Abstract
Objective
To evaluate the impact of a Pharmaceutical Care service in the identification and resolution of drug-related problems (DRPs) and in quality of life (QoL) of a group of elderly outpatients with chronic health conditions.
Methods
30 outpatients (aged 60–75-years old) were followed between August 2003 and July 2004 at a primary health care unit in Ribeirão Preto (SP), Brazil. Patients were scheduled monthly to meet with the researcher, who provided Pharmaceutical Care service (the intervention). Through Pharmaceutical Care, the pharmacist worked with the patient and other care providers to improve outcomes of drug therapy through focused education, care planning, and monitoring. Intervention outcomes were the number of DRPs prevented or resolved, and the impact on QoL. The Short Form-36 health survey was used to measure changes in QoL.
Results
The mean age of patients was 66 ± 5 years, 21 of whom had low literacy. During the study, 92 DRP were identified, 3.0 ± 1.5 problems per patient. By the end of the study, the interventions solved 69% of actual DRP and prevented 78.5% potential DRP. In addition, QoL showed improvement in 22 patients after DRP resolution or prevention.
Conclusion
Despite the limitations in this study that may affect generalizability of the results, this study demonstrates that humanistic and behavioral interventions based on the Pharmaceutical Care model were capable in reducing DRPs, and improve QoL in patients.
Introduction
In Brazil, the increase in the absolute number of elderly persons with chronic health conditions has been reported to be one of the determining factors in the rise in medication use (CitationRozenfeld 2003). Although there have been no studies about drug-related morbimortality in Brazilian population, drugs have been identified as the first cause of intoxication in this country since 1996 (CitationSINITOX 2002). These data indicated the need to adopt new models of care that prevent drug-related morbimortality, and improve the population’s Quality of Life (QoL).
Globally, there have been significant changes in health care systems in respect of their quality and processes, and this had been specifically demonstrated in the practice of pharmacy. A dramatic shift in the way pharmacy had been practiced was demonstrated in the newly emerging Pharmaceutical Care practice, defined as ‘the responsible provision of drug therapy to achieve definite outcomes that improve a patient’s quality of life’ (CitationHepler and Strand 1990). This definition, which placed QoL in the core of the Pharmaceutical Care philosophy, was subsequently adopted worldwide (CitationKheir et al 2004).
Quality of life is generally considered a multidimensional construct that includes physical, mental, and social functioning, as well as perceptions of general well-being (CitationHays et al 2000). Nowadays, QoL can be measured objectively with questionnaires (instruments) possessing sufficient sensitivity to change, reliability and validity properties (CitationSiedl and Zannon 2004). It has been a fundamental research topic in health, as its results are important to assess the effectiveness of care as well as to obtain social and health funding (CitationOkano et al 2001).
Therefore, the purpose of this study was to evaluate the effect of pharmaceutical interventions in the reduction of drug-related problems (DRP) and improvement of QoL in a group of elderly outpatients with chronic health conditions.
Methods
A prospective study was conducted at a primary health care unit (PHCU) in Ribeirão Preto (SP), Brazil, from August 2003 to July 2004. The site was chosen because 300 of the 1500 patients have hypertension, and the center’s health care providers identified 40% (120) of non-adherence as a primary reason for poor treatment outcomes. At the PHCU, the outpatients were attended by four physicians, two dispensing pharmacists and a researcher pharmacist.
Patients
During a week period, all hypertensive patients who came to the ambulatorial care pharmacy of PHCU to receive their medication were identified as potential candidates for the study. Patients were eligible to participate if they met three or more of the following criteria (CitationKoecheler et al 1989): five or more drugs in their drug therapy regimen, twelve or more doses per day, a medication regimen that had changed four or more times in the past year, three or more co-morbidities, a history of medication non-compliance, and presence of at least one drug that requires therapeutic monitoring (Appendix A). Exclusion criteria were stage 3 hypertension (systolic ≥180 mmHg and/or diastolic pressure ≥110 mmHg based on JNC-VI criteria), an identified secondary cause of hypertension, such as chronic renal disease, renovascular disease, pheochromocytoma, Cushing’s syndrome, and primary aldosteronism; or if the patient missed more than three appointments during the study.
