between 0.75–1.25 D) in Groups B and C using toric and spheric lenses respectively, we observed significant difference in residual corneal astigmatism (P = 0.005) and astigmatic neutralization (P = 0.048), Although not significant statistically, visual success rates (<1 line loss) was lower in Group C (96%) than Group B (100%) (P = 0.674), and residual retinal deviation success (<0.50 D) was lower in Group C (78%) than Group B (95%) (P = 0.551), and astigmatic neutralization value was 53% (±26%) in Group B and 94% (±25%) in Group C.
As a conclusion, in this study, visual acuity and residual retinal deviation remained between tolerable limits with the use of toric and spheric contact lenses. Spherical lenses failed to mask corneal toricity during topography and even increased the corneal astigmatism, even in low astigmatism, while toric lenses caused central neutralization and decrease in corneal cylinder. Toric lenses should be preferred in patients with low astigmatism.
Disclosure
The authors disclose no conflicts of interest.
References
- HoldenBHThe principles and practices of correcting astigmatism with soft contact lensesAst J Optom199558279299
- MorganPEfronNTrends in UK contact lens prescribing 1999Optician199921757004344
- KanpolatAOralDTypes of contact lenses applied in astigmatic casesContactologia2000224245
- MorganPEfronNWoodsCInternational contact lens prescribing in 2004CL Spectrum20052013437
- BennettAGPower changes in soft lenses due to bendingOphthalmic Optician197616939945
- BennetESBlancPRembaMRCorrection of astigmatismHenryVAClinical Manual of Contact LensesPhiledelphiaLippincott Williams & Wilkins2000376390
- McCareyBEAmosCFTopographic evaluation of toric soft contact lens correctionCLAO J1994202612657820924
- HallDKWerdJAEdmondsonWSpectacles and custom toric hydrogel contact lenses: A comparison of visionJAOA19946511783787
- CabreraJVRodriguesJBVision with disposable toric contact lenses and daily wear toric contact lensesOphthalmic Phsiol Opt199816674
- Hickson-CurranSDiasLToric soft contact lenses: Where are we now?Optician200623160411416
- YoungGEvaluation of soft contact lens fitting characteristicsOptom Vis Sci1996732472548728492
- PoyorRERobertsSRSchvallicIDSoft toric lens power accuracy and reproducibilityCLAO J19952131631687586474
- McCareyBEAmosCFTaubLRSurface topography of soft contact lenses for neutralizing corneal astigmatismCLAO J19931921141207710455
- WeissmanBATheoretical optics of toric hydrogel contact lensesAm J Optom Physiol Opt1986635365383740208
- MaedaNKlyceSDSmolekMKHamanoHVideokeratography for quantitative surface analysis of used soft contact lensesJpn J Ophthalmol19974142352399304437
- TomlinsonAContact lens and corneal topography with wear of the SoflensAm J Optom Physiol Opt19765311727734998714
- ChoPCWooGCVision of low astigmats through thick and thin lathe-cut soft contact lensesContact Lens Anterior Eye200124415316016303470
- HarrisMGLauSMaHTuanJDo disposable contact lenses mask astigmatism?Optical Prism19961424446
- BernsteinPRGundelRERosenJSMasking corneal toricity with hydrogels: Does it work?Int Contact Lens Clinic199160728731
- EdmondsonLEdmondsonWIIPriceRMasking astigmatism: Ciba Focus Night and Day vs Focus MonthlyOptom Vis Sci20038012184
- DabkowskiJARoachMPBegleyCGSoft toric versus spherical contact lenses in myopes with low astigmatismInt Contact Lens Clin199219252256
- RichdaleKBerntsenDAMackCJMercheaMMBarrJTVisual acuity with spherical and toric soft contact lenses in low- to moderate-astigmatic eyesOptom Vis Sci2007841096997518049362
- MorganPBEfronSEEfronNHillEAInefficacy of aspheric soft contact lenses for the correction of low levels of astigmatismOptom Vis Sci200582982382816189492