Abstract
Objective:
A prospective descriptive study to assess acceptability and effectiveness of a locally made ready-to-use therapeutic food (RUTF) in HIV-infected chronically sick adults (CSA) with mid-upper-arm circumference (MUAC) <210 mm or pitting edema.
Methods:
Sixty-three wasted AIDS adults were prescribed 500 g representing ~2600 kcal/day of locally made RUTF for three months and routine cotrimoxazole. Weight, height, MUAC, Karnofsky score and morbidity were measured at admission and at monthly intervals. The amount of RUTF intake and acceptability were assessed monthly.
Results:
Ninety-five percent (60/63) of the CSA that were invited to join the study agreed to participate. Mean daily intake in these 60 patients was 300 g/person/day (~1590 Kcal and 40 g of protein). Overall, 73.3% (44/60) gained weight, BMI, and MUAC. The median weight, MUAC and BMI gains after three months were 3.0 kg, 25.4 mm, and 1.1 kg/m2, respectively. The intervention improved the physical activity performance of participants and 78.3% (47/60) regained sufficient strength to walk to the nearest health facility. Mortality at three months was 18.3% (11/60).
Conclusion:
Locally made RUTF was acceptable to patients and was associated with a rapid weight gain and physical activity performance. The intervention is likely to be more cost effective than nutritional support using usual food-aid commodities.
Introduction
In human immunodeficiency virus (HIV)-infected patients, malnutrition is associated with an increased risk of death and studies in industrialized countries have demonstrated that weight loss is a good predictor of both opportunistic infection and death.Citation1–Citation3 Similar results have been reported from developing countries including in patients on highly active antiretroviral therapy (HAART).Citation4–Citation6
In industrialized countries, wasting is an indication of progression to acquired immune deficiency syndrome (AIDS), generally occurring as part of the wasting syndrome and closely correlated with stage of the disease.Citation7 By contrast, analysis of anthropometric data from a high prevalence HIV population in South Africa showed that there was no association between disease stage and nutritional status, suggesting that malnutrition due to food shortage might have played an important role in the occurrence of wasting.Citation8
For the World Health Organization (WHO), the comprehensive care for PLWHA must include nutritional support.Citation9 WHO recommends that symptomatic HIV and AIDS patients to increase their daily energy intake by 50% from the requirements of normal active HIV negative adult of 2430 Kcal for male and 2170 kcal for female but to keep proteins and vitamins and minerals intakes at normal daily requirement.Citation9 Thus, the daily recommended energy and proteins intake for symptomatic PLWHA are 2910 to 3160 kcal and 57 g of proteins for male and 2600 to 2820 kcal and 48 g of proteins for female to just maintain weight.Citation10 The most widespread nutrition intervention for HIV-positive adults in developing countries consists of nutrition counseling and the distribution of corn soy blend (CSB; a blended flour) and vegetable oil. However, a study in Malawi indicates that this type of support does little to improve the nutritional status or the survival of HIV-infected people.Citation11 By contrast, data does exist showing the effectiveness in HIV-positive malnourished children of ready-to-use therapeutic food (RUTF).Citation12
The pilot program described in this paper aimed at assessing the effectiveness of RUTF made out of local crops without the addition of milk powder, for the nutritional support of sick HIV-positive adults in Malawi.
Methods
Subjects
The research was conducted in the central region of Malawi from May 2005 to October 2005 in collaboration with SASO (Salima AIDS Support Organization) and NASO (Nkhotakota AIDS Support Organization), home-based care organizations (HBC).
People already receiving care from the NASO and SASO HBC programs were eligible for enrolment in the study. Entry criteria were a middle-upper-arm circumference (MUAC) below 210 mm, a body mass index (BMI) below 17 kg/m2, bilateral pitting edema of the feet or legs or bedridden for >50% of the daytime for more than one month. Exclusion criteria were confirmed HIV-negative, long term physical disability and inability to eat.