Out of 300 hypertensive patients, 90 eligible patients were invited. Of these, 16 refused to participate, 74 accepted to be included, but 15 were eventually excluded because of their age. From the remaining 59, thirty patients completed the entire study, attending all of the interviews with the researcher and provided complete data. The remaining 29 patients declined to participate or rejected by the research team; and the most common reasons for declining/rejection were lack of time (n = 11), missing more than one scheduled interview (n = 10), patient’s lack of belief in any health-related added value in the study (n = 6), and patient moved out of the area (n = 2). The nature of the study was explained to the patients, and an informed consent forms were signed by those eligible and interested in participating.
Pharmaceutical Care program
Patients were scheduled to see the pharmacist at least once every month at the PHCU for a year. Following a structured pharmaceutical care methodology, the pharmacist conducted interviews lasting from 30 to 40 minutes, and addressed a number of issues (from socio-demographic variables collected at the initial interview, to medical and drug history, identification of problems and needs, assessment, and care planning) (CitationCurrie et al 2003). The aim for the provision of Pharmaceutical Care was to provide individualized care tailored to the health needs of the patient in order to improve therapy outcomes, with special emphasis on quality of life (QoL). The two major areas addressed through the process were health education and drug therapy (CitationLyra et al 2005). The process aimed at achieving personal transformation through focusing into three key consciousness-raising experiences: relating and reflecting on experience; exploration and problem solving; and taking thoughtful action. These steps provide a framework for Freire’s participatory social orientation approach to the design of effective educational strategies in health. While originally applied to the teaching of basic literacy skills to adults in Brazil, it has been used internationally in health education (CitationRoter 2001; CitationFreire 1983; CitationRoter 2000).
The educational part of the intervention consisted of: orientation concerning chronic health conditions (nature, causes and treatment) and changes in lifestyle, the recognition of signs and symptoms caused by medication (effectiveness and safety) and the encouragement of patients to participate actively in designing his/her drug therapy regimen.
The pharmacist evaluated patients individually to identify actual and potential DRPs, which were categorized in terms of need, effectiveness and safety (Comité de Consenso 2002 – Appendix). All the information was recorded in dedicated database that was updated monthly. Drug therapy interventions also consisted of: assessment of drug history (current and past medication history, need for drug therapy, compliance with drug therapy), identification, prevention, and resolution of DRPs (actual and potentials), use and storage of medicines (prescription, over-the-counter (OTC), and herbal drugs), and the level and ability for the implementation of adherence-improving strategies.
Evaluation of QoL
In this study, the Medical Outcomes Study Short Form 36 (SF-36®) – a well established generic health status questionnaire- was chosen because of its applicability to a variety of disease sates, ease of administration, international application and documented validity (CitationWare and Sherbourne 1992).
The SF-36 version that was used in the current study had been adapted and validated for Brazilian-Portuguese (CitationCiconelli et al 1999). The SF-36 contains 36 multiple choice questions distributed in eight domains, each of which evaluates one of the following characteristics: functional ability (10 items), physical appearance (4 items), pain (2 items), global health state (5 items), vitality (4 items), social situation (2 items), emotional status (3 items) and mental health (5 items). Each domain was transformed to a scale ranging from 0 to 100, in which the highest score represented the best QoL level. For each unanswered domain, the average value of the other items in the same domain was considered. The SF-36 was administrated to patients at baseline (first interview) and at the end of the study (12-months). The pharmacist researcher was trained to apply the SF-36 instrument.
Statistical analysis
The paired t test was used to measure differences in DRP and QoL between baseline (August 2003) and the end (July 2004) of this study. A difference of 5 points in changed SF-36 domain scores was considered clinically meaningful (CitationWare et al 1995). All analyses used SPSS (version 12, SPSS Inc., Chicago, IL). A significance level of 0.05 was adopted for all statistical tests. All results were validated by means of Wilcoxon’s Rank-sum test.
Results
Socio-demographic and health situation profile
The mean age of patients was 66 ± 5-years, 20 of whom were women (n = 30). 21 (71%) of the interviewees reported low literacy. In Brazil, literate is a person who can both read and write at least a simple statement in a language he or she knows (language – Portuguese) (CitationUNESCO 2006). There was a predominance of retirees/pensioners and housewives (63% and 27% respectively). The mean number of chronic health conditions per elderly individual corresponded to 3.5 ± 1.5. In this study, 17 (56.5%) of the patients reported hypertension, diabetes mellitus and hyperlipidemia diagnosed more than 10-years before. Due to various morbidities, each patient had an average of five physicians’ appointments with different specialists per year.