Protocols
Possible candidates identified by the volunteers were visited by the HBC supervisors and the study research team, who confirmed eligibility, explained the study objectives and procedures and presented a consent form for signing if willing to participate. At admission, MUAC, weight, height, presence of bilateral edema and physical activity performance using the Karnofsky score were assessed.Citation13 A brief medical history and physical examination was conducted to assess the WHO clinical HIV stage and identify existing morbidity. In those subjects who agreed to have capillary blood taken (n = 51), hemoglobin and CD4 count were measured using a portable hemoglobin meter (hemoCue AB, Angelholm, Sweden) and immunophenotyping (EPICS or FACS count Machine), respectively. All subjects were followed up monthly.
Dietary and medical treatment
Subjects received two pots (500 g) of chickpea sesame-based RUTF (CS-RUTF) providing 2600 kilocalories, 61.5 g of proteins and >1 recommended dietary intake (RDI) for all the vitamins and minerals per day for three months (). The composition in vitamins and minerals was based on WHO specifications for RUTF.Citation14 In addition, 960 mg daily prophylaxis dose of cotrimoxazole was provided along with treatment for minor diseases. More severe medical conditions were referred to the HBC clinic or district hospital.
Table 1 CS-RUTF composition and content and comparison of prescribed amount and the recommended daily intake
Data collection and analysis
At admission and during follow up visits, RUTF intake and acceptability, patient complaints, signs and symptoms of disease and nutritional status were assessed. The acceptability of the CS-RUTF was determined through discussion with patients and caretakers. Intake of RUTF was determined by counting the number of finished pots.
Patient information was recorded on individual cards and entered into a database using Epi Info version 6 (Centers for Disease Control and Prevention, Atlanta, GA). Analyses were performed using SPSS version 12 (SPSS Inc., Chicago, IL). The outcomes of interest were: MUAC, weight, BMI, and physical activity performance changes. MUAC, BMI, and weight change were calculated by subtracting the value at admission from the value at one, two, and three months of treatment. Physical activity performance changes were based on the Karnofsky score (KS)Citation13 that we used to define four categories of physical activity performance and ability to accomplish activities of daily living. These categories were: able to carry out all pre-disease activities (KS >= 80%); restricted in strenuous activity but ambulatory and able to care for self (KS of 70%); very reduced activity, inability to walk long distances or to carry out normal activity but able to care for self (KS of 60% or 50%); disabled, bedridden and requires considerable amount of assistance (KS ≤ 40%).
Quantitative data for normally distributed variables were described using means and standard deviation (SD) and compared using Student’s t-test; nonnormally distributed variables were described using median and inter-quartile range (IQR) and compared using the Kruskall–Wallis test. The association between weight, MUAC, BMI gains, and total RUTF intake were explored using the bivariate correlation analysis (Pearson correlation) with stepwise multivariate linear regression analysis used to explore the independence of the relationships. The predictors for the multivariate models were selected from a pool of pre-chosen potential predictors that included sex (potential influence of energy differences in requirements and expenditure), Weight, MUAC, and BMI of admission (the extend of weight gain is usually related to the initial deficit of body mass), presence of edema (as edema could influence mortality and also minimize weight gain even when using lowest weight) and the morbidity during treatment (as diseases can interfere with utilization of nutrients and increase energy expenditure). Many other variables were tested and retained in the models if they helped in the reduction of the residual variance. The Wilcoxon test and McNemar test for paired samples were used in the analysis of change in physical activity performance.
Results
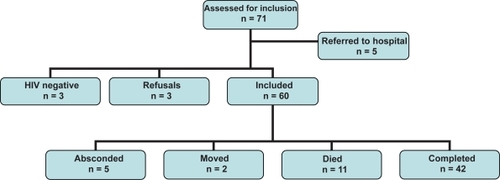
One hundred twenty HBC patients selected by volunteers were assessed for the program and 71 of these met criteria for admission. Out of the 71, five were moribund and excluded from the study (see ). Of the 66 remaining, 63 (95.5%) agreed to participate. Two refused to join the program because of fear of stigmatization and one on the advice of a traditional healer. Three of those who started to take RUTF were later confirmed as HIV-negative, leaving a total of 60 for the study analysis.