Drug therapy profile
During the study period, 250 different medicines were used (mean 8.5 ± 4 drugs per patient), and the majority (81%) were prescribed by a physician. Twenty patients were taking more than five different drugs at the same time.
Evaluation of Pharmaceutical Care interventions
In this study, 590 interventions were performed and documented. Of these, 214 were concerned drug therapy and 376 involved provision of education ( and ). These interventions were equally distributed among the different chronic health conditions that the patients suffered.
Table 1 Quantitative distribution of the drug therapy interventions, Ribeirão Preto, 2004
Table 2 Quantitative distribution of the drug therapy interventions, Ribeirão Preto, 2004
Ninety two DRPs were identified during the study, averaging 3.0 ± 1.5 problems per patient. There was higher incidence of problems in the of the Safety category (64%), mainly in drug classes such as: diuretics (12 [19%]), analgesics (10 [16%]), calcium channel blockers (9 [14%]) and angiotensin-converting-enzyme (ACE) inhibitors (8 [13%]).
Twenty one patients showed a mean of 2.6 actual DRP and 0.5 potential DRP. 65% of 214 drug therapy interventions required a physician’s approval or agreement. The physicians agreed to change 86% of drug therapy regimen. By the end of the study, the interventions resolved 69% of actual DRPs and prevented 78% potential DRPs. The results demonstrated an average of 4 ± 2 Pharmaceutical Care interviews to identify and solve DRPs. All of the health education interventions that were made were accepted by the patients and implemented by them.
Some actual and potential DRP remained unresolved or were not prevented. The resolution and prevention of these DRP required modifications in drug regimens that relied exclusively on a medical decision.
Details involving socio-demographic profile and the evaluation of Pharmaceutical Care interventions are well described in a previous publication (CitationIV DBHA 2002).
Analysis of QoL
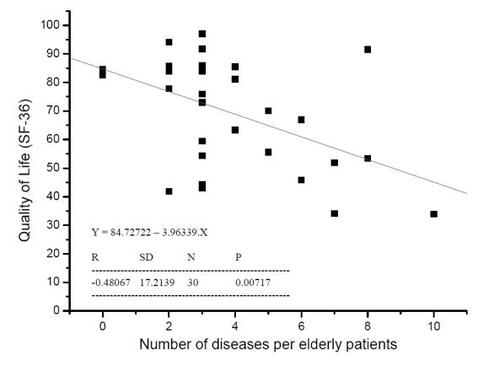
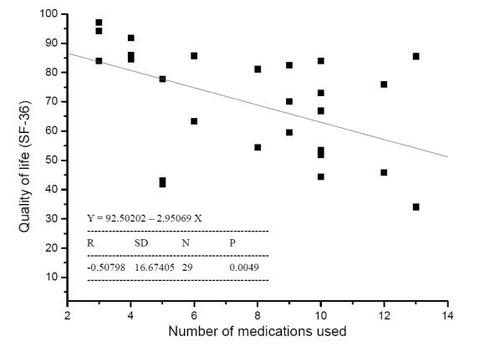
At baseline of this study, there was a trend for poor QoL in patients who had more diseases and used more medications ( and , respectively).
At the end of the study, the statistically significant difference were found in SF-36 domains (p < 0.05) of physical aspects, pain, general health status, vitality, social and emotional aspects after interventions (). Score in mental health domain also was higher but did not achieve statistical significance (p = 0.05).
Table 3 QoL scores before and after the intervention asassessed by the SF-36, Ribeirão Preto, 2004
The results of changes in QoL were evaluated and compared with number of interventions made and DRPs resolved or prevented (). Twenty two patients presented with mean change in QoL score of >5 units after DRP resolution or prevention. There was a proportional converse relationship between QoL and the number of DRPs, after the interventions. See .
Figure 3 Correlation between the number of drug-related problems (DRP) resolved or prevented and quality of life.