Description of subjects
The median age of the patients was 37.7 years (29.7–44) and 63.3% (38/60) of them were female. Clinically, 75% (45/60) had WHO HIV stage 4% and 25% HIV stage 3, but HIV infection was confirmed serologically at the time of inclusion in only 55% (33/60). 100% had reduced physical activity performance (). 26.7% (16/60) had commenced cotrimoxazole prophylaxis at the time of admission, and 13.3% (8/60) had started antiretroviral (ARV) therapy with a combination of stavudine, lamivudine, and nevirapine. These eight patients had been on ARV for one to two months prior to inclusion in the study (). At admission, the overall average weight was 41.6 (7.3) kg, 23.3% (14/60) of patients had edema, 78.3% (47/60) had a MUAC of less than 210 mm (overall mean ± SD of 195.0 ± 18.8 mm), 69% (40/58) had a BMI of less than 17 kg/m2 (overall mean ± SD of 16.1 ± 1.7 kg/m2) and 50% (29/58) a BMI less than 16 kg/m2. Medical complaints at admission were dominated by fever, but diarrhea, oral candidiasis and dermatitis were also common (). The mean hemoglobin was 9.3 (1.8) g/dl and the median CD4 count was 182 (54–310) cells/μl. Patients already on ARVs at admission had lower average weight [35.9 (3.9) kg for those on ARV versus 42.4 (7.3) kg for those not on ARVs; p = 0.017], lower average MUAC [184.1 (22.7) mm for those on ARVs compared to 196.7 (17.8) mm for those not on ARVs; p = 0.79] and lower average BMI [14.9 (1.4) kg/m2 for those on ARV compared to 16.3 (1.6) kg/m2 for those not on ARVs; p = 0.26] than those not yet on ARVs. The mean age, the sex distribution, the mean hemoglobin, the mean CD4 count, the proportion of those with edema and the proportions of bedridden of those on ARVS at admission were not different to that of those not on ARVs (data not shown).
Table 2 Characteristics and condition of patients at admission into the program
Morbidity and mortality during follow-up
Seventy percent (42/60) completed the program, 3.3% (2/60) moved from the area, 8.3% (5/60) defaulted, and 18.3% (11/60) died within the three months of follow-up with a median (IQR) time to death of 46 days (22–70). Two deaths occurred in patients already nutritionally stabilized and who had resumed normal activity. During the three months of follow up, 37 of 55 patients (67.3%) reported or presented at least once with a new episode of diarrhea, fever, cough, oral thrush, headache, or abdominal pain.
RUTF intake and impact on nutrition status
The median (IQR) daily intake of RUTF amongst the subjects included in the program was 300 (150–400) g/person/day (1,590 kcal and ~40 g protein per/person/day). Overall, 73.3% (44/60) gained weight and BMI during the intervention. The median (IQR) of weight, MUAC, and BMI gain were 2.5 (0.4–6.0) kg, 15 (0.0–28.0) mm, and 0.8 (−0.2–1.8), respectively. The weight gain (SD) per 1000 kcal provided was 19.1 (86.9) g (n = 54).
The total RUTF intake predicted the MUAC, weight and BMI changes () (Pearson correlation coefficient = 0.503 (p < 0.001), 0481 (p < 0.001) and 0.458 (p = 0.001), respectively). RUTF intake was independently and positively associated with change in MUAC, weight, and BMI in multivariate models that adjusted for sex, admission characteristics (including MUAC, BMI, bilateral pitting edema, Karnofsky score, HIV clinical stage, and presence of diarrhea) and morbidity encountered during the program (nausea, abdominal pain, cough, headache, diarrhea, and fever) (). The models indicate that commencing ARV triple therapy prior to entering the program or whilst in the program also positively affected MUAC, weight, and BMI gains. Headache and cough during the three months of the program reduced weight gain. The multivariate models explained 37.9%, 52.8%, and 52.8% of the variability of the change in MUAC, weight, and BMI, respectively ().