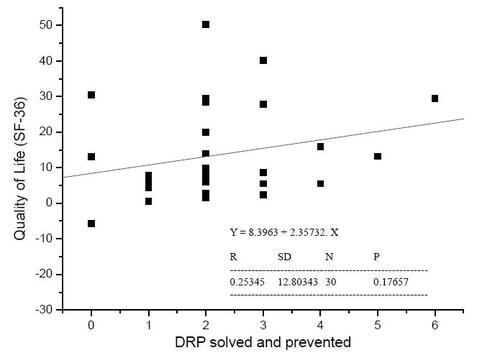
Table 4 Drug-related problems and QoL before and after the intervention per individual patient
Discussion
This study provided evidence for the benefits of a patient-focused role of the pharmacist in identifying and resolving drug-related problems in the patient population studied.
The large number of medications taken and the occurrence of problems associated to these drugs suggested that medications are potential harmful agents to the health of the elderly population and that they can cause an array of symptoms ranging from orthostatic hypotension and gastritis to dizziness and muscle cramps. These symptoms necessitated the withdrawal of the drug in many cases. However, collaborative work between the pharmacist and physicians was successful in making tangible changes in the drug regimens and introduced simple therapeutic regimens tailored to the needs and circumstances of the individual patient. The co-operation between the pharmacist and the clinician also was key to resolving and/or preventing DRPs in PHCU. Other studies showed positive results of interventions that lead to the resolution and prevention of DRPs, reduction of treatment costs and overall satisfaction with pharmaceutical care program (CitationMehos et al 2000; CitationBernsten et al 2001; CitationGeber et al 2002; CitationVivian 2002).
Most of the patients in this study had low literacy rates. In Brazil, individuals with reduced education levels are approximately 5 times as likely to have health problems (CitationRosa et al 2003). In this situation, the educational interventions could contribute to awareness development and to the exchange of experiences. This would also be expected to introduce or improve a process of humanization, replacing the dominant formal practices that kept the patients at a comfortable distance and separated them form reality. Empowering patients through more involvement in their care builds their confidence and helps in a process of personal transformation and realization of a state of ‘critical consciousness’ (CitationRoter et al 2001).
The predominance of retirees/pensioners and housewives was high is this sample. According to Rosa et al, retirees and housewives are almost 8 times as likely to present with morbidities (CitationRosa et al 2003). In our study, patients presented with at least two concurrent chronic health conditions; as a consequence they had to be treated by different specialist physicians, which needed polypharmacy and subsequently created the need for comprehension about complex drug therapy regimen. In the literature, it has been demonstrated that the number of drugs prescribed increases with the number of physicians seen (CitationRollason and Vogt 2003). In the USA, for example, 43% of the patients use medication prescribed by more than two physicians, which increases the risk of redundancy and drug interaction (CitationSteinbrook 2002).
The high level of medication consumed and the occurrence of an associated high incidence of DRPs suggested that the medications were potential harmful agents to the health of the elderly population and that they can cause an array of symptoms ranging from orthostatic hypotension and gastritis to dizziness and muscle cramps. These symptoms necessitated the withdrawal of the drug in many circumstances. However, collaborative work between the pharmacist and physicians succeeded in making tangible changes in drug regimens and introduced simple therapeutic regimens tailored to the needs and circumstances of the individual patient. The co-operation between the pharmacist and the clinician also was key to resolving and/or preventing DRPs in PHCU. Other studies showed positive results of interventions that lead to the resolution and prevention of DRPs, reduction of treatment costs and overall satisfaction with pharmaceutical care program (CitationMehos et al 2000; CitationBernsten et al 2001; CitationGeber et al 2002; CitationVivian 2002).
Generic instruments, such as the SF-36, can accurately assess all significant health aspects and reflect the impact of a disease on an individual (CitationFayers 2000). These types of instruments have been used to study groups of patients with different diseases, ambulatory populations, and populations with chronic health conditions.
The findings obtained in baseline of our study suggest an inverse relationship between the number of health conditions suffered by the patient and QoL. It also provides evidence of an inverse relationship between QoL and the number of medications taken at the same time by the patient. These are important findings because often the goal of therapy is to improve QoL, as was indeed the cases in several other studies which reported QoL improvements as a result of the introduction of drug therapy, for example in patients with asthma (CitationKheir 2001), diabetes (CitationCranor and Christensen 2003) and migraine (CitationAlsuwaidan 1998). In our case, it seems polypharmacy might be the culprit, especially when there is involvement of prescription ands non-prescription drugs.
One of the important aspects of using QoL instruments in intervention studies is the measurement properties of the questionnaire used. In case of the Sf-36, patients are not shown their first visit’s scores at the second data collection visit. This is not a requirement when completing the SF-36 (while it is required in some other QoL instruments like the Asthma Quality of Life Questionnaire, where it is assumed that informing patients of their previous health status, subjectively assessed, would improve the instrument’s sensitivity). However, showing the patients their previous scores would have violated the structured method by which the SF-36 is used. Issues regarding sensitivity to change of the SF-36 are discussed below.
In this study, there was a trend for QoL to decline in 7 domains over time. However, functional capacity was the only domain that remained stable, probably due to the physical decline that is characteristic of aging, associated with multiple biopsychosocial aspects that were present in our population of patients. Other studies showed positive outcomes for functional capacity, although the differences had been insignificant after 6-months of follow-up (CitationCarter et al 1997; CitationBernsten et al 2001; CitationOkamoto and Nakahiro 2001). In the elderly, QoL is understood in terms of health and functional capacity and often associated with the degree of personal dependence and autonomy (the ability for self rule). This dependence can result from biological transformations (into disability) as it can from social transformation. Consequently, this subject should not only be linked to health promotion, but also to the persons’ social and cultural contexts (CitationCuellar and Fitzsimmons 2003). Actually, this emphasizes the humanistic nature and relevance of QoL and suggests the need for a form of pharmaceutical practice that is humane as much as it is professional.
Malone and colleagues affirmed that the SF-36 may not be sensitive enough to detect more changes in QoL that are attributable to pharmacist interventions (CitationMalone et al 2001). Most of studies carried out in community pharmacies and hospital outpatient clinics in the USA and Europe which only applied the SF-36 did not demonstrate statically significant effects on elderly QoL (CitationBillups et al 2000; CitationBernsten et al 2001; CitationMalone et al 2001; CitationVolume et al 2001). Otherwise, studies without a control group demonstrated that pharmacist interventions obtained positive results on one or more domains of QoL when compared with research with a control group, although the difference had not been statistically significant (CitationPickard and Hung 2006).
According to the literature, the nature of interventions could be an important aspect for the failure in obtaining positive outcomes for QoL (CitationKheir et al 2001; CitationMelchiors 2005). Traditional approaches to teaching, in which patients are treated as passive and dependent objects, reinforce powerlessness and helplessness (CitationRoter et al 2001). Moreover, traditional and purely pharmacological interventions can be very invasive in order to produce effective changes in QoL domains and to be detected by not very sensitive instruments (CitationKheir et al 2004). Adults, mainly elderly with low literacy, need a different approach to engage with the interventions. In comparison, Pharmaceutical Care is basically a behavioral intervention that may achieve positive outcomes, with subtle changes in QoL domains 4. Actually, interventions aimed at influencing behavior and awareness requires construction of therapeutic relationship, self-directed orientation, patient-centeredness, valorization of life experience, recognition of social roles, long periods of follow-up with a view to obtaining significant and measurable changes (CitationRoter 2000; CitationGrueninger 1995). Therefore, the interventions based on awareness-raising in this study were probably responsible for the positive outcomes in terms of elderly QoL.
Limitations
The limitation of this study could be summarized as follows: the researcher’s experience in pharmaceutical care, sample size, ability of researcher to apply SF-36 and program conducted in only one setting.
The researcher’s lack of experience in pharmaceutical care (a relatively new practice in the filed of pharmacy) may have prevented the detection of more DRPs. These undetected DRPs may have negatively impacted on the patients’ QoL hence affecting the degree of improvement resulting from the intervention. Other studies demonstrated that the major difficulty to improve QoL in the elderly was because of the variations in pharmacists’ education (CitationBillups et al 2000; CitationMalone et al 2001; CitationGarção et al Cabrita 2002). Therefore, a longer training period for the researcher might have produced better results.
Although the SF-36 has been frequently used in pharmaceutical care research, there is very little evidence to suggest improvement in QoL (measured by this generic instrument) after pharmaceutical care interventions (CitationBillups et al 2000; CitationOkano et al 2001; Schultz 2001; CitationVivian 2002). Several studies have supported the notion that existing generic QoL instruments may lack the specificity and sensitivity required to express changes as a result of Pharmaceutical Care interventions (CitationBillups et al 2000; CitationMalone et al 2001; CitationKheir et al 2004). The absence of a QoL instrument specifically designed for use in Pharmaceutical Care could be a possible reason for the difficulty in detecting improvement in QoL domains as a result of pharmaceutical care interventions (CitationKheir et al 2004). The development of a specific instrument to measure the impact of pharmaceutical care on QoL may optimize the assessment of intervention outcomes, if sufficiently sensible to detect truly positive outcomes (Schultz 2001; CitationPickard and Hung 2006).