Figure 2a–c Association between anthropometric change and RUTF intake
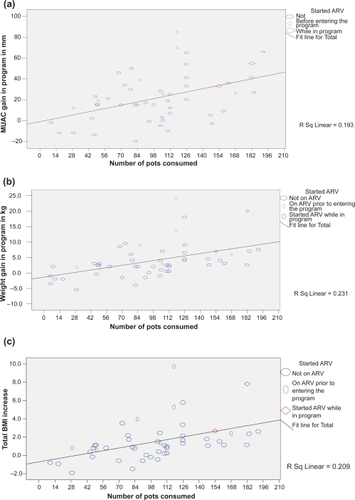
Table 3 Association between anthropometric changes and total RUTF intake
Impact on physical activity performance
The proportion of patients able to walk to the clinic increased from 41.7% (25/60) at admission to 78.3% (47/60) at three months (p < 0.001). Overall, the intervention improved the Karnofsky score of 73.3% (44/60) of participants with 36.7% (22/60) improving by one category, 26.7% (16/60) improving by two categories, and 10.0% (6/60) improving by three categories. 80.1% (34/42) of the subjects who completed the three months of intervention had a Karnofsky score >80%, allowing them to resume their previous activities. 9.5% (4/42) still required external assistance for their personal care. Out of the 25 patients bedridden at admission who completed the three-month study, 88% (22/25) were able to resume their normal activity before commencing ART while 12% (3/22) were still bedridden.
Discussion
Acceptability of RUTF
These results indicate that locally made CS-RUTF was acceptable to HIV-positive patients. Although, some patients linked gastrointestinal symptoms to CS-RUTF intake, these symptoms did not influence the intake of CS-RUTF. This finding suggests that these symptoms were minor or that patients were encouraged to overcome them because of the improvement of their health status as a result of the CS-RUTF intervention. Also, the symptoms reported by the participants are common in HBC patients and tend to reoccur.Citation15
Effectiveness
CS-RUTF intake was associated with a considerable improvement in physical activity performance and nutritional status. The high degree of impact demonstrated in this study stands in marked contrast to other intervention studies that have examined the impact of traditional food aid commodities on nutritional status and survival amongst chronically sick adults. An observational before and after study carried out at Bangwe (Malawi) that provided a monthly ration of 7.5 kg of CSB, 50 kg of maize floor, 5 kg of beans ± 4 liters of fortified vegetable oil for 18 months, demonstrated a BMI increase of only 0.17 kg/m2/100 days.Citation11 Their conclusions were that food supplementation did not have a significant impact.Citation11 Similarly, in Uganda, Maina and colleagues found that nine months of food supplementation for chronically sick adults providing 300 g of CSB and 25 g of vitamin A fortified vegetable oil per day (equivalent to 1333 kcal/person/day) led to a weight gain and MUAC increment of only 2.06 kg and 0.99 cm, respectively.Citation16
The three-month intervention providing 500 g/day of CS-RUTF achieved a tenfold greater increase in BMI than the 12 months of nutritional support described by Bowie and colleaguesCitation11 and double the weight and MUAC gains reported after the nine-month intervention in the Uganda study.Citation16 Participants in this present study gained 19.1 g for each 1,000 Kcal of RUTF provided compared to only 5.7 g/1000 Kcal provided in the Uganda study.
The use of high nutrient supplement was necessary as patients enrolled in the present study were severely wasted and needed therapeutic feeding rather than supplementary feeding. Indeed, compared to the normal MUAC, weight, and BMI of rural Malawian of 238 mm, 50.1 kg and 18.8 kg/m2 for male and 266 mm, 48.1 kg and 19.6 kg/m2 for female, some patients have lost up to 20% or more of their weight.Citation17
The high nutrient density, especially the energy density of RUTF, the ease of use of RUTF, and the decreased propensity to share RUTF when compared with traditional aid commodities such as CSB, oil, and sugar, are probably all important factors contributing to the better impact of this study. The energy density of CS-RUTF is ~530 kcal/100 g and the average intake seen here of 300 g of RUTF per day provided 1590 kcal/day. By contrast, the energy density of porridge cooked in villages rarely exceeds 80 kcal/100 ml,Citation18 requiring at least 2.5 liters of a thick porridge to achieve an equivalent energy intake. The low nutrient density of relief foods also precludes diets based on these commodities achieving the nutrient densities recommended by the WHO for the treatment of severe acute malnutrition.Citation19 An additional factor that might have contributed to the better outcome is less sharing of the RUTF than with traditional food-aid commodities. Anthropological studies looking at people’s acceptance of community-based therapeutic care have indicated that RUTF, although shared amongst the family, tends to be better targeted towards the individual undergoing treatment than blended flour.Citation20
Although we do not have pre-intervention data on mortality in PLWHA in the study areas, the observed three-month mortality of 18.3% in the patients included in the program seems relatively low given that 75% of the patients were in stage 4 and had wasting syndrome known to be associated with a median survival of only 9.3 months and 3.4 months, respectively.Citation21–Citation23
Cost effectiveness
The combination of improved energy and nutrient content, increased rates of weight gain, better targeting and shorter duration of treatment has important implications for cost effectiveness. Using the WFP-Malawi costing of $10 per person/month receiving CSB and oil, $40 /household/month for the household food support and $50/MT for operational costs, the monthly cost of the nutrition support was $53.25/targeted patient using the standard food-aid commodities of CSB and oil. In our study the cost of RUTF was $3/kg and $50/MT for operational costs, equivalent to $45.9/month for the 500 g/day ration. The far shorter three-month duration of treatment meant that the total cost of the intervention was $137.7/patient, less than 20% of the cost of the Bangwe program at $629/patient and less than 25% the cost of the intervention in Uganda ($479.25/patient).