The SF-36 is a self-completed instrument, but it was administrated by the researcher because of the low literacy of patients. The researcher’s lack of experience to apply the SF-36 might have influenced in results. The literature emphasize that pharmacists’ inability to apply the instrument might cause to negative results in QoL (CitationBentley et al 1998; CitationKheir et al 2004).
The small sample size (30 patients) allowed us to detect significant final differences in DRPs and QoL results. However, several studies demonstrated that the small samples used in ambulatory settings and community pharmacy studies were associated with poor or insignificant QoL outcomes (CitationCarter et al 1997; CitationMehos et al 2000; CitationVivian 2002; CitationPickard and Hung 2006). Thus, for generalizability of results, larger size samples would naturally be needed.
Because this study was conducted in only one setting, our results may not be extrapolated to populations in Brazil or elsewhere.
Conclusion
Study participants were largely of low literacy, with high prevalence of chronic health conditions and high medication consumption. Inadequate drug therapy led to various DRPs, particularly related to the safety domain, which caused other health problems. Despite the limitations that may have affected the ability to generalize the results, this study demonstrates that the humanistic and behavioral interventions based on the Pharmaceutical Care model have the ability to reduce DRPs, and improve the QoL of elderly outpatients.
The researcher pharmacist did not discuss with the patients on the answers of the SF-36 in the base line. Therefore, the first results had not influenced the effect of the PCP when the questionnaire was repeated 12-months later.
Acknowledgements
The authors wish to thank all the patients who participated in this study. The authors also acknowledge the valuable comments of Adriano Araújo, Fernanda Gimenes and Tatiane Marques.
Financial support
This study was supported by CAPES and FAPESP.
Possible conflict of interest
There are none.
References
- AlsuwaidanSMaloneDCBillupsSJCharacteristics of ambulatory care clinics and pharmacists in Veteran Affairs medical centersAm J Health-Syst Pharm19985568729437478
- BentleyJPSmithMCBanahanBF3Quality of life assessment by community pharmacists: an exploratory studyQual Life Res19987175869523499
- BernstenCBjörkmanICaramonaMImproving the well-being of elderly patients via community pharmacy-based provision of pharmaceutical careDrugs and Aging200118637711232739
- BillupsSJMaloneDCCarterBLRelationship between drug therapy noncompliance and patient characteristics, health-related quality of life, and health care costsPharmacotherapy200020941910939555
- CarterBLBarnetteJChrichilesEEvaluation of hypertensive patients after care provided by community pharmacists in a rural settingPharmacotherapy1997171274859399611
- CiconelliRMFerrazMBSantosWBrazilian-Portuguese version of SF-36. A reliable and valid quality of life outcome measureRev Bras Reumatol19993913950
- COMITÉ DE CONSENSOSegundo Consenso de Granada sobre Problemas Relacionados con MedicamentosArs Pharmaceutica20024317584
- CranorCWChristensenDBThe Asheville Project: short-term outcomes of a community pharmacy diabetes care programJ Am Pharm Assoc20034314959
- CuellarLMFitzsimmonsDSRaising pharmacists’ cultural awarenessAm J Health-Syst Pharm200360285612613240
- CurrieJDDoucetteWRKuhleJIdentification of essentials elements in the documentation of pharmacist-provided careJ Am Pharm Assoc200343419
- FayersPMDQuality of lifeAssessment, analysis and interpretation2000ChichesterJonh Wiley
- FreirePEducation for critical consciousness1983New YorkContinuum Press
- GarçãoJACabritaJEvaluation of a pharmaceutical care program for hypertensive patients in rural PortugalJ Am Pharm Assoc20024285864
- GeberJParraDBeckeyNPOptimizing drug therapy in patients with cardiovascular disease: the impact of pharmacist-managed pharmacotherapy clinics in a primary care settingMedscape2002