An important finding of this study is that two local AIDS support organizations were able to implement this type of intervention with little external support. Our support covered only training of the main supervisors and volunteers, the delivery of CS-RUTF to the main office of NASO and SASO and provision of financial support for drugs, fuel purchase and replenishment of the HBC kits.
Access to ARV services
The positive impact of the intervention on physical activity performance and well being had several important consequences. During the course of the intervention 15 out of 27 HIV untested patients who had been reluctant to consider voluntary counseling and HIV testing (VCT), changed their minds and underwent VCT. The increase in physical activity as a result of treatment also enabled many patients previously too weak to access their nearest clinic to walk to their clinic and qualify for admission into ART programs. This is an important outcome in a country where in 2004 only approximately 17% of young adults had ever undergone HIV testing.Citation24 In Malawi the low uptake of VCT means that in practice most HIV infections remain undiagnosed and are merely suspected on clinical grounds in chronically sick patients. As within developing countries, the time from first AIDS-defining condition to death can be as short as nine months,Citation21–Citation23 this delayed diagnosis means that by the time that HIV is suspected many patients may no longer be able to walk to the nearest VCT centre and cannot therefore be enrolled into an ART program. This represents a barrier to accessing ARVs for a substantial number of adults and starts a vicious cycle wherein the patient is too weak to access appropriate care, becomes weaker and then loses hope. Findings from this study indicate that types of intervention have the potential to substantially increase access and uptake of ARV services.
Study limitations
The observational design and the absence of pre-intervention data for comparison are limitations to the study. Unfortunately, it was impossible to implement interventions that provided different types of nutritional support, as NASO and SASO authorities believed that this would create problems with their beneficiaries. Another limitation of the study is the absence of data on food availability at household level and of dietary intake from other food. This data would have enabled us to control for impact of quality and quantity of household food and consumption of other food on study outcomes. However, as CS-RUTF intake correlated positively with the rate of nutritional recuperation, even after adjusting for potential confounding factors, it is reasonable to propose that a causal link exists between the two. The short time of follow up did not allow us to assess the impact of the early mortality after HAART commencement; a follow up study is going to address this question.
Conclusions
These results were obtained in HBC programs run by local volunteer organizations where, apart from the provision of free RUTF, no additional operational inputs were provided. The study has indicated that nutrition support with CS-RUTF was acceptable to the majority of patients and was associated with an improvement of the nutritional status measured using anthropometric parameters in the majority of HIV-positive patients with WHO clinical stage 3 and 4 disease. The majority of subjects also experienced marked increases in physical capacity and well being that increased both access to and uptake of VCT and ART services. These results were achieved at a substantially reduced cost when compared to usual nutritional support using traditional food-aid commodities. These results suggest that in the context of rural Malawi, the provision of RUTF should be a core component of HBC programs. Further work is required to investigate whether these results can be generalized to other contexts and to confirm that the improvement in weight and physical activity performance correspond to a significant gain in fat free mass.
Acknowledgements
All the authors participated in the design of the study, the interpretation of the data and the writing. The authors would like to acknowledge the invaluable assistance of the Salima AIDS Support Organization and Nkhotakota AIDS Support Organization management and staff and all the program participants and their families. Funding for this work was provided by the Concern Worldwide. All the authors work for Valid International a company sister to Valid Nutrition that promotes local production of Ready To Use Therapeutic Food.