- GrueningerUJArterial hypertension: lessons from patient educationPatient Education and Counseling19952637557494753
- HaysRDMoralesLSReiseSPItem response theory and health outcomes measurement in the 21st centuryMed Care200038II284210982088
- HeplerCDStrandLMOportunities and responsabilities in pharmaceutical careAm J Hosp Pharm199047533452316538
- IVDBHADiretrizes Brasileiras de Hipertensão ArterialSão Paulo (SP): SBH/SBC/SBN200240
- KheirNEmmertonLShawJCan pharmacists influence the health-related quality of life of patients with asthma? The New Zealand Pharmaceutical Care experienceSqu Journal for Scientific Research: Medical Sciences200136975
- KheirNMVan MilFShawJPHealth-related quality of life measurement in pharmaceutical care: targeting an outcome that mattersPharm World Sci200426125815230357
- KoechelerJAAbramowitzPWSwimSEIndicators for the selection of ambulatory patients who warrant pharmacist monitoringAm J Health-Syst Pharm198954180515
- LyraDPJrAmaralRTAbriataJPSatisfaction as an outcome of a pharmaceutical care program for elderly in Ribeirão Preto – São Paulo (Brazil)Seguimiento Farmacoterapéutico200533042
- MaloneDCCarterBLBillupsSJCan clinical pharmacists affect SF-36 scores in veterans at high risk for medication-related problems?Med Care2001391132211176549
- MehosBMSaseenJJMac laughlinEJEffect of pharmacist intervention and initiation of home blood pressure monitoring in patients with uncontrolled hypertensionPharmacotherapy2000111384911079287
- MelchiorsACCorrerCJRossignoliPHumanistic-outcomes questionnaires in diabetes research and practiceAm J Health Syst Pharm200562354515745883
- OkamotoMPNakahiroRKPharmacoeconomic evaluation of a pharmacist-managed hypertension clinicPharmacotherapy20012113374411714206
- OkanoGJMaloneDBillupsSJReduced quality of life in Veterans at risk for drug-related problemsPharmacotherapy2001211123911560202
- PickardASHungSYAn update on evidence of clinical pharmacy services’ impact on health-related quality of lifeThe Annals of Pharmacotherapy20064016233416912249
- RollasonVVogtNReduction of polypharmacy in the elderly: a systematic review of the role of the pharmacistDrugs and Aging2003208173212964888
- RosaTECBenícioMHDLatorreMRDODeterminant factors of functional status among the elderlyRev Saúde Públ200337404
- RoterDLMargalit-StashefskyRRuddRCurrent perspectives on patient education in the USPat Educ Couns2001447986
- RoterDLThe medical visit context of treatment decisionmaking and the therapeutic relationshipHealth Expect20003172511281908
- RozenfeldSPrevalence, associated factors, and misuse of medication in the elderly: a reviewCad Saúde Públ20031971724
- SchultzMApplying health status instruments in pharmaceutical care researchProceedings of the 2nd International Working Conference on Quality Issues in Pharmaceutical Care ResearchJanuary 2001Hillerod, Denmark
- SiedlEMFZannonCLMCQuality life and health conceptual and methodological issuesCad Saúde Públ2004205808
- [SINITOX] Sistema Nacional de Informações Tóxico-FarmacológicasEstatística anual de casos de intoxicação e envenenamento: Brasil, 2001Rio de Janeiro: Fundação Oswaldo Cruz/Centro de Informações Científica e Tecnológica200240
- SteinbrookRThe prescription-drug problemN Engl J Med200234679011893789
- UNESCO Institute for Statistics (UIS). Literacy and Non Formal Education Section2006 URL: http://www.uis.unesco.org/TEMPLATE/html/Exceltables/education/MetadataLiteracy_CurrentRel.xl
- VivianEMImproving pressure control in a pharmacist-managed hypertension clinicPharmacotherapy20021215334012495164
- VolumeCIFarrisKBKassamRPharmaceutical care research and education project: patient outcomesJ Am Pharm Assoc20014141120
- WareJEKosinskiMKellerSDSF-12: how to score the SF-12 physical and mental health summary scales1995BostonHealth Institute, New England Medical Center
- WareJESherbourneCDThe MOS Item Short-form Health Survey (SF-36). Conceptual framework and item selectionMed Care199230473831593914
Appendix A
Classification of drug-related problems, according to the Consensus of Granada (2002)