References
- KotlerDPWasting syndrome: nutritional support in HIV infectionAIDS Res Hum Retroviruses1994109319347811545
- WheelerDAWeight loss and disease progression in HIV infectionAIDS Read1999934735312737124
- ZachariahRSpielmannMPHarriesADSalaniponiFMModerate to severe malnutrition in patients with tuberculosis is a risk factor associated with early deathTrans R Soc Trop Med Hyg20029629129412174782
- PatonNSangeethaSEarnestABellamyRThe impact of malnutrition on survival and the CD4 count response in HIV infected patients starting antiretroviral therapyHIV Med20067330332
- van der SandeMASchim van der LoeffMFAveikaAABody mass index at time of HIV diagnosis: a strong and independent predictor of survivalJ Acquir Immune Defic Syndr2004371288129415385737
- ZachariahRFitzgeraldMMassaquoiMRisk factors for high early mortality in patients on antiretroviral treatment in a rural district of MalawiAIDS2006202355236017117022
- WankeCASilvaMGandaARole of acquired immune deficiency syndrome-defining conditions in human immunodeficiency virus-associated wastingClin Infect Dis200337Suppl 2S81S8412942378
- DannhauserAvan StadenAMvan derRENutritional status of HIV-1 seropositive patients in the Free State Province of South Africa: anthropometric and dietary profileEur J Clin Nutr19995316517310201796
- World Health OrganizationConference on Nutrition and HIV/AIDS in Africa: Evidence, lessons and recommendations for action Executive summary of a scientific reviewGenevaWHO2005
- Republic of UgandaNutritional Care and Support for People Living with HIV/AIDS in Uganda: Guidelines for Service ProvidersKampala, UgandaRepublic of Uganda2005
- BowieCKalilaniLMarshRMisiriHClearyPBowieCAn assessment of food supplementation to chronically sick patients receiving home based care in Bangwe, Malawi: a descriptive studyNutr J200541215777483
- NdekhaMJManaryMJAshornPBriendAHome-based therapy with ready-to-use therapeutic food is of benefit to malnourished, HIV-infected Malawian childrenActa Paediatr20059422222515981758
- KarnofskyDABurchenalJHEvaluation of chemotherapeutic agentsYale J Biol Med194922103104
- Who, 2006
- BowieCAlinafeLClearyPBowieCThe pattern of symptoms in patients receiving home based care in Bangwe, Malawi: a descriptive studyBMC Palliat Care20065116472392
- MainaGWGardnerCFMurphyENutrition impact of the Title II feeding program targeting people living with and affected by HIV and AIDS in UgandaDurban, South AfricaHIV/AIDS and Food and Nutrition Security Conference2005
- ZverevYChisiJAnthropometric indices in rural Malawians aged 45–75 yearsAnn Hum Biol200431293714742163
- TrecheSMbomeILViscosity, energy density and osmolality of gruels for infants prepared from locally produced commercial flours in some developing countriesInt J Food Sci Nutr19995011712510616652
- PrudhonCPrinzoZWBriendADaelmansBMMasonJBProceedings of the WHO, UNICEF, and SCN Informal Consultation on Community-Based Management of Severe Malnutrition in ChildrenFood Nutr Bull200627S99S10417076216
- BandaweCKabwaziNCultural and social factors affecting the implementation and success of the Community-Based Therapeutic Care (CTC) approach to treating severe malnutrition in Dowa, MalawiLondonValid International2003
- MorganDMaudeGHMalambaSSHIV-1 disease progression and AIDS-defining disorders in rural UgandaLancet19973502452509242801
- MorganDMalambaSSOremJMayanjaBOkongoMWhitworthJASurvival by AIDS defining condition in rural UgandaSex Transm Infect20007619319710961197
- OkongoMMorganDMayanjaBRossAWhitworthJCauses of death in a rural, population-based human immunodeficiency virus type 1 (HIV-1) natural history cohort in UgandaInt J Epidemiol1998276987029758128
- National Statistical Office, ORC MacroMalawi Demographic and Health Survey 2004Calverton, MarylandNational Statistical Office (Zomba, Malawi)2005